Published online Apr 26, 2017. doi: 10.4330/wjc.v9.i4.384
Peer-review started: October 13, 2016
First decision: November 30, 2016
Revised: February 4, 2017
Accepted: February 28, 2017
Article in press: March 2, 2017
Published online: April 26, 2017
Ostial lesions present unique challenges for percutaneous coronary intervention (PCI). These lesions are often more calcified, fibrotic, rigid, and more prone to elastic recoil. Intervention on these lesions is associated with higher procedural complications and higher rates of restenosis. Ostial lesions require precise stent placement in the ostium with the absence of side branch compromise. Accurate stent placement in the ostium without side branch compromise is difficult to accomplish with angiography alone. The Szabo technique uses two coronary guidewires for the correct placement in the aorto-ostial or bifurcation lesion. One guidewire is passed through the final cell of the stent strut and acts as the anchor wire. It helps to prevent migration of the stent beyond the ostium and facilitates the precise stenting at the ostium. This technique has several advantages including less reliance on angiography, lower rates of stent malposition and lower rates of incomplete stent coverage. Potential disadvantages include stent distortion and dislodgement from stent manipulation. We describe two cases of successful PCI to bifurcation lesions using the Szabo technique and confirmation of correct placement in the ostium with optical coherence tomography.
Core tip: Percutaneous intervention of ostial and bifurcation lesions is associated with higher rates of restenosis and procedural complications. Vessel anatomy, histology, and the variable angle of takeoff of ostial lesions contribute to the challenging nature of intervention. Lesion histology demonstrates greater calcification, rigidity, eccentricity as well as thicker muscular and elastic tissue, which contribute to greater elastic recoil. The Szabo two-wire technique provides accurate and complete stent positioning within the ostium, with less dependence on angiography. Intravascular imaging such as with intravascular ultrasound and optical coherence tomography (OCT) can confirm proper stent positioning. We describe two cases of successful percutaneous coronary intervention to bifurcation lesions using the Szabo technique and confirmation of correct placement in the ostium with OCT.
- Citation: Yu K, Hundal H, Zynda T, Seto A. Three-dimensional optical coherence tomography reconstruction of bifurcation stenting using the Szabo anchor-wire technique. World J Cardiol 2017; 9(4): 384-390
- URL: https://www.wjgnet.com/1949-8462/full/v9/i4/384.htm
- DOI: https://dx.doi.org/10.4330/wjc.v9.i4.384
The Szabo or anchor-wire technique utilizes two coronary guidewires for the precise placement of stents in aorto-ostial or bifurcation lesions. One guidewire is placed in the main artery, while the second wire is placed in the side branch or aorta and threaded through the most proximal strut of the stent[1,2]. Gutiérrez-Chico et al[3] evaluated it in a retrospective study in 2010 that showed reduction in incidence of angiographic malpositioning in bifurcation and aorto-ostial lesions without increasing complications. Others have concluded that the technique is imprecise with stent protrusion into the proximal main vessel after evaluation with intravascular ultrasound (IVUS) or stent dislodgement[4,5]. We present two such cases of evaluation of stent placement by the Szabo technique using optical coherence tomography (OCT).
A 27-year-old female with CREST syndrome, limited scleroderma, interstitial lung disease, mild pulmonary hypertension, and chronic kidney disease (CKD) from scleroderma renal crises presented with intermittent atypical chest pain. It was midsternal, not worsened with exercise or relieved with rest, but relieved with nitroglycerin. During one episode of chest pain, she had an elevated troponin to 5.0 ng/mL. She was initially managed conservatively due to her CKD and equivocal nuclear stress test findings. She continued to have daily angina that was responsive to nifedipine so a coronary angiography was performed.
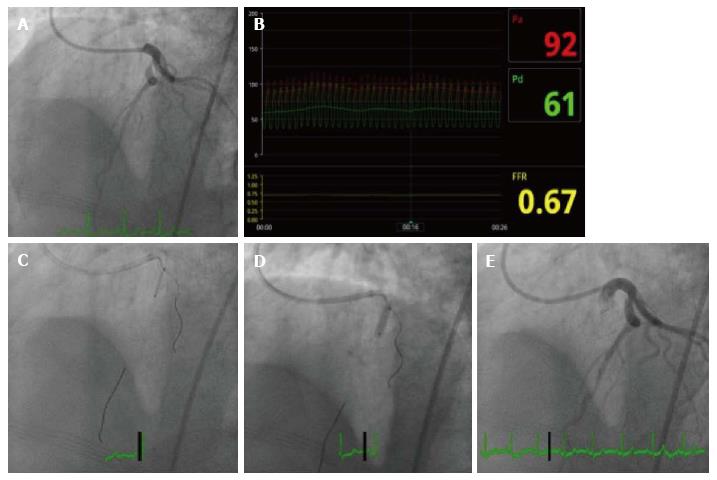
Her angiogram revealed a severe stenosis of the proximal left anterior descending (LAD) distal to the bifurcation of a high diagonal vessel (Figure 1) with associated collaterals from the right coronary artery and slow flow. The right coronary artery and left circumflex were normal. The patient had chest pain during the angiogram. Nitroglycerin relieved her symptoms and improved the angiographic flow of the LAD, but the stenosis distal to the takeoff of the diagonal was persistent.
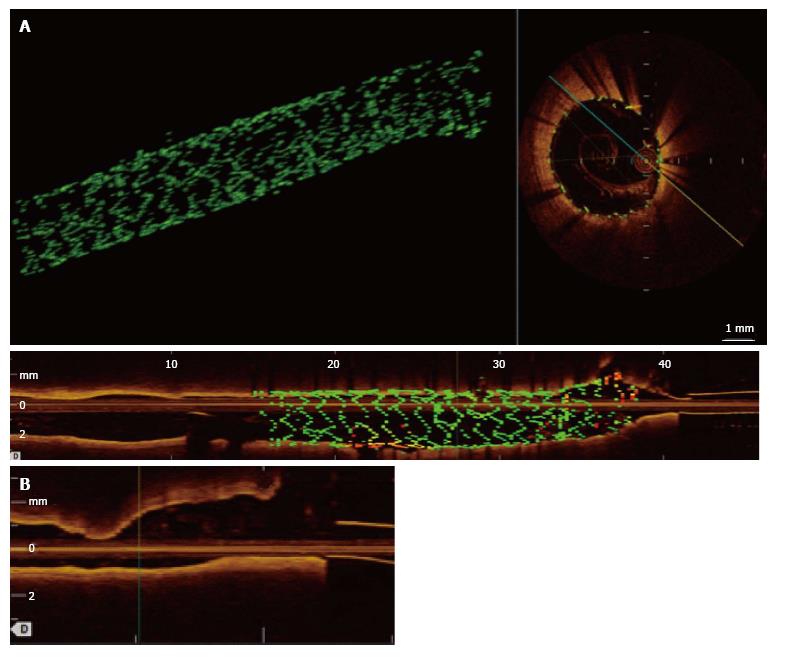
Using an XB 3.5 guide catheter, a pressure wire (PressureWire Aeris, St. Jude Medical, St. Paul, MN, United States), was advanced across the LAD lesion and the resting Pd/Pa ratio was found to be ischemic at 0.67. A HiTorque Whisper MS wire (Abbott Vascular, Temecula, CA, United States) was advanced past the lesion in the LAD and the PressureWire was removed. A second wire, PT 2 (Boston Scientific, Natick, MA), was advanced into the high diagonal. The LAD lesion was pre-dilated with a 2.0 mm × 12 mm compliant balloon. Coronary stent placement was performed using the Szabo technique with a 3.0 mm × 15 mm drug Xience drug eluding stent. Post-dilation was performed with a 3.0 mm × 8 mm non-compliant balloon. Intravascular imaging with OCT was performed from the LAD, and showed stent malapposition and insufficient expansion of the distal portion of the stent, but also demonstrated optimal stent positioning with only a single stent strut visible beyond the ostium of the main branch of the LAD. Repeat OCT from the diagonal artery showed no stent struts encroaching on the diagonal artery. Other notable OCT findings were the absence of atherosclerotic disease and the presence of intimal medial hypertrophy in the proximal LAD rather than atherosclerosis. Following OCT images, the stent was post-dilated with a 4-0 noncompliant balloon with excellent results (Figure 2).
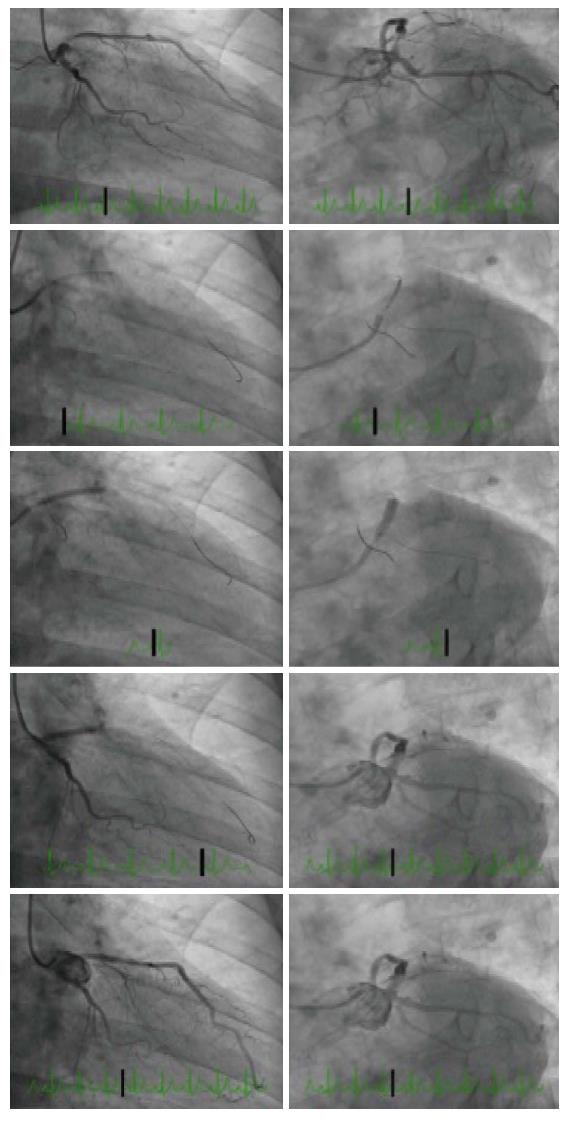
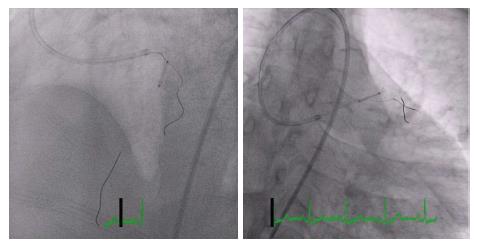
A 65-year-old man with atypical chest pain underwent stress echocardiography, which demonstrated ischemia in the LAD territory. Angiography showed separate ostia of the LAD and left circumflex artery (LCx) and proximal moderate to severe LAD stenosis (Figure 3). Percutaneous coronary intervention (PCI) using the anchor wire technique was performed. An IL 3.5 guide catheter was used to engage the LAD. A Balanced Middleweight 0(Abbott).014” coronary guidewire was placed across the lesion. A Whisper MS wire (Abbott) was backloaded through the proximal stent strut and across the LCx artery. A Vision 3.5 × 23 bare metal stent (Abbott) was deployed in the proximal LAD, anchored by the LCx wire. OCT of the LAD revealed adequate stent apposition. OCT of the LCx did not show any protrusion of stents into the branch vessel (Figure 4).
Precise stent placement in ostial and bifurcation lesions can be technically challenging. Proper stent placement is essential as a stent placed too proximally may obstruct side branches or make future interventions difficult by preventing guiding catheter engagement. A stent placed too distally results in the use of additional stents leading to stent overlap and an increased risk of stent restenosis and adverse outcomes. Angiography alone has inherent limitations in visualizing bifurcation and ostial lesions of due to foreshortening, vessel overlap, and poor resolution. Intravascular imaging with OCT or IVUS are essential in such cases.
Several different interventional techniques have been developed to treat ostial or bifurcation lesions. Many operators attempt to optimize placement with careful fluoroscopic views, but this is associated with a significant risk of geographic miss and restenosis. PCI with a single stent approach extending across the side branch can be reasonable when there is no significant disease in the side branch and the side branch is comparably small. Side branch wiring without anchoring the stent strut can be used to mark the bifurcation but has limited accuracy. Bifurcation stenting with a two-stent strategy would have been inappropriate for these Medina 0, 1, 0 lesions because there was no disease in the side branch and five-year outcome data from the Nordic bifurcation study confirmed an absence of benefit and an increase in complications with an empiric two-stent strategy[6].
We performed PCI using an anchor wire technique in both cases because the side branches were comparably large and without disease. With the anchor wire technique, both the main and side branch vessel are wired. The stent is loaded onto the main branch wire and the back end of the side branch wire (aka anchor wire) is carefully inserted through the final cell of the stent. This can be done by partially flaring the back of the stent using a partial inflation of the balloon while the stent cover is still in place. The stent is then manually re-crimped onto the balloon and advanced gently over both wires. The stent is pushed across the lesion, until the anchor wire prevents further forward motion. The stent is then deployed, the anchor wire removed, and the stent post-dilated. The advantages of this technique are decreased dependence on angiographic localization and avoidance of proximal protrusion or side branch compromise (Figure 5).
The Szabo technique has been evaluated by angiography and intravascular ultrasonography[7]. A series of 26 patients using the Szabo technique demonstrated a success rate of only 88% by angiography with a few cases of stent dislodgment and deformation[4]. In a series of 41 patients, PCI at the ostial lesion by the Szabo technique showed success rate 97.6% by IVUS[8]. In our experience, there are several ways to minimize complications. First, this technique is probably safest for aorto-ostial lesions where the stent does not need to traverse any part of the coronary artery before reaching the lesion. Second, the side branch wire should be stiff to allow for resistance to stent advancement and should not have a polymer coating that may be stripped off as the wire is removed through the stent struts. Third, balloon expansion when backloading the wire onto the stent should be minimized or even avoided as any stent deformation may interfere with stent advancement and recovery. Lastly, testing the advancement of the stent into the main branch without the anchor wire will ensure that the stent will advance smoothly and reduce the risk of stent dislodgement upon attempted withdrawal.
While the Szabo technique has been evaluated by angiography and intravascular ultrasonography, it has not been studied with OCT. OCT has a resolution of 10-15 mm and provides excellent images of a stented vessel, especially the adequacy of stent apposition and positioning. OCT of the non-stented vessel can also provide excellent visualization of stent struts, which may be deformed or protruding into the side-branch. This technology provides more definitive evidence of successful stent placement as compared to angiography alone as individual stent struts are easily imaged with OCT. Advances in image processing capabilities have enabled three-dimensional OCT reconstruction of the artery and the stent position within the artery. This allows for even finer evaluation of individual stent struts for deformation, malapposition, or side-branch encroachment.
These two cases demonstrate that the anchor wire method can provide complete ostial coverage and optimal placement for ostial lesions as documented by OCT. Prospective evaluation of the anchor wire technique combined with three-dimensional OCT may further elucidate factors that can contribute to suboptimal long-term outcomes and adverse events.
A woman with CREST syndrome and a man with risk factors for coronary artery disease present with chest pain.
The woman from case 1 developed elevated troponin and the man from case 2 had a positive stress echocardiogram.
Gastroesophageal reflux disease, coronary vasospasm, musculoskeletal chest pain.
The woman with CREST syndrome developed a troponin of 5 ng/mL and had a chronically elevated BUN/Cr due to chronic kidney disease.
The woman from case 1 had a severe stenosis of the proximal left anterior descending artery (LAD) distal to the bifurcation of a high diagonal vessel, and the man from case 2 had separate ostia of the LAD and left circumflex artery (LCx) and proximal moderate to severe LAD stenosis.
Optical coherence tomography of the woman with CREST syndrome showed intimal medial hypertrophy, and the man from case 2 had atherosclerotic coronary artery disease.
After percutaneous coronary intervention, both patients were treated with dual antiplatelet therapy.
There are different interventional techniques to treat ostial and bifurcation lesions. The accuracy of the Szabo technique has been evaluated by both angiography and intravascular ultrasonography.
An ostial lesion begins within 3-5 mm of the origin of a major epicardial artery. The Szabo technique uses two coronary guidewires for the correct placement in the aorto-ostial or bifurcation lesion.
Precise stent placement in ostial and bifurcation lesions can be technically challenging, but the anchor wire method can be used to provide complete ostial coverage and optimal placement.
It is a fine case presentation with new stenting technique. The manuscript is well-written and deserves publication.
Manuscript source: Invited manuscript
Specialty type: Cardiac and cardiovascular systems
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Amiya E, Nicholson GT S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | Kern MJ, Ouellette D, Frianeza T. A new technique to anchor stents for exact placement in ostial stenoses: the stent tail wire or Szabo technique. Catheter Cardiovasc Interv. 2006;68:901-906. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 49] [Cited by in F6Publishing: 49] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 2. | Szabo SAB, Vaitkus P. New technique of aorto-ostial stent placement. Am J Cardiol. 2005;96:212. [Cited in This Article: ] |
| 3. | Gutiérrez-Chico JL, Villanueva-Benito I, Villanueva-Montoto L, Vázquez-Fernández S, Kleinecke C, Gielen S, Iñiguez-Romo A. Szabo technique versus conventional angiographic placement in bifurcations 010-001 of Medina and in aorto-ostial stenting: angiographic and procedural results. EuroIntervention. 2010;5:801-808. [PubMed] [Cited in This Article: ] |
| 4. | Vaquerizo B, Serra A, Ormiston J, Miranda-Guardiola F, Webber B, Fantuzzi A, Delgado G, Brugera J. Bench top evaluation and clinical experience with the Szabo technique: new questions for a complex lesion. Catheter Cardiovasc Interv. 2012;79:378-389. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 23] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 5. | Ferrer-Gracia MC, Sánchez-Rubio J, Calvo-Cebollero I. Stent dislodgement during Szabo technique. Int J Cardiol. 2011;147:e8-e9. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 6. | Maeng M, Holm NR, Erglis A, Kumsars I, Niemelä M, Kervinen K, Jensen JS, Galløe A, Steigen TK, Wiseth R. Long-term results after simple versus complex stenting of coronary artery bifurcation lesions: Nordic Bifurcation Study 5-year follow-up results. J Am Coll Cardiol. 2013;62:30-34. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 141] [Cited by in F6Publishing: 145] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 7. | Yang S. Cardiovascular disease clinical research - Coronary intervention: GW23-e0582: Safety and feasibility of Szabo technique in percutaneous coronary intervention of ostial lesion. Heart. 2012;98:Suppl 2 E210-E211. [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Wong P. Two years experience of a simple technique of precise ostial coronary stenting. Catheter Cardiovasc Interv. 2008;72:331-334. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 25] [Article Influence: 1.6] [Reference Citation Analysis (0)] |