Published online Dec 28, 2018. doi: 10.4329/wjr.v10.i12.184
Peer-review started: June 5, 2018
First decision: July 27, 2018
Revised: September 17, 2018
Accepted: November 24, 2018
Article in press: November 24, 2018
Published online: December 28, 2018
To investigate the hemothorax size for which tube thoracostomy is necessary.
Over a 5-year period, we included all patients who were admitted with blunt chest trauma to our level 1 trauma center. Focus was placed on identifying the hemothorax size requiring tube thoracostomy.
A total number of 274 hemothoraces were studied. All patients with hemothoraces measuring above 3 cm received a chest tube. The 50% predicted probability of tube thoracostomy was 2 cm. Pneumothorax was associated with odds of receiving tube thoracostomy for hemothoraces below 2 cm (Odds Ratio: 4.967, 95%CI: 2.225-11.097, P < 0.0001).
All patients with a hemothorax size greater than 3% underwent tube thoracostomy. Prospective studies are warranted to elucidate the clinical outcome of patients with smaller hemothoraces.
Core tip: There is no clear recommendation for tube thoracostomy in hemothorax management based on computed tomography scan measurements. In this study, we found that any hemothoraces above the cut-off size of 3 cm should be drained using tube thoracostomy. Smaller hemothoraces may warrant drainage based on other findings such as presence of pneumothorax.
- Citation: Malekpour M, Widom K, Dove J, Blansfield J, Shabahang M, Torres D, Wild JL. Management of computed tomography scan detected hemothorax in blunt chest trauma: What computed tomography scan measurements say? World J Radiol 2018; 10(12): 184-189
- URL: https://www.wjgnet.com/1949-8470/full/v10/i12/184.htm
- DOI: https://dx.doi.org/10.4329/wjr.v10.i12.184
Blunt chest trauma is commonly encountered in the emergency department as an individual presentation or part of the clinical scenario of a trauma patient[1]. According to the 2012 National Trauma Data Bank (NTDB) Research Data Set, 738396 patients with available Abbreviated Injury Scale were admitted nationwide. Patients with chest trauma constituted 87387 (11.8%) of the registered patients among which, 73809 (84.5% of chest trauma patients) had blunt chest trauma and 12200 (16.5% of blunt chest trauma patients) had hemothorax (Committee on Trauma, American College of Surgeons. NTDB 2012. Chicago, IL).
Although hemothorax is managed by tube thoracostomy in hemodynamically unstable and critical patients after initial chest/pelvic x-ray and focused assessment with sonography in trauma (FAST), virtually all stable blunt trauma patients undergo chest computed tomography (CT) scan as part of their trauma workup[2]. This is partially due to higher sensitivity of chest CT imaging in detecting pneumothorax, hemothorax and pulmonary contusions along with suboptimal imaging preparation and positioning for supine chest radiography in the acute setting[3]. Tube thoracostomy is an invasive procedure which can lead to immediate procedural injuries, infections, and pain, which can contribute to respiratory failure in patients with chest wall injury. Patients with hemothoraces managed without chest tube can lead to infections and trapped lung. Therefore, it is clinically important to know which patients should receive a chest tube.
At the advent of helical CT scanning, chest CT scan was reserved for cases where chest radiography had uncertain and equivocal results. Hence, up to 30% of blunt trauma patients had their hemothoraces identified on chest CT images, which were not readily identifiable on plain chest X-rays, a.k.a. occult hemothorax[4-6]. Thanks to fairly universal application of chest CT in assessment of blunt chest trauma patients, “occult hemothorax” is not practically occult anymore. In fact, the previously published research papers on occult hemothorax have included hemothoraces that are undoubtedly within the identification range of chest radiography[6,7]. In addition, these studies have included extrapolations from plain radiography studies as their cutoff value, primarily due to the absence of existing studies focusing on chest CT measurements[6-9].
In this study, we investigated the association between the measured size of hemothoraces on chest CT images and the likelihood of tube thoracostomy in an attempt to identify a CT scan-based cutoff value of chest tube placement in blunt chest trauma patients.
Following the approval of the Institutional Review Board of Geisinger Medical Center, we retrospectively studied all patients with the diagnosis of hemothorax and blunt chest trauma that were admitted to our level I trauma center from the beginning of September 2009 to the end of August 2014. Excluded patients were those who were admitted after 24 h from the traumatic accident, patients who were admitted with a chest tube in place, those with chest tube placement before CT scan imaging, patients with chronic hemothorax and those with known pleural diseases. The decision to place a chest tube was based on the clinical judgement of the trauma surgeon for each individual case.
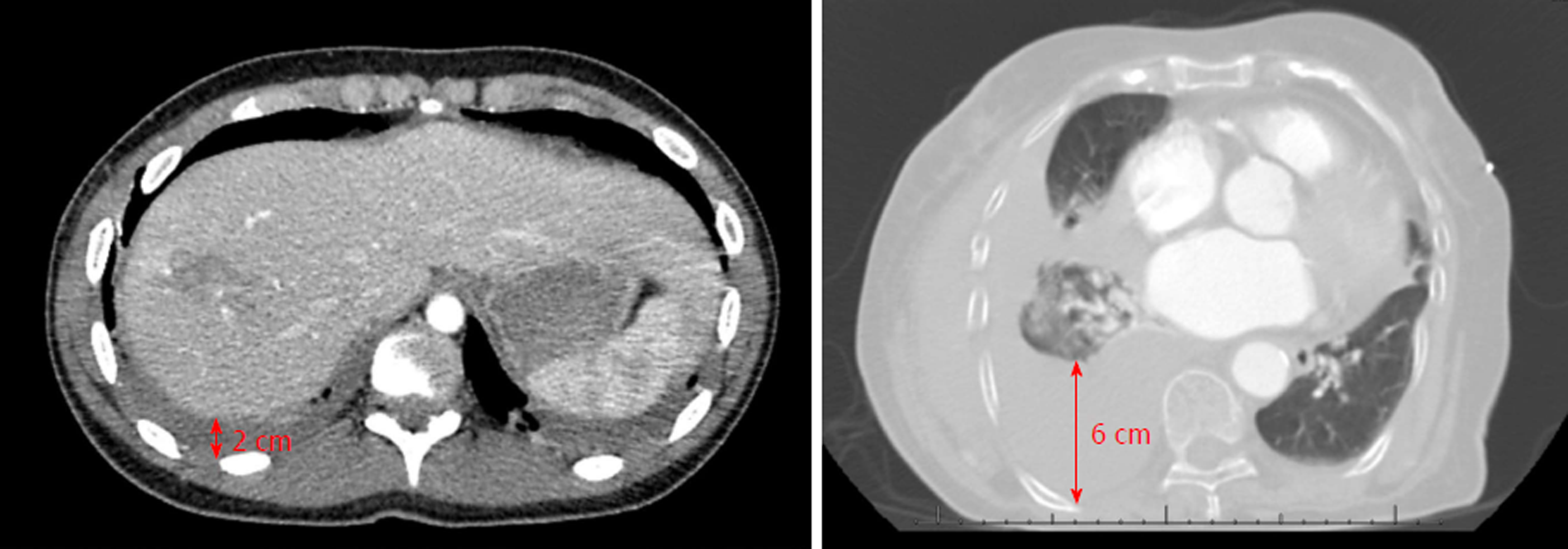
We extracted demographic and clinical data including age, sex, Injury Severity Score (ISS), mechanism of injury, Glasgow Coma Score (GCS), pneumothorax, number of rib fractures, pulmonary contusion and aortic injury. These variables were used in multivariate analysis. Hemothorax was measured as the size (centimeters) of the deepest lamellar fluid stripe in the dependent pleural gutter on axial CT scan images (Figure 1).
Continuous variables were expressed as means ± SD. Non-parametric continuous data were expressed as median with inter-quartile range. Categorical data were expressed as frequencies (%). Logistic regression was used to analyze the predicted probability for tube thoracostomy. Logistic regression with stepwise selection was used to identify variables that increased the chance of tube thoracostomy. SAS 9.4 (SAS Institute, Cary NC) was used for statistical analyses and P < 0.05 was considered significant.
Over the 5-year study period, 271 patients were admitted with the diagnosis of hemothorax and blunt chest trauma. Forty-three patients were excluded and the analysis was performed on the remaining 228 patients. A total number 274 hemothoraces were included from 150 males and 78 females. Table 1 summarized the demographic data and the clinical findings of our patients. The mechanism of injury was predominantly fall (41%) and motor vehicle crash (38%). Patients had a mean ISS of 20 ± 11. Most patients (86%) had a mild GCS (13-15). The median number of rib fractures was 5 (3, 8) and pneumothorax was identified in 128 (56%) patients.
| Variable | n (%) |
| Age (yr), (mean ± SD) | 60.8 ± 19.5 |
| Gender | |
| Female | 78 (34) |
| Male | 150 (66) |
| Mechanism of injury | |
| Fall | 93 (41) |
| MCC | 25 (11) |
| MVC | 86 (38) |
| Other | 21 (9) |
| Pedestrian struck | 3 (1) |
| ISS (mean ± SD) | 20 ± 11 |
| GCS | |
| Severe | 25 (11) |
| Moderate | 6 (3) |
| Mild | 197 (86) |
| Associated pneumothorax | 128 (56) |
| Number of rib fractures, median (IQR) | 5 (3, 8) |
| Pulmonary contusion | 112 (49) |
| Aortic injuries | 7 (3) |
| Size (cm) , median (IQR) | 1.4 (0.9, 2.4) |
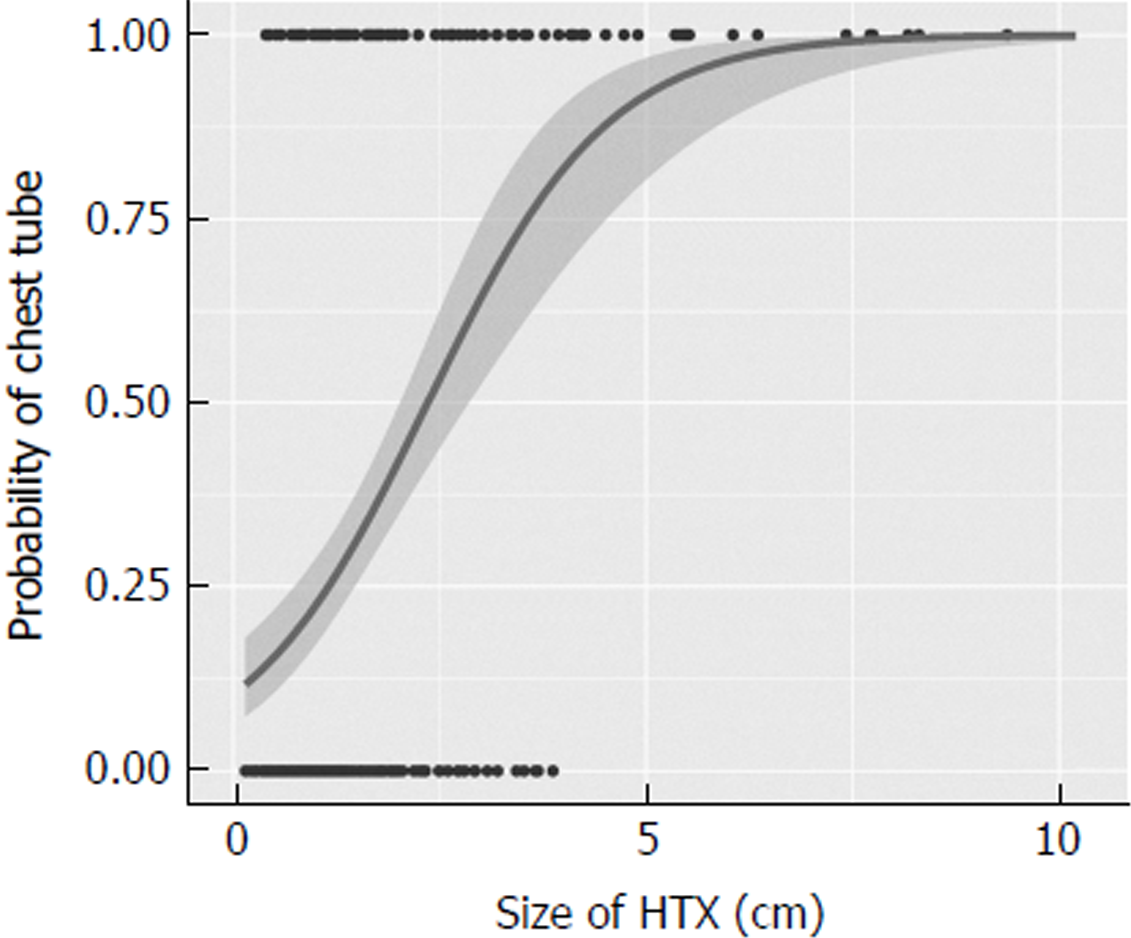
The median size of hemothorax was 1.4 cm (0.9, 2.4). As shown in Figure 2, using logistic regression, we plotted the chest tube insertion versus the measured size in the predicted probability graph. All patients with hemothoraces measuring above 3 cm underwent tube thoracostomy. We found that the probability of receiving a chest tube was more than 50% when the hemothorax measured more than 2.05 cm.
Logistic regression with stepwise selection was used to identify variables associated with odds of receiving a chest tube for hemothoraces < 2 cm. As table 2 summarizes, ISS and associated pneumothorax were associated with significantly higher odds of tube thoracostomy (P = 0.004 and P < 0.0001, respectively). In the 2-3 cm hemothorax range, between 14 patients who underwent tube thoracostomy, pneumothorax was not identified in two (14%). In the same hemothorax range, 15 patients did not receive a chest tube with pneumothorax absent in six (40%). In the remaining 9 patients (60%), pneumothoraces were radiographically identified as compromising less than 5% of the volume of the ipsilateral hemothorax.
We have reported the first study investigating the likelihood of tube thoracostomy based on the measurement of hemothoraces in chest CT scans of blunt chest trauma patients. We found that tube thoracostomy was performed in all patients with hemothoraces measuring more than 3 cm. We also found that the chance of tube thoracostomy was above 50% in patients with hemothoraces measuring above 2 cm; with pneumothorax significantly influencing the decision making. Although a few studies have investigated management of occult hemothorax and included the size in their analyses[6,7,10], they are primarily limited in founding their criteria on extrapolations of chest radiography measurements[8,9], which would highlight why our study was necessary.
The first study directly investigating chest tube placement in management of occult hemothorax was published in 2005 by Bilello et al[6] As the investigators stated, measurements and the 1.5 cm cutoff was set by extrapolation of pleural fluid measurements in chest radiography. Nearly half of the hemothoraces in this study were classified as moderate/large, which by definition, should have been identified in chest radiography and not be included in the study. The following year, another study was published by Stafford et al[10] on the incidence and management of occult hemothorax. In this study, the mean measurement of hemothorax in patients receiving chest tubes was close to 2 cm. More recently, the prospective study by Mahmood et al[7] in 2011 also reported 18% of the patients (the comparison group) to have measurements above 1.5 cm.
This discrepancy might be stemming from difficulty of extrapolation of chest radiography measurements into chest CT scan measurements. Some of the earlier chest X-ray measurements were based on lateral decubitus measurements rather than decubitus images[11]. In addition, chest X-ray fluid measurements propose a range of volumes rather than an exact number[8]. The need to have CT scan-based recommendations is also stemming from clinicians’ inclination towards chest CT scan rather than relying on chest X-ray images. This inclination is scientifically supported by a very recent study showing that up to 71% of patients with blunt chest injury have some or all injuries identified only on chest CT scans[12]. This shows why there was a need for a study based on CT scan measurements alone.
Based on aforementioned literature, the term “occult hemothorax” might not be a clinically applicable name as almost all patients with blunt chest trauma would undergo chest CT scan, which is capable of picking smallest effusions. Hence, the term “small hemothorax” would better delineate the clinical picture as “overt hemothorax” (i.e., large hemothoraces that are identified readily with FAST or chest X-ray) is the only practically true clinical entity that would undergo tube thoracostomy before chest CT imaging.
Our studied population is rather comparable to previously studied patients. In the Bilello et al[6] study, 78 patients with an average ISS close to 25 were included. Less than 40% of patients required tube thoracostomy[6]. The study of Stafford et al[10] included 88 patients with an average ISS of 20. Chest tubes were required in 48% of patients[10]. Lastly, the prospective study by Mahmood et al[7] included 81 patients with an average ISS of 18. Tube thoracostomy was required in only 17% of patients, which is probably reflecting the better job of a prospective study to include patients with smaller hemothoraces. Our study is thus far the largest study that includes 274 hemothoraces from 228 patients.
This study was limited by the operator-based measurements of hemothoraces. Availability or design of a computerized program to measure hemothorax would potentially eliminate this bias. Another limitation was stemming from the radiographic appearance of hemothorax, which does not always form a complete crescentic shape in trauma. Therefore, it is not always easy to define the deepest lamellar fluid stripe. A program that can measure the volume of the hemothorax rather than one single measurement of the thickness would overcome this limitation. Volumetric measurements have been used in other areas of medicine and would be a reachable goal in hemothorax studies[13,14]. Finally, our study was limited by the absence of tube thoracostomy criteria in small hemothoraces. Although the study was performed in a level I trauma center with well-trained trauma surgeons, the final decision of tube thoracostomy was made by the clinical judgement of the trauma surgeon. By expanding the study period over 5 years and including all patients, we tried to partially overcome this limitation. A prospective study including multiple centers with defined criteria for tube thoracostomy would overcome several of the limitations and would be a promising next-step to our current study.
In conclusion, based on chest CT scan measurements, patients with hemothoraces measuring above 3 cm required tube thoracostomy. Hemothoraces greater than 2 cm had more than 50% chance of receiving a chest tube. Further prospective studies are required to validate the cutoff and to investigate associations with outcomes.
No definite recommendation exists on the size of hemothoraces that require drainage using tube thoracostomy.
Hemothoraces are prevalent findings in trauma patients, yet, no standard-of-care exists that identifies need for chest tube placement based on the size of the hemothorax.
Identifying the cut-off size for a hemothorax based on computed tomography findings that would warrant placement of a chest tube.
Retrospective study of a trauma center database
Patients with hemothorax size over 3 cm received chest tube. In patients with smaller hemothoraces, presence of other findings such as pneumothorax warrants placement of chest tube.
Tube thoracostomy should be performed in any trauma patient with a hemothorax size of greater than 3 cm.
Findings are immediately applicable to the practice of trauma surgery at our center. It would also be beneficial for other subspecialties including emergency medicine, radiology and pulmonary medicine.
Manuscript source: Invited manuscript
Specialty type: Radiology, nuclear medicine and medical imaging
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Akbulut S, Sergi CM, Kai K S- Editor: Wang JL L- Editor: A E- Editor: Bian YN
| 1. | Karmy-Jones R, Jurkovich GJ. Blunt chest trauma. Curr Probl Surg. 2004;41:211-380. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 43] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 2. | Barrios C Jr, Pham J, Malinoski D, Dolich M, Lekawa M, Cinat M. Ability of a chest X-ray and an abdominal computed tomography scan to identify traumatic thoracic injury. Am J Surg. 2010;200:741-4; discussion 744-5. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 3. | Trupka A, Waydhas C, Hallfeldt KK, Nast-Kolb D, Pfeifer KJ, Schweiberer L. Value of thoracic computed tomography in the first assessment of severely injured patients with blunt chest trauma: results of a prospective study. J Trauma. 1997;43:405-11; discussion 411-2. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 220] [Cited by in F6Publishing: 192] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 4. | Karaaslan T, Meuli R, Androux R, Duvoisin B, Hessler C, Schnyder P. Traumatic chest lesions in patients with severe head trauma: a comparative study with computed tomography and conventional chest roentgenograms. J Trauma. 1995;39:1081-1086. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 60] [Cited by in F6Publishing: 63] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 5. | Omert L, Yeaney WW, Protetch J. Efficacy of thoracic computerized tomography in blunt chest trauma. Am Surg. 2001;67:660-664. [PubMed] [Cited in This Article: ] |
| 6. | Bilello JF, Davis JW, Lemaster DM. Occult traumatic hemothorax: when can sleeping dogs lie? Am J Surg. 2005;190:841-844. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 28] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 7. | Mahmood I, Abdelrahman H, Al-Hassani A, Nabir S, Sebastian M, Maull K. Clinical management of occult hemothorax: a prospective study of 81 patients. Am J Surg. 2011;201:766-769. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 8. | Eibenberger KL, Dock WI, Ammann ME, Dorffner R, Hörmann MF, Grabenwöger F. Quantification of pleural effusions: sonography versus radiography. Radiology. 1994;191:681-684. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 221] [Cited by in F6Publishing: 184] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 9. | Ruskin JA, Gurney JW, Thorsen MK, Goodman LR. Detection of pleural effusions on supine chest radiographs. AJR Am J Roentgenol. 1987;148:681-683. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 73] [Cited by in F6Publishing: 56] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 10. | Stafford RE, Linn J, Washington L. Incidence and management of occult hemothoraces. Am J Surg. 2006;192:722-726. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 36] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 11. | Moskowitz H, Platt RT, Schachar R, Mellins H. Roentgen visualization of minute pleural effusion. An experimental study to determine the minimum amount of pleural fluid visible on a radiograph. Radiology. 1973;109:33-35. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 67] [Cited by in F6Publishing: 69] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 12. | Langdorf MI, Medak AJ, Hendey GW, Nishijima DK, Mower WR, Raja AS, Baumann BM, Anglin DR, Anderson CL, Lotfipour S. Prevalence and Clinical Import of Thoracic Injury Identified by Chest Computed Tomography but Not Chest Radiography in Blunt Trauma: Multicenter Prospective Cohort Study. Ann Emerg Med. 2015;66:589-600. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 56] [Cited by in F6Publishing: 59] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 13. | De Vis JB, Zwanenburg JJ, van der Kleij LA, Spijkerman JM, Biessels GJ, Hendrikse J, Petersen ET. Cerebrospinal fluid volumetric MRI mapping as a simple measurement for evaluating brain atrophy. Eur Radiol. 2016;26:1254-1262. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 14. | Yan J, Schwartz LH, Zhao B. Semiautomatic segmentation of liver metastases on volumetric CT images. Med Phys. 2015;42:6283-6293. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |