Peer-review started: July 26, 2016
First decision: September 5, 2016
Revised: October 8, 2016
Accepted: November 1, 2016
Article in press: November 2, 2016
Published online: January 26, 2017
To evaluate the prevalence of salt sensitivity and the impact of cardiometabolic and psychological characteristics on salt sensitivity in normotensive population.
Of all participants, anthropometric measurements and fasting venous blood samples were collected, and study questionnaires were completed. Salt Sensitivity was defined based on the difference in mean arterial pressure with infusion of 2 L of normal saline followed by a low sodium diet and administration of three doses of oral furosemide the day after.
Of 131 participants, 56 (42.7%) were diagnosed with salt sensitivity. Crude and age and sex adjusted regression analysis showed that low-density lipoprotein cholesterol and depression were positively associated with salt sensitivity (OR = 1.02, 95%CI: 1.01-1.04 and OR = 1.15, 95%CI: 1.00-1.34, respectively).
The high prevalence of salt sensitivity and its significant relation with prevalent risk factors necessitates considering its reduction actions at the population level and the need for further research.
Core tip: Mean blood pressure can be reduced following a decrease in sodium intake in both hypertensive and normotensive individuals. Normotensive individuals with salt sensitivity trait are more likely to develop hypertension and other health problems. A relatively high prevalence of salt sensitivity has been indicated among Iranian adults. Low-density lipoprotein cholesterol was found to have strong positive association with salt sensitivity. Depressive individuals were more salt sensitive.
- Citation: Sadeghi M, Roohafza H, Pourmoghaddas M, Behnamfar O, Pourmoghaddas Z, Heidari E, Mahjoor Z, Mousavi M, Bahonar A, Sarrafzadegan N. How far cardio metabolic and psychological factors affect salt sensitivity in normotensive adult population? World J Cardiol 2017; 9(1): 47-54
- URL: https://www.wjgnet.com/1949-8462/full/v9/i1/47.htm
- DOI: https://dx.doi.org/10.4330/wjc.v9.i1.47
Hypertension is a prevalent well-documented risk factor for cardiovascular disease and premature mortality and therefore is an important public health issue[1]. Essential hypertension is a common disorder in areas with average daily sodium intake of over 100 meq/d (2.3 g sodium), however, is rarely seen with average daily sodium intake of less than 50 meq/d (1.2 g sodium)[2,3].
It has been demonstrated in multiple studies that mean blood pressure (BP) can be reduced following a decrease in sodium intake in both hypertensive and normotensive individuals[4,5]. Based on these reports, a minimum level of dietary sodium independent of other risk factors is required for development of hypertension[6,7].
There is an important clinical benefit to identify and target individuals who are more sensitive to alterations in dietary sodium intake by implementing dietary sodium reduction interventions. BP variations in response to changes in dietary sodium intake are known as Salt Sensitivity. This responsiveness of BP, however, may vary significantly from individual to individual[8,9]. Normotensive individuals with this trait of salt sensitivity are said to be more likely to develop hypertension and other health problems including Cardiovascular, Respiratory, and renal disorders independent of hypertension later in life[10,11].
Although incompletely understood, multiple mechanisms for sodium sensitivity have been demonstrated, from impaired renal sodium excretion, abnormalities in signaling and vascular tone, to the role of genetics in sodium regulation[12,13].
In spite of the fact that the protocols and methods of salt sensitivity definition vary in different studies, there is a general accordance in the main observations. Salt sensitivity appears to be a reproducible phenomenon with different measurement techniques[14].
Salt sensitivity is a practical clinical concept in spite of all the difficulties in measurement and identifying the sensitive individuals. This fact that is evident by positive outcomes of the recommended dietary approaches for the prevention and treatment of hypertension (HTN) (DASH diet)[15] There are certain traits and disorders that are markedly associated with salt sensitivity including African American ethnicity, obesity, chronic kidney disease, and cardiovascular risk factors[9,16].
Previous studies conducted in the Eastern Mediterranean region (EMR) demonstrate a substantially high incidence rate of almost all cardiovascular diseases particularly HTN and increased rate of mortality even in treated subjects[17-20]. These findings along with the increasing trend of salt intake at the population level[21], beside the lack of evidence of salt sensitivity of BP in Iran and in the region, highlight the importance of conducting this study. Therefore, we aimed to evaluate the prevalence of salt sensitivity in a normotensive Iranian adult population and to investigate the impact of cardiometabolic risk factors and psychological characteristics, on salt sensitivity.
The study was conducted by the hypertension research center affiliated to Cardiovascular Research Institute (a WHO collaborating center in the EMR) from July to October 2014. In order to find potential volunteers from community, we used a wide range of materials from flyers and brochures to posters. A total of 140 healthy participants volunteered to take part in this cross-sectional study. Eligibility requirements included willingness to participate in the study, age 18 years and older, normal BP defined as systolic BP below 140 mmHg and diastolic BP below 90 mmHg based on 3 screening visits of 1 wk apart. The exclusion criteria was history of hypertension; history of special diet including low salt diets; history of taking antihypertensive medications and diuretics for any reason, oral contraceptives and nonsteroidal anti-inflammatory drugs; any history of myocardial infarction, heart failure, cerebrovascular accidents and renal failure. Written informed consents were obtained from each participant and the study protocol was approved by the ethical committee of Cardiovascular Research Institute.
A questionnaire was used at the baseline observation by trained staff to collect information on demographic characteristics as well as family history of hypertension, coronary artery disease, and lifestyle habits including regular physical activity, dietary pattern and smoking status. The Hospital Anxiety and Depression Scale questionnaire was also used to determine the score of anxiety and depression. This scale consists of seven items for anxiety and seven items for depression, with scores ranging from 0 to 21. The higher scores demonstrate more intensity in anxiety or depression level. Scores higher than 7, in both domains indicate that participants are likely to be depressed or suffer from anxiety[22,23].
Anthropometric measurements of weight, height, waist and hip circumferences were obtained during baseline examination with the individual in minimal clothing. The WHO STEPS Surveillance Manual (The WHO STEP wise Approach to Chronic Disease Risk Factor Surveillance) was used for measuring waist and hip circumference[24]. Body mass index (BMI) was calculated as weight (in kilograms) over height squared (in meters).
Venous blood samples after fasting for at least 8 h were taken for measurement of fasting blood sugar (FBS), serum blood urea nitrogen (BUN), creatinine (Cr), uric acid (UA), sodium (Na), potassium (K) levels, and lipid profile including low-density lipoprotein (LDL), high-density lipoprotein (HDL), triglycerides (TG), and total cholesterol (TC). Plasma measurements were assessed using commercially available kits (Parsazmoun). BP was measured by trained staff for each participant using an automated mercury sphygmomanometer with the individual in sitting position and 5 min of rest. All the participants were asked to avoid consumption of alcohol, tea, or coffee, physical exercise or smoking for at least one hour prior to admission. Mean arterial pressure (MAP) was calculated as [(2 × diastolic) + systolic]/3 and reported for each measurement.
We considered the following definitions for cardiovascular risk factors: Current smoking of at least one cigarette per day; lack of regular physical activity (less than 30 min a day, five days a week); raised blood glucose (FBS > 126 mg/dL); elevated blood cholesterol [TC > 200 mg/dL, TG > 150 mg/dL, LDL > 130 mg/dL, HDL below 40 mg/dL (male) and less than 50 mg/dL (female)]; and being overweight or obese (BMI > 25 kg/m2, waist circumference > 92 cm in males and > 88 cm in females)[25].
The study was conducted in two days. On the first day of the study, individuals were admitted at 8 AM and were put on a low calorie and low sodium diet (10 mmol/d). At this time, venous blood samples were obtained, anthropometric measurements were calculated, and the questionnaires were filled out from participants by trained staff. Two hours after the admission, three measurements of BP were obtained with five minutes intervals and the mean of them was recorded as the baseline BP.
After obtaining the baseline BP, 2 L of normal saline was administered intravenously over 4 h (500 mL/h). Two hours after normal saline infusion, BP was obtained and post-saline MAP was calculated. Then participants were discharged and were asked to return back to the clinic the next morning.
To ensure compliance to the study protocol, individuals were required to eat pre-packaged foods that were prepared according to the protocol including low-carbohydrate, low-fat, and low-sodium diet (10 mmol/d) and were instructed to avoid any foods that were not provided by the study staff. Participants were also followed up over the night by telephone to evaluate any potential side effects and to ensure their adherence to the study dietary protocol.
On the following day, participants were admitted again at 8 AM and BPs were obtained. Sodium and volume depletion was then induced by a low sodium diet (10 mmol/d) and administration of three doses of oral furosemide (40 mg each dose, at 10 AM, 2 PM and 6 PM). Two hours after completion of the last dose of furosemide, BP was measured according to the study protocol. The MAP after sodium and volume depletion was compared with the post-saline MAP.
Individuals who demonstrated a decrease in MAP ≥ 10 mmHg were defined as “salt sensitive”. Those with MAP decrease < 10 mmHg were categorized as “salt insensitive” including both the salt resistant (ΔMAP < 6 mmHg) and intermediate (ΔMAP 6-10 mmHg) with respect to sodium sensitivity.
All data were analyzed by SPSS, version 15 (SPSS Inc, Chicago, IL, United States). Respectively, a P value ≤ 0.05 and P value ≤ 0.1 were considered as statistically and marginally significant for all analyses. Student’s t test for continuous variables and χ2 test for discrete variables were used. Man-Whitney test was applied where appropriate. Multiple Logistic Regression model was carried out to examine the association between demographic, anthropometric, psychological characteristics and laboratory studies of those with the salt sensitivity. Odds ratios (ORs) were reported with the corresponding 95%CI. Repeated measure ANOVA was used for comparing the means of systolic BP in different times.
The dependent variable was salt sensitivity. Independent variables included demographic, anthropometric, psychosocial characteristics, laboratory studies, and cardiovascular risk factors of those adjusted based on age and sex. The statistical methods of the study were reviewed by biomedical statistician.
Of the total of 140 participants, 9 who failed to adhere to dietary protocol or did not complete the intervention were excluded from the study. Among the 131 individuals included in the study, 56 participants (42.7%) were diagnosed with salt sensitivity while 75 (57.3%) participants including 52 (39.7%) salt resistant and 23 (17.6%) intermediate were determined as salt insensitive group. Of participants, hundred were male and 31 were female, with a mean age of 25.70 ± 5.71. Significant differences were not statistically detected in the age or sex distribution between both groups.
Table 1 shows the baseline demographic, psychological and anthropometric characteristics of participants as well as laboratory evaluations. Lipid profile tests revealed that LDL cholesterol level was significantly higher in Salt Sensitive group compared with Salt Insensitive one (P = 0.038). In the Salt Sensitive group, BMI, FBS, BUN, and Cr levels were higher than those in the Salt Insensitive group with a marginally significant difference (P = 0.057, 0.072, 0.077, 0.067, respectively). There wasn’t any significant difference in the Depression or Anxiety Score between two groups.
| Variable | Salt insensitive n = 75 | Salt sensitive n = 56 | P value |
| Sex (male) (%) | 55 (73.3) | 45 (80.4) | 0.3491 |
| Age (yr) (mean ± SD) | 25.23 ± 4.68 | 26.36 ± 6.91 | 0.2722 |
| Family history of HTN (y/n) (%) | 22 (29.3) | 16 (28.6) | 0.9951 |
| Family history of CAD (y/n) (%) | 7 (9.3) | 6 (10.7) | 0.7701 |
| Regular physical activity (y/n) (%) | 30 (40.0) | 19 (33.9) | 0.5221 |
| Current smoker (y/n) (%) | 12 (16.0) | 8 (14.3) | 0.8651 |
| Weight (kg) (mean ± SD) | 68.21 ± 13.05 | 71.16 ± 12.33 | 0.1932 |
| Body mass index (kg/m2) (mean ± SD) | 22.75 ± 2.71 | 23.71 ± 2.93 | 0.0572 |
| Waist circumference (cm) (mean ± SD) | 81.54 ± 8.96 | 82.86 ± 8.41 | 0.4042 |
| Hip circumference (cm) (mean ± SD) | 96.97 ± 5.90 | 97.38 ± 5.77 | 0.6982 |
| Waist to hip ratio (mean ± SD) | 0.83 ± 0.06 | 0.84 ± 0.05 | 0.3462 |
| Waist to height ratio (mean ± SD) | 0.47 ± 0.04 | 0.48 ± 0.49 | 0.3822 |
| Fasting blood sugar (mg/dL) (mean ± SD) | 79.71 ± 6.16 | 82.64 ± 10.74 | 0.0722 |
| Total cholesterol (mg/dL) (mean ± SD) | 156.54 ± 28.70 | 164.66 ± 26.64 | 0.1092 |
| High-density lipoprotein cholesterol (mg/dL) (mean ± SD) | 46.23 ± 11.90 | 44.09 ± 12.23 | 0.3272 |
| Low-density lipoprotein cholesterol (mg/dL) (mean ± SD) | 82.56 ± 21.27 | 90.05 ± 17.49 | 0.0382 |
| Triglyceride (mg/dL) (mean ± SD) | 136.75 ± 97.26 | 145.32 ± 75.93 | 0.5942 |
| Uric acid (mg/dL) (mean ± SD) | 6.91 ± 6.57 | 6.42 ± 1.56 | 0.5972 |
| Sodium (mg/dL) (mean ± SD) | 140.30 ± 2.42 | 140.46 ± 2.39 | 0.6992 |
| Potassium (mg/dL) (mean ± SD) | 4.38 ± 0.53 | 4.34 ± 0.34 | 0.6622 |
| Blood urea nitrogen (mg/dL) (mean ± SD) | 12.56 ± 3.72 | 13.73 ± 3.63 | 0.0772 |
| Creatinine (mg/dL) (mean ± SD) | 0.92 ± 0.12 | 0.96 ± 0.10 | 0.0672 |
| Depression score (mean ± SD) | 4.00 ± 2.66 | 3.25 ± 2.15 | 0.0953 |
| Anxiety score (mean ± SD) | 3.73 ± 3.18 | 3.08 ± 3.25 | 0.1613 |
Table 2 shows the Crude, and age and sex-adjusted logistic regression analysis with salt sensitivity as an outcome. As shown in Table 2, with adjusted logistic regression analysis, LDL along with Depression were found to be the only two variables of significance (OR = 1.02, 95%CI: 1.01-1.04 and OR = 1.15, 95%CI: 1.00-1.34, respectively). At last, multiple logistic regression model with variables including, WC, Depression, FBS, LDL, Cr, age and sex was performed. Finding showed that there were not statistically difference between the result of multiple logistic regression model and age and sex adjusted logistic regression analysis and depression and LDL was still significant.
| Variable | Crude OR (95%CI) | P value | Adjusted OR (95%CI) | P value |
| Total cholesterol (mg/dL) | 1.01 (1.00-1.02) | 0.11 | 1.01 (1.00-1.03) | 0.12 |
| Triglyceride (mg/dL) | 1.01 (1.00-1.01) | 0.59 | 1.00 (1.00-1.01) | 0.87 |
| High-density lipoprotein cholesterol (mg/dL) | 0.99 (0.96-1.02) | 0.33 | 0.99 (0.96-1.02) | 0.45 |
| Low-density lipoprotein cholesterol (mg/dL) | 1.02 (1.01-1.04) | 0.04 | 1.02 (1.01-1.04) | 0.04 |
| Fasting blood sugar (mg/dL) | 1.04 (1.00-1.09) | 0.06 | 1.04 (0.99-1.09) | 0.14 |
| Sodium (mg/dL) | 1.06 (0.97-1.04) | 0.35 | 1.03(0.98-1.05) | 0.37 |
| Potassium (mg/dL) | 1.05 (0.99-1.07) | 0.51 | 1.06(0.98-1.06) | 0.41 |
| Body mass index (kg/m2) | 1.14 (1.00-1.28) | 0.06 | 1.12 (0.97-1.28) | 0.13 |
| Waist circumference (cm) | 1.02 (0.98-1.06) | 0.40 | 1.02 (0.97-1.06) | 0.49 |
| Waist to hip ratio | 1.19 (0.83-1.69) | 0.34 | 1.16 (0.76-1.79) | 0.48 |
| Regular physical activity (y/n) | 0.79 (0.38-1.64) | 0.52 | 0.85 (0.39-1.82) | 0.66 |
| Smoking (y/n) | 1.07 (0.95-1.15) | 0.40 | 1.08 (0.97-1.25) | 0.47 |
| Depression (y/n) | 1.14 (0.98-1.32) | 0.06 | 1.15 (1.00-1.34) | 0.04 |
| Family history of HTN (y/n) | 1.19 (0.37-3.85) | 0.77 | 1.28 (0.35-4.76) | 0.70 |
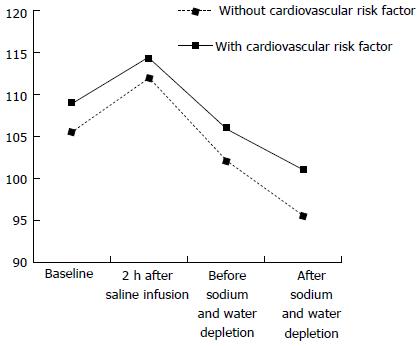
Means of systolic and diastolic BP measurements in participants without any cardiovascular risk factor compared with those with at least one risk factor at the baseline observation, 2 h after saline infusion, and before and after sodium and water depletion is shown in Figure 1. It has been founded that there is significant difference between baseline, 2 h after saline infusion and before and after sodium and water depletion (F = 102.02, P ≤ 0.001). No significant interaction was observed between groups and times. (F = 0.99, P = 0.39).
As a whole, 131 normotensive individuals properly completed the study protocol and were included in the study analysis. This study showed a relatively high prevalence of salt sensitivity among Iranian adults as well as significant and positive association between the level of LDL cholesterol and salt sensitivity. Based on age and sex adjusted logistic regression analysis, LDL cholesterol and depression were found to have strong positive association with salt sensitivity.
Multiple studies conducted in the EMR have shown high incidence rate of hypertension and its low control level in the region[18-20]. This factor along with high average intake of sodium in the Iranian diet[21] highlight the importance of integrating salt sensitivity in risk assessment and management of hypertension in the region.
The heterogeneity and susceptibility of individual BP response to Sodium intake is the basis for development of salt sensitivity and appears to be a common, normally distributed biological concept in populations[10,26]. The salt sensitivity definition and categorizing individuals to salt sensitive or insensitive is arbitrary and several methods exist to measure salt sensitivity. It can be defined as BP variations in response to a change in dietary salt or as the difference in MAP with infusion of normal saline followed by a low sodium diet and loop diuretic administration the day after[15,16]. Our protocol, with salt loading and depletion, allowed us to maximize the follow-up and adherence to the protocol with a more practical and controllable intervention. Despite the differences in the measurement or definition methods, there has been accordance in several findings[26,27].
Overall, 42.7% of participants in our study were diagnosed with salt sensitivity. Even though relatively high, it is still in line with previous reports. The salt sensitivity has been observed in 25%-50% of normotensives and 40%-75% of hypertensive patients depending on the measurement techniques and geographic variation of studies in different ethnic populations[4,5,28].
Several mechanisms for sodium sensitivity have been demonstrated[29]. Impaired renal sodium excretion with resultant sodium retention that leads to volume expansion has been suggested as one of the underlying mechanism[30-32]. Abnormalities in signaling and vascular tone in response to sodium intake are another possible process[13,14]. Multiple genes are shown to be associated with sodium regulation and salt sensitivity[33,34]. This genetic predisposition is thought to be responsible for several relations seen in the salt sensitive group.
The strong, positive association of LDL cholesterol level with salt sensitivity presented in Table 2 can be interpreted by the role of genetic predisposition. In a study by Hoffmann et al[35], the endothelial nitric oxide synthase (ENOS) gene polymorphism was shown to be associated with higher levels of LDL cholesterol and reduced levels of nitric oxide (NO) production that can be responsible for the increased BP sensitivity to salt. Several previous studies have also revealed that the alpha-adducin gene polymorphisms may increase the LDL cholesterol levels and are probably responsible for salt sensitivity of BP[33,36,37].
In the present study, depression was found to be a potential predictive variable for salt sensitivity. The mechanism by which depression is related to salt sensitivity is not clearly understood and further studies are required. However, this association can be explained by the role of stress as a predisposing factor to depression in susceptibility of BP to salt. Previous studies have demonstrated the contribution of the stress and sympathetic nervous system to salt sensitivity[10,38,39]. One mechanism might be the impaired stress-induced renin-angiotensin-aldosterone system regulation[40].
Depression and elevated LDL cholesterol level are reported to be highly prevalent among the Iranian population[41]. The fact that makes the importance of these two factors in salt sensitivity was even more significant among Iranian population.
Our findings showed that in the crude model, BMI, FBS, BUN and Cr levels were related to salt sensitivity with a marginally significant difference. The association between BMI and salt sensitivity has been noted in previous studies[39,42]. This relation may be explained by the higher sodium renal tubular reabsorption in obese individuals or due to drinking more soft drinks while eating salty products. Multiple previous studies have identified strong association between the plasma glucose level as a metabolic risk factor with salt sensitivity of BP independent of BMI, physical activity and hypertension[43]. Reduced renal function, which can be monitored with the level of BUN and Cr, has been also shown in previous observations to be associated with salt sensitivity[31].
The prevalence of salt sensitivity is increased among older individuals with a family history of hypertension[11,29], however, our results failed to show an association between higher age or positive family history of HTN and salt sensitivity. Multiple Factors such as including only normotensive participants, and relatively small sample size of the study can be considered as the reason for these inconclusive observations or differences found in our study compared to others.
The limitations of our study include relatively small sample size, the measurement method used for defining salt sensitivity, and exclusion of hypertensive individuals from the study. Even though all these factors were intentionally incorporated into the study design to enhance the practicality, feasibility and efficacy of the study, they ought to be considered as the limitations of the study.
According to our knowledge, this study is the first to investigate and report the prevalence and characteristics of salt sensitivity in our country and the EMR. The important clinical and public health implications of our study necessitate the need for more studies with larger sample size and to consider hypertensive patients too.
Authors wish to thank all study volunteers who participated to this study and the staff of Cardiovascular Research Institute for their kind cooperation.
Blood pressure (BP) can be reduced following a decrease in sodium intake in both hypertensive and normotensive individuals. There is an important clinical benefit to identify and target individuals who are more sensitive to alterations in dietary sodium intake by implementing dietary sodium reduction interventions. Normotensive individuals more likely develop hypertension and other health problems including cardiovascular, respiratory, and renal disorders independent of hypertension later in life.
Increasing trend of salt intake at the population level beside the lack of evidence of salt sensitivity of BP in Iran and in the region, highlight the importance of conducting this study.
This study evaluates the prevalence of salt sensitivity in a normotensive Iranian adult population and to investigate the impact of cardiometabolic risk factors and psychological characteristics, on salt sensitivity. According to our knowledge, this study is the first to investigate and report the prevalence and characteristics of salt sensitivity in our country and the Eastern Mediterranean Region.
Salt sensitivity is a practical clinical concept in spite of all the difficulties in measurement and identifying the sensitive individuals.
Salt sensitivity is a measure of how your BP responds to salt intake. People are either salt-sensitive or salt-resistant. Salt sensitive individuals are more likely to have high BP than those who are resistant to salt; Normotensive having or denoting a normal BP.
This is an interesting manuscript about the relations of salt sensitivity to cardiometabolic risk factors and psychological characteristics.
Manuscript source: Invited manuscript
Specialty type: Cardiac and cardiovascular systems
Country of origin: Iran
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Chawla M, Said SAM, Ueda H S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365:217-223. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2858] [Cited by in F6Publishing: 3634] [Article Influence: 191.3] [Reference Citation Analysis (1)] |
| 2. | Adrogué HJ, Madias NE. Sodium and potassium in the pathogenesis of hypertension. N Engl J Med. 2007;356:1966-1978. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 496] [Cited by in F6Publishing: 454] [Article Influence: 26.7] [Reference Citation Analysis (0)] |
| 3. | Elliott P, Stamler J, Nichols R, Dyer AR, Stamler R, Kesteloot H, Marmot M. Intersalt revisited: further analyses of 24 hour sodium excretion and blood pressure within and across populations. Intersalt Cooperative Research Group. BMJ. 1996;312:1249-1253. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 561] [Cited by in F6Publishing: 523] [Article Influence: 18.7] [Reference Citation Analysis (0)] |
| 4. | Whelton PK, He J, Appel LJ, Cutler JA, Havas S, Kotchen TA, Roccella EJ, Stout R, Vallbona C, Winston MC. Primary prevention of hypertension: clinical and public health advisory from The National High Blood Pressure Education Program. JAMA. 2002;288:1882-1888. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 997] [Cited by in F6Publishing: 934] [Article Influence: 42.5] [Reference Citation Analysis (0)] |
| 5. | Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jones DW, Materson BJ, Oparil S, Wright JT. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560-2572. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13416] [Cited by in F6Publishing: 12992] [Article Influence: 618.7] [Reference Citation Analysis (0)] |
| 6. | Strazzullo P, D’Elia L, Kandala NB, Cappuccio FP. Salt intake, stroke, and cardiovascular disease: meta-analysis of prospective studies. BMJ. 2009;339:b4567. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 977] [Cited by in F6Publishing: 1007] [Article Influence: 67.1] [Reference Citation Analysis (0)] |
| 7. | Aburto NJ, Ziolkovska A, Hooper L, Elliott P, Cappuccio FP, Meerpohl JJ. Effect of lower sodium intake on health: systematic review and meta-analyses. BMJ. 2013;346:f1326. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 845] [Cited by in F6Publishing: 793] [Article Influence: 72.1] [Reference Citation Analysis (0)] |
| 8. | Weinberger MH. Salt sensitivity of blood pressure in humans. Hypertension. 1996;27:481-490. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 554] [Cited by in F6Publishing: 550] [Article Influence: 19.6] [Reference Citation Analysis (0)] |
| 9. | Obarzanek E, Proschan MA, Vollmer WM, Moore TJ, Sacks FM, Appel LJ, Svetkey LP, Most-Windhauser MM, Cutler JA. Individual blood pressure responses to changes in salt intake: results from the DASH-Sodium trial. Hypertension. 2003;42:459-467. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 141] [Cited by in F6Publishing: 125] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 10. | Barba G, Galletti F, Cappuccio FP, Siani A, Venezia A, Versiero M, Della Valle E, Sorrentino P, Tarantino G, Farinaro E. Incidence of hypertension in individuals with different blood pressure salt-sensitivity: results of a 15-year follow-up study. J Hypertens. 2007;25:1465-1471. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 40] [Cited by in F6Publishing: 43] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 11. | Frisoli TM, Schmieder RE, Grodzicki T, Messerli FH. Salt and hypertension: is salt dietary reduction worth the effort? Am J Med. 2012;125:433-439. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 117] [Cited by in F6Publishing: 111] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 12. | Kotchen TA, Cowley AW, Frohlich ED. Salt in health and disease--a delicate balance. N Engl J Med. 2013;368:2531-2532. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 29] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 13. | Schmidlin O, Forman A, Leone A, Sebastian A, Morris RC. Salt sensitivity in blacks: evidence that the initial pressor effect of NaCl involves inhibition of vasodilatation by asymmetrical dimethylarginine. Hypertension. 2011;58:380-385. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 57] [Cited by in F6Publishing: 63] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 14. | Nakagawa K, Holla VR, Wei Y, Wang WH, Gatica A, Wei S, Mei S, Miller CM, Cha DR, Price E. Salt-sensitive hypertension is associated with dysfunctional Cyp4a10 gene and kidney epithelial sodium channel. J Clin Invest. 2006;116:1696-1702. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 111] [Cited by in F6Publishing: 114] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 15. | Vollmer WM, Sacks FM, Ard J, Appel LJ, Bray GA, Simons-Morton DG, Conlin PR, Svetkey LP, Erlinger TP, Moore TJ. Effects of diet and sodium intake on blood pressure: subgroup analysis of the DASH-sodium trial. Ann Intern Med. 2001;135:1019-1028. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 393] [Cited by in F6Publishing: 343] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 16. | Chen J, Gu D, Huang J, Rao DC, Jaquish CE, Hixson JE, Chen CS, Chen J, Lu F, Hu D. Metabolic syndrome and salt sensitivity of blood pressure in non-diabetic people in China: a dietary intervention study. Lancet. 2009;373:829-835. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 194] [Cited by in F6Publishing: 160] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 17. | Talaei M, Sarrafzadegan N, Sadeghi M, Oveisgharan S, Marshall T, Thomas GN, Iranipour R. Incidence of cardiovascular diseases in an Iranian population: the Isfahan Cohort Study. Arch Iran Med. 2013;16:138-144. [PubMed] [Cited in This Article: ] |
| 18. | Talaei M, Sadeghi M, Mohammadifard N, Shokouh P, Oveisgharan S, Sarrafzadegan N. Incident hypertension and its predictors: the Isfahan Cohort Study. J Hypertens. 2014;32:30-38. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 36] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 19. | Aljefree N, Ahmed F. Prevalence of Cardiovascular Disease and Associated Risk Factors among Adult Population in the Gulf Region: A Systematic Review. Advances in Public Health. 2015;23. [Cited in This Article: ] |
| 20. | Khosravi A, Pourmoghaddas M, Kelishadi R, Sabet B, Ansari R, Shirani S. Trends in Blood Pressure Level, Prevalence of Hypertension and its Care in Isfahan. Iran Red Crescent Med J. 2005;2006:62-68. [Cited in This Article: ] |
| 21. | Khosravi A, Kelishadi R, Sarrafzadegan N, Boshtam M, Nouri F, Zarfeshani S, Esmaillzadeh A. Impact of a community-based lifestyle intervention program on blood pressure and salt intake of normotensive adult population in a developing country. J Res Med Sci. 2012;17:235-241. [PubMed] [Cited in This Article: ] |
| 22. | Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361-370. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28548] [Cited by in F6Publishing: 29363] [Article Influence: 716.2] [Reference Citation Analysis (0)] |
| 23. | Montazeri A, Vahdaninia M, Ebrahimi M, Jarvandi S. The Hospital Anxiety and Depression Scale (HADS): translation and validation study of the Iranian version. Health Qual Life Outcomes. 2003;1:14. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 303] [Cited by in F6Publishing: 368] [Article Influence: 17.5] [Reference Citation Analysis (0)] |
| 24. | Available from: http://www.who.int/iris/handle/10665/43376. [Cited in This Article: ] |
| 25. | Global Atlas on Cardiovascular Disease Prevention and Control. Mendis S, Puska P, Norrving B editors. Geneva: World Health Organization (in collaboration with the World Heart Federation and World Stroke Organization) 2011; . [Cited in This Article: ] |
| 26. | Kawasaki T, Delea CS, Bartter FC, Smith H. The effect of high-sodium and low-sodium intakes on blood pressure and other related variables in human subjects with idiopathic hypertension. Am J Med. 1978;64:193-198. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 395] [Cited by in F6Publishing: 343] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 27. | Chiolero A, Würzner G, Burnier M. Renal determinants of the salt sensitivity of blood pressure. Nephrol Dial Transplant. 2001;16:452-458. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 32] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 28. | GenSalt Collaborative Research Group. GenSalt: rationale, design, methods and baseline characteristics of study participants. J Hum Hypertens. 2007;21:639-646. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 110] [Cited by in F6Publishing: 115] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 29. | van Paassen P, de Zeeuw D, de Jong PE, Navis G. Renin inhibition improves pressure natriuresis in essential hypertension. J Am Soc Nephrol. 2000;11:1813-1818. [PubMed] [Cited in This Article: ] |
| 30. | Aviv A, Hollenberg NK, Weder AB. Sodium glomerulopathy: tubuloglomerular feedback and renal injury in African Americans. Kidney Int. 2004;65:361-368. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 45] [Cited by in F6Publishing: 46] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 31. | de Wardener HE, He FJ, MacGregor GA. Plasma sodium and hypertension. Kidney Int. 2004;66:2454-2466. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 138] [Cited by in F6Publishing: 145] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 32. | Iwamoto T, Kita S, Zhang J, Blaustein MP, Arai Y, Yoshida S, Wakimoto K, Komuro I, Katsuragi T. Salt-sensitive hypertension is triggered by Ca2+ entry via Na+/Ca2+ exchanger type-1 in vascular smooth muscle. Nat Med. 2004;10:1193-1199. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 221] [Cited by in F6Publishing: 220] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 33. | Beeks E, Kessels AG, Kroon AA, van der Klauw MM, de Leeuw PW. Genetic predisposition to salt-sensitivity: a systematic review. J Hypertens. 2004;22:1243-1249. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 97] [Cited by in F6Publishing: 100] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 34. | Poch E, González D, Giner V, Bragulat E, Coca A, de La Sierra A. Molecular basis of salt sensitivity in human hypertension. Evaluation of renin-angiotensin-aldosterone system gene polymorphisms. Hypertension. 2001;38:1204-1209. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 143] [Cited by in F6Publishing: 150] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 35. | Hoffmann IS, Tavares-Mordwinkin R, Castejon AM, Alfieri AB, Cubeddu LX. Endothelial nitric oxide synthase polymorphism, nitric oxide production, salt sensitivity and cardiovascular risk factors in Hispanics. J Hum Hypertens. 2005;19:233-240. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 60] [Cited by in F6Publishing: 59] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 36. | Castejon AM, Alfieri AB, Hoffmann IS, Rathinavelu A, Cubeddu LX. Alpha-adducin polymorphism, salt sensitivity, nitric oxide excretion, and cardiovascular risk factors in normotensive Hispanics. Am J Hypertens. 2003;16:1018-1024. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 26] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 37. | Ramu P, Umamaheswaran G, Shewade DG, Swaminathan RP, Balachander J, Adithan C. Gly460Trp polymorphism of the ADD1 gene and essential hypertension in an Indian population: A meta-analysis on hypertension risk. Indian J Hum Genet. 2010;16:8-15. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 38. | Campese VM, Romoff MS, Levitan D, Saglikes Y, Friedler RM, Massry SG. Abnormal relationship between sodium intake and sympathetic nervous system activity in salt-sensitive patients with essential hypertension. Kidney Int. 1982;21:371-378. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 223] [Cited by in F6Publishing: 206] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 39. | Strazzullo P, Barba G, Cappuccio FP, Siani A, Trevisan M, Farinaro E, Pagano E, Barbato A, Iacone R, Galletti F. Altered renal sodium handling in men with abdominal adiposity: a link to hypertension. J Hypertens. 2001;19:2157-2164. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 94] [Cited by in F6Publishing: 96] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 40. | Schneider MP, Klingbeil AU, Schlaich MP, Langenfeld MR, Veelken R, Schmieder RE. Impaired sodium excretion during mental stress in mild essential hypertension. Hypertension. 2001;37:923-927. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 13] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 41. | Sadeghi M, Roohafza H, Afshar H, Rajabi F, Ramzani M, Shemirani H, Sarafzadeghan N. Relationship between depression and apolipoproteins A and B: a case-control study. Clinics (Sao Paulo). 2011;66:113-117. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 24] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 42. | Hall JE. Mechanisms of abnormal renal sodium handling in obesity hypertension. Am J Hypertens. 1997;10:49S-55S. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 144] [Cited by in F6Publishing: 95] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 43. | Hoffmann IS, Cubeddu LX. Increased blood pressure reactivity to dietary salt in patients with the metabolic syndrome. J Hum Hypertens. 2007;21:438-444. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 35] [Article Influence: 2.1] [Reference Citation Analysis (0)] |