Published online Aug 26, 2017. doi: 10.4330/wjc.v9.i8.693
Peer-review started: November 10, 2016
First decision: March 8, 2017
Revised: March 29, 2017
Accepted: May 3, 2017
Article in press: May 5, 2017
Published online: August 26, 2017
To extend our previously-published experience in estimating pressure gradients (PG) via physical examination in a large patient cohort.
From January 1, 1997 through December 31, 2009, an attending pediatric cardiologist compared clinical examination (EXAM) with Doppler-echo (ECHO), in 1193 patients with pulmonic stenosis (PS, including tetralogy of Fallot), aortic stenosis (AS), and ventricular septal defect (VSD). EXAM PG estimates were based primarily on a murmur’s pitch, grade, and length. ECHO peak instantaneous PG was derived from the modified Bernoulli equation. Patients were 0-38.4 years old (median 4.8).
For all patients, EXAM correlated highly with ECHO: ECHO = 0.99 (EXAM) + 3.2 mmHg; r = +0.89; P < 0.0001. Agreement was excellent (mean difference = -2.9 ± 16.1 mmHg). In 78% of all patients, agreement between EXAM and ECHO was within 15 mmHg and within 5 mmHg in 45%. Clinical estimates of PS PG were more accurate than of AS and VSD. A palpable precordial thrill and increasing loudness of the murmur predicted higher gradients (P < 0.0001). Weight did not influence accuracy. A learning curve was evident, such that the most recent quartile of patients showed ECHO = 1.01 (EXAM) + 1.9, r = +0.92, P < 0.0001; during this time, the attending pediatric cardiologist had been > 10 years in practice.
Clinical examination can accurately estimate PG in PS, AS, or VSD. Continual correlation of clinical findings with echocardiography can lead to highly accurate diagnostic skills.
Core tip: Knowing pressure gradients across valves, arteries, and ventricular septal defects is important to clinical management of patients. In a large cohort of patients, we have determined the high degree of accuracy of the physical examination against the benchmark Doppler echocardiography. We discuss this clinical approach in the context of clinical practice, technology, and healthcare costs.
- Citation: Kadle RL, Phoon CKL. Estimating pressure gradients by auscultation: How technology (echocardiography) can help improve clinical skills. World J Cardiol 2017; 9(8): 693-701
- URL: https://www.wjgnet.com/1949-8462/full/v9/i8/693.htm
- DOI: https://dx.doi.org/10.4330/wjc.v9.i8.693
Strong clinical skills, including history-taking and physical diagnostic skills, remain an important part of patient evaluation - central to the practice of medicine. The clinical skills required for auscultation are especially important in childhood, when more than 50% of children have heart murmurs, most of which are benign[1,2]. In recent years however, there have been a decline in clinical examination skills and an increasing reliance on diagnostic testing[3-7].
The gradual loss of emphasis on physical exam skills has several implications[8-11]. The physical exam is an integral part of the doctor-patient relationship, and can also garner otherwise unattainable observations and findings. Additionally, the information obtained from the physical exam can help delineate the need for further testing. Although there have been several initiatives to minimize wasteful testing by focus on clinical examination[12-14], few groups have described specific and learnable techniques to do so.
In this follow-up to a small pilot study[15], our objectives of this study were several-fold. We hoped to further validate our technique of estimating peak pressure gradients through auscultation with a much larger cohort of patients. We also hoped to debunk the idea that the physical exam has a dwindling role in medicine; we believe its use in conjunction with technology can allow for a more accurate clinical assessment. We also hoped to determine the specific situations and characteristics associated with a more accurate physical exam, allowing others to learn this technique as well.
The methods are essentially as detailed in our previous report[15]. This study was approved by the Institutional Review Boards at NYU Langone Medical Center and Bellevue Hospital Center (both located in New York, NY, United States). Including our initial cohort of 151 patients[15], a total of 1193 consecutive patients with pulmonary stenosis (PS, n = 563), aortic stenosis (AS, n = 234), or ventricular septal defect (VSD, n = 396) were studied by both auscultation and Doppler echocardiography over a 13-year period between February 1997 and December 2009. Not all patients were diagnosed with these lesions at the visits; some were “first” visits, but the physical examination was characteristic for valvar stenosis or VSD, and therefore a clinical estimate of the pressure gradient could be made even before a diagnosis was established by echocardiography. All levels of PS (including tetralogy of Fallot) and AS, all types of VSDs, and residual lesions after surgical or transcatheter interventions were included. In our patient population, the AS seen was congenital, rheumatic, or postoperative, not the fibrocalcific AS seen in older patients. “Complex” AS or PS (as opposed to valvar AS or PS) denotes non-valvar stenosis, or multi-level stenosis; examples include the PS in patients with tetralogy of Fallot, subvalvular AS and supravalvar AS. It has been standard clinical practice in our pediatric echocardiography laboratory for the author (CKLP), an attending echocardiographer, to examine every patient briefly as time permits; it is felt by at least some echocardiographers, including the author, that this preliminary examination (which may include palpation and auscultation, especially of the heart sounds and murmurs) improves the reliability of the echocardiographic study. This physical examination helps to assess the degree of clinical suspicion and to focus the requested echocardiogram. For lesions with pressure gradients, the author routinely estimates a pressure gradient (see below) before the echocardiographic study. It should be noted this study was started (1997) only 1.5 years following the completion of clinical fellowship training by CKLP; therefore, at the completion of data acquisition (2009), 13.5 years had elapsed since completion of training.
The auscultatory pressure gradient was estimated by an “auscultatory scale” based predominantly on a murmur’s perceived predominant frequencies and frequency spread[15,16]. A stethoscope is inched around the chest until the highest frequencies of a murmur are heard. These frequencies are then used to estimate the pressure gradient. As the examiner continued to gain clinical experience, other components of auscultation were incorporated into the clinical estimate of the pressure gradients, including murmur loudness and length. Short murmurs generally comprised < 50% of systole, medium-length 50% to < 100% of systole with a crescendo-decrescendo quality, and long/holosystolic 100% of systole. Gradients were estimated in 5 mmHg range increments (for example, 5-10 mmHg or 25-30 mmHg) and then recorded as a midpoint value [5-10 (= 8 mmHg), 25-30 (= 28 mmHg), etc.]. In the remainder of this article, the terms “auscultation” and “auscultatory gradient” will refer to this technique of assessing the frequency composition of a murmur unless otherwise specified.
To avoid bias, the auscultatory gradient was recorded before Doppler echocardiography, and the Doppler examination was performed by a pediatric cardiac sonographer who was unaware of the auscultatory estimate. Echocardiograms performed solely by the author were excluded. In standard fashion, the Doppler beam was aligned as parallel as possible with the blood flow jet, without angle correction, interrogating for the maximal flow velocity from multiple views. The peak instantaneous Doppler pressure gradient was calculated with the modified Bernoulli equation. Any perceived inconsistencies between the auscultatory gradient and the echocardiographic results were resolved with further imaging.
Ideally, patients should be in a calm resting state for both the auscultatory examination and the echocardiogram because changes in activity level will change the cardiac output and therefore flow characteristics, including gradients. Because we do not routinely use conscious sedation, we examined patients in as calm a state as possible, recognizing that variability in the resting state will introduce variability into our assessments.
Age, weight, diagnoses, and history of interventions were obtained from the patient reports.
The relationship between the auscultatory and Doppler pressure gradients was assessed by simple linear regression. Agreement was assessed by Bland-Altman analysis[17]. Results are expressed as mean ± SD. Differences were analyzed with a 2-tailed Student t test. Comparison of categorical variables was performed with chi-square analysis or Fisher’s exact test. Statistical significance was set at P < 0.05.
Patients were 0-38.4 years old (mean 6.8 years, median 4.8), weighing 0.83-129 kg (mean 26.8 kg, median 18.2). There were 339 patients between 0-1 years of age (infants); 270 patients > 1 year-5 years (toddlers and young children); 311 patients between > 5 years-12 years (school-age children); 200 patients between 12-18 years (adolescents); and 73 patients older than 18 years (adults).
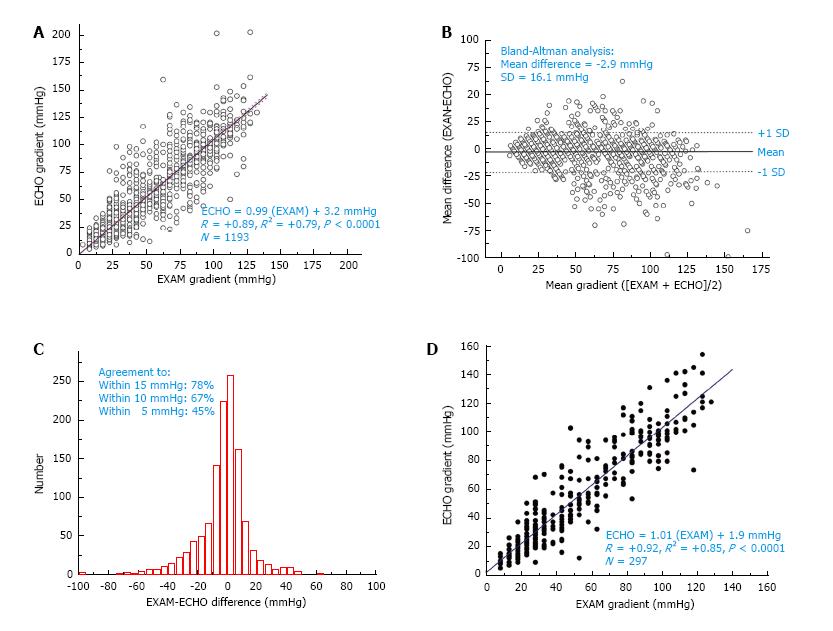
For all patients, auscultation correlated highly with echocardiography: ECHO= 0.99 (AUSC) + 3.2 mmHg; r = +0.89 (r2 = +0.79); P < 0.0001 (Figure 1A). Agreement was excellent [mean difference between clinical exam and echo = -2.9 ± 16.1 mmHg (SD), also as seen in the Bland-Altman analysis, Figure 1B]. In 78% of all patients, agreement between auscultation and echocardiography was within 15 mm Hg; in 67%, within 10 mmHg; and in 45%, within 5 mmHg (Figure 1C). Clinical estimates of PS pressure gradients were more accurate than of AS and VSD (Table 1). Valvar PS appeared to be more accurately estimated than other lesions, and VSD showed the worst agreement overall.
| Lesion | n | Mean gradient (mmHg) | Agreement to: ≤ 15 mmHg | ≤ 10 mmHg | ≤ 5 mmHg | r |
| Pulmonary stenosis | ||||||
| PS (all) | 563 | 42 ± 28 | 82% | 70% | 49% | 0.85 |
| Valvar PS | 313 | 36 ± 22 | 89% | 77% | 56% | 0.85 |
| Complex PS | 250 | 49 ± 32 | 72% | 61% | 40% | 0.84 |
| PVR | 81 | 48 ± 25 | 84% | 65% | 42% | 0.86 |
| Aortic stenosis | ||||||
| AS (all) | 234 | 38 ± 24 | 81% | 71% | 49% | 0.8 |
| Valvar AS | 112 | 42 ± 24 | 77% | 68% | 46% | 0.76 |
| Complex AS | 122 | 34 ± 23 | 85% | 75% | 52% | 0.85 |
| AVR | 34 | 46 ± 22 | 71% | 65% | 38% | 0.71 |
| Ventricular septal defect | ||||||
| VSD | 396 | 83 ± 31 | 70% | 60% | 36% | 0.82 |
A learning curve was evident. Overall agreement and correlation in the original published cohort of 151 patients [ECHO = 0.99 (AUSC) + 7.12, r = +0.84 (r2 = +0.71)] were worse (Phoon 2001); the most recent quartile of patients showed ECHO = 1.01 (AUSC) + 1.9, r = +0.92 (r2 = +0.85), P < 0.0001 (n = 297) (Figure 1D). The initial cohort[15] corresponded to a time period from early 1997 through mid-1998, while the most recent quartile of data corresponded to a time period from mid-2007 through end of 2009; thus, there was a 10-year difference in clinical experience.
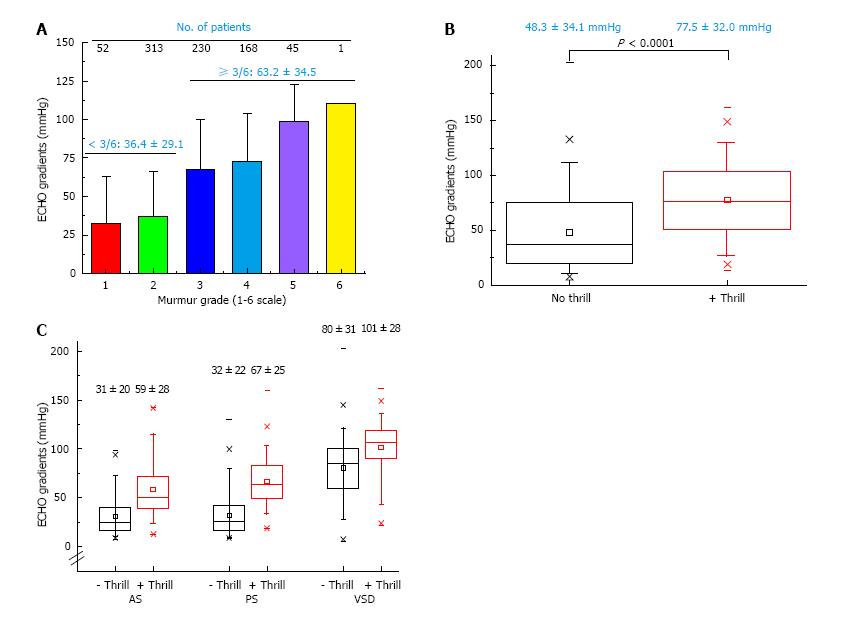
Increasing loudness of the murmur (standard 1-6 grade scale) predicted higher gradients (r = +0.54, P < 0.0001), with the largest gap occurring between grades 2 (mean PG: 36 ± 29 mmHg) and 3 (mean PG: 63 ± 35 mmHg) (Figure 2A). Similarly and as expected, a palpable precordial thrill predicted significantly higher gradients [all P < 0.0001: PS: 32 ± 22 mmHg (no thrill) vs 67 ± 25 (+thrill); AS: 31 ± 20 vs 59 ± 29; VSD: 80 ± 31 vs 101 ± 28] (Figure 2B, C). Despite the highly significant differences in patients with and without a palpable precordial thrill, there was considerable overlap in the pressure gradients. Possible influencing factors are shown in Table 2. Heavier weight and prior surgery did not appear to influence accuracy. Infants and young toddlers appeared to be less accurately assessed. Although a previous echocardiogram (and therefore possibly knowledge of the previous gradient) exhibited a better correlation, the correlation coefficient even during a “first” visit was very high (Table 2).
| Variable | n | Mean gradient (mmHg) | Agreement to: ≤ 15 mmHg | ≤ 10 mmHg | ≤ 5 mmHg | r |
| Weight | ||||||
| ≤ 10 kg | 367 | 61 ± 32 | 71% | 61% | 42% | +0.81 |
| > 10 to 20 kg | 270 | 57 ± 36 | 79% | 69% | 46% | +0.92 |
| > 20 to 40 kg | 236 | 53 ± 38 | 81% | 71% | 48% | +0.91 |
| > 40 to 70 kg | 237 | 49 ± 34 | 81% | 67% | 42% | +0.91 |
| > 70 kg | 82 | 45 ± 35 | 85% | 74% | 48% | +0.88 |
| Age | ||||||
| < 2 yr | 414 | 60 ± 32 | 71% | 62% | 42% | +0.83 |
| ≥ 2 yr | 779 | 52 ± 36 | 81% | 70% | 46% | +0.91 |
| Prior echo? | ||||||
| No prior | 321 | 61 ± 36 | 72% | 64% | 43% | +0.85 |
| +Prior | 872 | 53 ± 35 | 79% | 68% | 45% | +0.90 |
| Operative status (all CHD) | ||||||
| No operative | 688 | 65 ± 37 | 74% | 64% | 43% | +0.89 |
| Post-operative | 505 | 42 ± 27 | 82% | 70% | 46% | +0.87 |
In several cases, the physical examination “trumped” the echocardiogram, although this represented a small percentage of all patients. Nearly all were VSD’s, for which Doppler echocardiography underestimated the predicted peak gradient due to a suboptimal Doppler incident angle (Table 3). In such cases, the VSD gradient alone would have predicted the presence of pulmonary hypertension.
| Case | Age (yr) | Lesion | Clinical Gradient | DOPP Gradient | Comment |
| 1 | 6.7 | Supravalvar PS s/p repair of TOF with homograft from RV to PA | 63 | 24 | Homograft poorly visualized; tricuspid regurgitation jet predicted a systolic RV pressure of 66 mmHg plus the right atrial v-wave, so the PS gradient was significantly underestimated by DOPP |
| 2 | 6.9 | VSD, s/p repair of TOF | 70 | 66 | Prior echocardiograms did not visualize VSD; exam led to finding of a tiny residual VSD |
| 3 | 10.8 | VSD | 88 | 63 | Poor DOPP incident angle predicted pulmonary hypertension |
| 4 | 0.005 | VSD | 68 | NA | VSD was so tiny and anterior, a jet could not be obtained for a DOPP gradient |
| 5 | 4.3 | VSD | 73 | 61 | BP 104/50; poor DOPP incident angle predicted pulmonary hypertension |
| 6 | 0.01 | VSD | 88 | 48 | Technician obtained initial VSD DOPP gradient of 28 mmHg; exam prompted a search for a better DOPP angle |
| 7 | 2.8 | VSD | 83 | 55 | Poor DOPP incident angle predicted pulmonary hypertension; tricuspid regurgitation jet predicted normal PA pressures |
| 8 | 5.5 | VSD, s/p repair | 98 | 62 | Poor DOPP incident angle predicted pulmonary hypertension; tricuspid and pulmonary regurgitation jets predicted normal PA pressures |
| 9 | 3.8 | VSD | 73 | 53 | Poor DOPP incident angle predicted pulmonary hypertension; tricuspid regurgitation jet predicted normal PA pressures |
| 10 | 15.4 | VSD, Shone’s complex with minimal LV outflow tract obstruction | 93 | 63 | Poor DOPP incident angle predicted pulmonary hypertension |
| 11 | 15.7 | VSD | 118 | 73 | Poor DOPP incident angle predicted pulmonary hypertension, even though the VSD was 2.8 mm in diameter; tricuspid and pulmonary regurgitation jets predicted normal PA pressures |
This large dataset extends our previous observations and confirms that physical examination, relying mainly on auscultation, can be very accurate in determining pressure gradients. We emphasize that our purpose was not to diagnose specific conditions de novo, but to evaluate pressure gradients clinically. Other studies have previously demonstrated that the cardiac physical exam, specifically auscultation, can accurately distinguish benign from pathologic murmurs[15,18-24]. Although these studies look at auscultation in general, they do not specifically analyze pressure gradients. We have now in more detail analyzed some of those aspects of clinical auscultation, as well as patient characteristics, which impact the accuracy of the physical examination. A key finding in this study is how technology - in this case, echocardiography - can help improve clinical skills, presumably by providing feedback to the examiner.
Pressure gradients have been examined in dogs, and have been found to both correlate with echocardiographic findings[25-28] and be associated with severity of disease[29]. These studies corroborate the validity of our findings, and we further show its applicability to human subjects. Several groups have shown that examination can diagnose both AS and PS successfully[30-36]. Diagnosis of VSDs by clinical exam is also accurate but can be imperfect for major VSDs[37]. Our study takes these analyses further by laying out a specific auscultatory technique to assess heart murmurs, and by continually correlating clinical findings with echocardiographic data to improve accuracy. We demonstrate that auscultation has the greatest accuracy in predicting pressure gradients in PS, and is still accurate but less so in VSD. We speculate that the murmur of PS is consistently directed in a similar direction in nearly all patients, whereas VSD jets would exhibit far more variability that may change their auscultatory characteristics. We additionally experienced several cases in which echocardiography underestimated the severity of the murmur, or missed the etiology of a murmur completely, demonstrating the significance of auscultation in a clinical exam.
Several auscultatory characteristics have been identified to predict pathologic disease, such as holosystolic timing, harshness, grade 3 or more, or palpable precordial thrill[24,38]. We confirmed such factors can be used to estimate pressure gradients clinically, specifically the loudness of the murmur and the presence of a palpable thrill. Somewhat surprisingly, neither heavier weight nor prior surgery worsened clinical accuracy, even though we had wondered if adipose or scar tissue would impact the auscultated frequency spectrum of heart murmurs.
We believe several teaching points can be made from our data. Although the data exhibit much overlap, the presence of a precordial thrill may help differentiate higher gradients in PS and AS, although this appears to be much less useful with VSD’s. For both PS and AS, the presence of a thrill is likely to indicate a pressure gradient of > 40-45 mmHg. Infants and toddlers also are more difficult to assess clinically.
Our study raises the question of whether clinical skills such as these are important in the current era of medical practice. It is debatable or even unlikely a study such as this will impact use of technology or healthcare costs significantly. Nevertheless, it is our impression that: (1) some cases were diagnosed based primarily on clinical findings, and echocardiography played a limited or initially misleading role; and (2) our data exposes some strengths and weaknesses of the cardiac physical examination with regards to estimating pressure gradients. We and others continue to believe the gradual loss of emphasis on physical exam skills has several implications.
The physical exam is a central part of the doctor-patient relationship. The intimate contact of a physical exam not only gives the patient a sense of comfort and confidence in their physician, but can itself help the patient heal[10,11,39,40]. Besides the desired dynamic bedside skills help to create, there is also a great deal of information obtained through the physical exam that might otherwise be lost[11,41]. Many clinical signs and symptoms cannot be classified by technology alone, and can only be appreciated with a thorough physical exam. Fred discussed the implications of over-reliance on CT scans in the diagnosis of patients, including delays in treatment by waiting for a CT scan to confirm a diagnosis that can be made by physical examination alone[9]. McGee described several instances where the physical exam bested technological testing, including reactive arthritis and pericarditis[42].
However, as Verghese et al[39] argue, it is not a fight of physical exam skills vs technology, but the attempt to merge these two to produce the optimal comprehensive exam. Ippisch et al[43] demonstrated this with regards to cardiology specifically. Neither the physical exam nor a hand-carried echocardiography machine were as accurate as the two used together[6]. We conclude that technology does not erode physical exam skills but in fact improves both bedside skills and clinical judgment. Technology and clinical examination can and should go hand-in-hand for optimal patient care. “It has to make sense”[16].
Recently, several groups have discussed the development of technologies that can assist physicians in analyzing heart murmurs, including computer-assisted auscultation and artificial neural networks[44,45]. Heart murmurs are complex sounds that can nevertheless be analyzed by a simple frequency analysis, which can be done either with advanced technologies or with a trained ear and a stethoscope.
It has been shown that physicians listening to recorded heart sounds can accurately distinguish innocent from pathologic murmurs[46-48]. Therefore, telecardiology (tele-auscultation) may find potential use in areas where access to echocardiography is limited. Many rural areas, both in the United States and around the world, do not have either an echocardiography machine or a trained echocardiographer. Doctors trained to auscultate for peak pressures could feasibly receive digital heart sounds from remote areas, and improve remote diagnostic capabilities.
As physicians move away from their stethoscopes, they increasingly rely on diagnostic testing that may be unnecessary and is often uninformed, and certainly costly. Unfortunately in our study, it is impossible to know how many patients could have avoided an echocardiogram, based purely on auscultatory estimation of a pressure gradient; other clinical questions may also prompt an echocardiogram. Nevertheless, in response to the increasing impact of echocardiography on health care costs, the ACCF and the ASE prepared a 2011 revision on appropriate use criteria (AUC) for echocardiography[14] More recently AUC has also been described for pediatric echocardiography, specifically to determine the need for TTE as an initial diagnostic tool in the outpatient setting[13]. The AUC are not absolute, but should be applied to clinical exams to determine when an echocardiogram is appropriate. We believe that an increased focus on auscultation would aid in this.
This technique has been proven rigorously for one cardiologist only. The study period corresponded to this cardiologist’s early and middle career. Of note, in our original study, we validated the auscultatory scale using a senior pediatric cardiology fellow. In our anecdotal experience, several other individuals have mastered this technique to some degree. Similar to our findings, others have shown that attention to clinical examination skills can allow residents and students to improve their physical exam skills and diagnoses[1]. Moreover, similar findings in animal studies as cited above further validate our approach[25-29].
This study was performed primarily in children but included heavier children as well as some adults. Still, this data may not be applicable to adults with calcific valve disease or other pathologies not addressed in this study. In addition, pressure gradients depend on flow, and the true severity of a valvar or arterial obstruction may not be reliably assessed when there is myocardial failure. For instance, severe AS in adults may present with only a short, unimpressive midsystolic murmur or even no murmur at all. Finally, we did not test this technique for diastolic gradients.
Physical examination can accurately estimate pressure gradients in most patients with PS, AS, or VSD. An accurate physical examination may provide data that may be missed by technology, contribute to the patient-doctor relationship, and has a role for the cost-conscientious physician. And it may prove useful in areas with limited access to technological resources. We do not propose that the physical exam should replace echocardiography, but believe that the use of the two in conjunction allows for the optimal patient assessment. Contrary to the belief that technology erodes clinical skills, continual correlation of clinical findings with a technological “gold standard” such as echocardiography can lead to highly accurate diagnostic skills and improved clinical judgment, thereby enhancing clinical skills training and further substantiating the value of clinical examination.
Strong clinical skills, including physical examination skills, remain central to the practice of medicine. In recent years, there has been a much-decried decline in clinical examination skills. The authors had performed a small pilot study over 15 years ago with 151 patients that indicated that physical examination can be very accurate in determining pressure gradients across stenosis or septal defects.
Very little research is being performed to help clinicians improve clinical skills, or to determine the strengths and/or weaknesses of clinical examination. Moreover, very little is known about how technology such as imaging can help clinicians improve their physical examination skills.
In pediatric cardiology, physical examination is felt to be very accurate in determining normal from abnormal heart murmurs. What is not known, however, is whether the physical examination can accurately predict pressure gradients in aortic stenosis, pulmonary stenosis, and ventricular septal defect. Knowledge of such pressure gradients helps guide clinical management. Almost no work has been done on this area.
Honing physical examination skills such as being able to predict pressure gradients has two potential benefits: (1) The clinician may rely less on technology and therefore may reduce the use of expensive testing (imaging); and (2) The clinician may use the physical examination findings in conjunction with testing (imaging) to come to a better overall evaluation of the patient.
Aortic stenosis (AS): Anatomical obstruction to blood flow at any level, including subaortic stenosis, valvar aortic stenosis, supravalvar aortic stenosis (narrowing of the ascending aorta). In this project, aortic stenosis did not include coarctation of the aorta; Pulmonary stenosis (PS): Anatomical obstruction to blood flow at any level, including subpulmonary or infundibular stenosis, valvar stenosis, and supravalvar stenosis (narrowing of the main pulmonary artery). For the purposes of this project, the authors did not include stenoses of the peripheral branch pulmonary arteries; Ventricular septal defect (VSD): the authors included VSD’s at any site, including perimembranous, muscular, and supracristal (subpulmonary) VSD’s; Doppler echocardiography, peak instantaneous pressure gradient: For aortic or pulmonary stenosis, there will be a higher-pressure site (proximal to the obstruction) and a lower-pressure site (distal to the obstruction). For ventricular septal defects, the higher-pressure site is generally the left ventricle, while the lower-pressure site is the right ventricle. The difference in pressures (ΔP) between the two sites in the heart or arteries can be estimated using the Doppler principle on echocardiography systems; most commonly, one uses the modified Bernoulli equation, ΔP = 4V2, where V is the maximal velocity across the region of interest (stenosis or VSD) as acquired from the Doppler ultrasound transducer.
This is a well-written and interesting paper demonstrating how clinical auscultation in expert hands may approximate echo results. The results are important in an era of considerable expenses in technology and of looking down on clinical examination.
Manuscript source: Invited manuscript
Specialty type: Cardiac and cardiovascular systems
Country of origin: United States
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: den Uil CA, Innasimuthu A, Peteiro J, Petretta M S- Editor: Song XX L- Editor: A E- Editor: Lu YJ
| 1. | Dhuper S, Vashist S, Shah N, Sokal M. Improvement of cardiac auscultation skills in pediatric residents with training. Clin Pediatr (Phila). 2007;46:236-240. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 2. | Noponen AL, Lukkarinen S, Angerla A, Sepponen R. Phono-spectrographic analysis of heart murmur in children. BMC Pediatr. 2007;7:23. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 39] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 3. | Mangione S, Nieman LZ, Gracely E, Kaye D. The teaching and practice of cardiac auscultation during internal medicine and cardiology training. A nationwide survey. Ann Intern Med. 1993;119:47-54. [PubMed] [Cited in This Article: ] |
| 4. | St Clair EW, Oddone EZ, Waugh RA, Corey GR, Feussner JR. Assessing housestaff diagnostic skills using a cardiology patient simulator. Ann Intern Med. 1992;117:751-756. [PubMed] [Cited in This Article: ] |
| 5. | Gaskin PR, Owens SE, Talner NS, Sanders SP, Li JS. Clinical auscultation skills in pediatric residents. Pediatrics. 2000;105:1184-1187. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 82] [Cited by in F6Publishing: 89] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 6. | Roelandt JR. The decline of our physical examination skills: is echocardiography to blame? Eur Heart J Cardiovasc Imaging. 2014;15:249-252. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 21] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 7. | Johnson JE, Carpenter JL. Medical house staff performance in physical examination. Arch Intern Med. 1986;146:937-941. [PubMed] [Cited in This Article: ] |
| 8. | Fred HL. Hyposkillia: deficiency of clinical skills. Tex Heart Inst J. 2005;32:255-257. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 9. | Fred HL. The downside of medical progress: the mourning of a medical dinosaur. Tex Heart Inst J. 2009;36:4-7. [PubMed] [Cited in This Article: ] |
| 10. | Phoon CK. Must doctors still examine patients? Perspect Biol Med. 2000;43:548-561. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Verghese A, Horwitz RI. In praise of the physical examination. BMJ. 2009;339:b5448. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 58] [Cited by in F6Publishing: 56] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 12. | Levinson W, Kallewaard M, Bhatia RS, Wolfson D, Shortt S, Kerr EA; Choosing Wisely International Working Group. ‘Choosing Wisely’: a growing international campaign. BMJ Qual Saf. 2015;24:167-174. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 331] [Cited by in F6Publishing: 349] [Article Influence: 34.9] [Reference Citation Analysis (0)] |
| 13. | Writing Group for Echocardiography in Outpatient Pediatric Cardiology, Campbell RM, Douglas PS, Eidem BW, Lai WW, Lopez L, Sachdeva R; American College of Cardiology Appropriate Use Criteria Task Force; American Academy of Pediatrics; American Heart Association; American Society of Echocardiography; Heart Rhythm Society; Society for Cardiovascular Angiography and Interventions; Society of Cardiovascular Computed Tomography; Society for Cardiovascular Magnetic Resonance; Society of Pediatric Echocardiography. ACC/AAP/AHA/ASE/HRS/SCAI/SCCT/SCMR/SOPE 2014 appropriate use criteria for initial transthoracic echocardiography in outpatient pediatric cardiology: a report of the American College of Cardiology Appropriate Use Criteria Task Force, American Academy of Pediatrics, American Heart Association, American Society of Echocardiography, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, and Society of Pediatric Echocardiography. J Am Soc Echocardiogr. 2014;27:1247-1266. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 42] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 14. | American College of Cardiology Foundation Appropriate Use Criteria Task Force; American Society of Echocardiography; American Heart Association; American Society of Nuclear Cardiology; Heart Failure Society of America; Heart Rhythm Society; Society for Cardiovascular Angiography and Interventions; Society of Critical Care Medicine; Society of Cardiovascular Computed Tomography; Society for Cardiovascular Magnetic Resonance, Douglas PS, Garcia MJ, Haines DE, Lai WW, Manning WJ, Patel AR, Picard MH, Polk DM, Ragosta M, Ward RP, Weiner RB. ACCF/ASE/AHA/ASNC/HFSA/HRS/SCAI/SCCM/SCCT/SCMR 2011 Appropriate Use Criteria for Echocardiography. A Report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, American Society of Echocardiography, American Heart Association, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, Society of Critical Care Medicine, Society of Cardiovascular Computed Tomography, and Society for Cardiovascular Magnetic Resonance Endorsed by the American College of Chest Physicians. J Am Coll Cardiol. 2011;57:1126-1166. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 457] [Cited by in F6Publishing: 456] [Article Influence: 35.1] [Reference Citation Analysis (0)] |
| 15. | Phoon CK. Estimation of pressure gradients by auscultation: an innovative and accurate physical examination technique. Am Heart J. 2001;141:500-506. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Phoon CKL. A Guide to Pediatric Cardiovascular Physical Examination, Or, How to Survive in an Outreach Clinic. Philadelphia: Lippincott-Raven 1998; . [Cited in This Article: ] |
| 17. | Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307-310. [PubMed] [Cited in This Article: ] |
| 18. | Bloch A, Crittin J, Jaussi A. Should functional cardiac murmurs be diagnosed by auscultation or by Doppler echocardiography? Clin Cardiol. 2001;24:767-769. [PubMed] [Cited in This Article: ] |
| 19. | Geva T, Hegesh J, Frand M. Reappraisal of the approach to the child with heart murmurs: is echocardiography mandatory? Int J Cardiol. 1988;19:107-113. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 61] [Cited by in F6Publishing: 65] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 20. | Klewer SE, Samson RA, Donnerstein RL, Lax D, Zamora R, Goldberg SJ. Comparison of accuracy of diagnosis of congenital heart disease by history and physical examination versus echocardiography. Am J Cardiol. 2002;89:1329-1331. [PubMed] [Cited in This Article: ] |
| 21. | Shub C. Echocardiography or auscultation? How to evaluate systolic murmurs. Can Fam Physician. 2003;49:163-167. [PubMed] [Cited in This Article: ] |
| 22. | Smythe JF, Teixeira OH, Vlad P, Demers PP, Feldman W. Initial evaluation of heart murmurs: are laboratory tests necessary? Pediatrics. 1990;86:497-500. [PubMed] [Cited in This Article: ] |
| 23. | Roldan CA, Shively BK, Crawford MH. Value of the cardiovascular physical examination for detecting valvular heart disease in asymptomatic subjects. Am J Cardiol. 1996;77:1327-1331. [PubMed] [Cited in This Article: ] |
| 24. | McCrindle BW, Shaffer KM, Kan JS, Zahka KG, Rowe SA, Kidd L. Cardinal clinical signs in the differentiation of heart murmurs in children. Arch Pediatr Adolesc Med. 1996;150:169-174. [PubMed] [Cited in This Article: ] |
| 25. | Jenni S, Gardelle O, Zini E, Glaus TM. Use of auscultation and Doppler echocardiography in Boxer puppies to predict development of subaortic or pulmonary stenosis. J Vet Intern Med. 2009;23:81-86. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 26. | Linde A, Koch J. Screening for aortic stenosis in the Boxer: Auscultatory, ECG, blood pressure and Doppler echocardiographic findings. J Vet Cardiol. 2006;8:79-86. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 27. | Kvart C, French AT, Fuentes VL, Häggström J, McEwan JD, Schober KE. Analysis of murmur intensity, duration and frequency components in dogs with aortic stenosis. J Small Anim Pract. 1998;39:318-324. [PubMed] [Cited in This Article: ] |
| 28. | Höglund K, Ahlstrom CH, Häggström J, Ask PN, Hult PH, Kvart C. Time-frequency and complexity analyses for differentiation of physiologic murmurs from heart murmurs caused by aortic stenosis in Boxers. Am J Vet Res. 2007;68:962-969. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 29. | Ahlstrom Ast C, Höglund K, Hult P, Häggström J, Kvart C, Ask P. Assessing aortic stenosis using sample entropy of the phonocardiographic signal in dogs. IEEE Trans Biomed Eng. 2008;55:2107-2109. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 30. | Perloff JK. The Clinical Recognition of Congenital Heart Disease. Philadelphia: Saunders 2012; . [Cited in This Article: ] |
| 31. | Perloff JK, Lebauer EJ. Auscultatory and phonocardiographic manifestations of isolated stenosis of the pulmonary artery and its branches. Br Heart J. 1969;31:314-321. [PubMed] [Cited in This Article: ] |
| 32. | Crawford MH, O’Rourke RA. A systematic approach to the bedside differentiation of cardiac murmurs and abnormal sounds. Curr Probl Cardiol. 1977;1:1-42. [PubMed] [Cited in This Article: ] |
| 33. | Leatham A, Weitzman D. Auscultatory and phonocardiographic signs of pulmonary stenosis. Br Heart J. 1957;19:303-317. [PubMed] [Cited in This Article: ] |
| 34. | Lembo NJ, Dell’Italia LJ, Crawford MH, O’Rourke RA. Bedside diagnosis of systolic murmurs. N Engl J Med. 1988;318:1572-1578. [PubMed] [Cited in This Article: ] |
| 35. | Ellison RC, Wagner HR, Weidman WH, Miettinen OS. Congenital valvular aortic stenosis: clinical detection of small pressure gradient. Prepared for the joint study on the joint study on the natural history of congenital heart defects. Am J Cardiol. 1976;37:757-761. [PubMed] [Cited in This Article: ] |
| 36. | Danford DA, Salaymeh KJ, Martin AB, Fletcher SE, Gumbiner CH. Pulmonary stenosis: defect-specific diagnostic accuracy of heart murmurs in children. J Pediatr. 1999;134:76-81. [PubMed] [Cited in This Article: ] |
| 37. | Danford DA, Martin AB, Fletcher SE, Gumbiner CH, Cheatham JP, Hofschire PJ, Kugler JD. Children with heart murmurs: can ventricular septal defect be diagnosed reliably without an echocardiogram? J Am Coll Cardiol. 1997;30:243-246. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 17] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 38. | Frommelt MA. Differential diagnosis and approach to a heart murmur in term infants. Pediatr Clin North Am. 2004;51:1023-1032, x. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 27] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 39. | Verghese A, Brady E, Kapur CC, Horwitz RI. The bedside evaluation: ritual and reason. Ann Intern Med. 2011;155:550-553. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 93] [Cited by in F6Publishing: 97] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 40. | Elder A, Chi J, Ozdalga E, Kugler J, Verghese A. A piece of my mind. The road back to the bedside. JAMA. 2013;310:799-800. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 41. | Fred HL, Grais IM. Bedside skills: an exchange between dinosaurs. Tex Heart Inst J. 2010;37:205-207. [PubMed] [Cited in This Article: ] |
| 42. | McGee S. A piece of my mind. Bedside teaching rounds reconsidered. JAMA. 2014;311:1971-1972. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 27] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 43. | Ippisch HM, Kimball TR. The impact of evolving hand-carried echocardiographic technology on outpatient physical examination accuracy in pediatric cardiology. Congenit Heart Dis. 2007;2:170-178. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 44. | Watrous RL, Thompson WR, Ackerman SJ. The impact of computer-assisted auscultation on physician referrals of asymptomatic patients with heart murmurs. Clin Cardiol. 2008;31:79-83. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 46] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 45. | Bhatikar SR, DeGroff C, Mahajan RL. A classifier based on the artificial neural network approach for cardiologic auscultation in pediatrics. Artif Intell Med. 2005;33:251-260. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 79] [Cited by in F6Publishing: 77] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 46. | Belmont JM, Mattioli LF. Accuracy of analog telephonic stethoscopy for pediatric telecardiology. Pediatrics. 2003;112:780-786. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 20] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 47. | Mahnke CB, Mulreany MP, Inafuku J, Abbas M, Feingold B, Paolillo JA. Utility of store-and-forward pediatric telecardiology evaluation in distinguishing normal from pathologic pediatric heart sounds. Clin Pediatr (Phila). 2008;47:919-925. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 48. | Dahl LB, Hasvold P, Arild E, Hasvold T. Heart murmurs recorded by a sensor based electronic stethoscope and e-mailed for remote assessment. Arch Dis Child. 2002;87:297-301; discussion 297-301. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 45] [Article Influence: 2.0] [Reference Citation Analysis (0)] |