Published online Sep 26, 2015. doi: 10.4330/wjc.v7.i9.555
Peer-review started: May 19, 2015
First decision: June 24, 2015
Revised: July 4, 2015
Accepted: July 29, 2015
Article in press: August 3, 2015
Published online: September 26, 2015
Electrical storm (ES) is a clinical condition characterized by three or more ventricular arrhythmia episodes leading to appropriate implantable cardioverter-defibrillator (ICD) therapies in a 24 h period. Mostly, arrhythmias responsible of ES are multiple morphologies of monomorphic ventricular tachycardia (VT), but polymorphic VT and ventricular fibrillation can also result in ES. Clinical presentation is very dramatic in most cases, strictly related to the cardiac disease that may worsen electrical and hemodynamic decompensation. Therefore ES management is challenging in the majority of cases and a high mortality is the rule both in the acute and in the long-term phases. Different underlying cardiomyopathies provide significant clues into the mechanism of ES, which can arise in the setting of structural arrhythmogenic cardiomyopathies or rarely in patients with inherited arrhythmic syndrome, impacting on pharmacological treatment, on ICD programming, and on the opportunity to apply strategies of catheter ablation. This latter has become a pivotal form of treatment due to its high efficacy in modifying the arrhythmogenic substrate and in achieving rhythm stability, aiming at reducing recurrences of ventricular arrhythmia and at improving overall survival. In this review, the most relevant epidemiological and clinical aspects of ES, with regard to the acute and long-term follow-up implications, were evaluated, focusing on these novel therapeutic strategies of treatment.
Core tip: Electrical storm is an increasingly common and life-threatening syndrome. The proper management of this arrhythmic emergency is related to a comprehensive assessment of each case. In this review we report all the essential aspects regarding the clinical and diagnostic evaluation, pharmacological treatment and, with special emphasis, catheter ablation approaches.
- Citation: Conti S, Pala S, Biagioli V, Giorno GD, Zucchetti M, Russo E, Marino V, Russo AD, Casella M, Pizzamiglio F, Catto V, Tondo C, Carbucicchio C. Electrical storm: A clinical and electrophysiological overview. World J Cardiol 2015; 7(9): 555-561
- URL: https://www.wjgnet.com/1949-8462/full/v7/i9/555.htm
- DOI: https://dx.doi.org/10.4330/wjc.v7.i9.555
Electrical storm (ES), also referred as arrhythmic storm, refers to a clinical condition characterized by 3 or more arrhythmia episodes of ventricular tachycardia (VT) or ventricular fibrillation (VF) leading to implantable cardioverter-defibrillator (ICD) therapies (Antitachycardia Pacing, ATP, or Direct Current shock, DC-shock), occurring over a single 24 h period[1]. ES represents an arrhythmic emergency that often affects patients at high risk of sudden cardiac death who previously underwent ICD implantation. In this setting ICD correctly interrupts VT/VF episodes; however ventricular arrhythmias, in terms of arrhythmogenic substrate, represent the gradual evolution of the underlying structural heart disease. In this review, we assess the most relevant epidemiological and clinical aspects of ES, with regard to the acute and long-term follow-up implications, focusing on novel therapeutic strategies of treatment.
The term ES was introduced in the 1990s to describe an instability condition, highly malignant, characterized by repetitive episodes of ventricular arrhythmias[2]. Nowadays, ES implies several appropriate ICD interventions aimed at terminating the arrhythmic episodes.
ES has been reported in 10%-40% of patients in secondary prevention whereas the incidence of ES is lower (3.5%-4%) in primary prevention[3-16]. However, the correct incidence of ES is uncertain due to several confounding factors such as population considered, type of cardiomyopathy, pharmacological therapy undertaken and other variables. In addition, most of the studies concerning ES incidence were retrospective thus including only the patients who survived the arrhythmic event.
ES mainly affects patients with advanced dilated cardiomyopathy, both ischemic and non-ischemic, representing the gradual evolution of the underlying arrhythmic substrate; however, ES may affect patients with different types of structural heart disease, such as valvular or congenital heart disease, as well as patients without structural heart disease (i.e., Brugada syndrome)[17].
The most significant predictors of ES are severe reduction of left ventricle (LV) function, advanced age and previous VT/VF episodes[8,10,11,13,18,19]. Monomorphic ventricular tachycardia is the most common arrhythmia documented in ES patients. VT episodes, hemodynamically unstable and interrupted with ATP or DC-shock, are the rule, with evidence of multiple VT morphologies[20]. Anyway, clinical presentation of ES is variable[9].
Less commonly, ES has been recorded in patients in whom premature ventricular complexes are the trigger of VT/VF both in acute myocardial infarction and in absence of structural heart disease[16,21]. The latter are often patients with “primitive ventricular fibrillation”, in whom the trigger of the arrhythmia has not been documented, presenting with multiple VF episodes after ICD implantation, mostly refractory to pharmacological therapy. Therefore, in this setting, the identification of ES triggers may be of interest in preventing VT/VF episodes, particularly in case of electrolyte disorder[9,14]. The role of adrenergic system in maintaining ES is of special interest as well; in terms of acute event treatment[7,16]. Adrenergic activation seems to play a key role in patients with arrhythmogenic right ventricular cardiomyopathy/dysplasia due to the well known arrhythmic sensitivity to adrenergic stimulation; although in the majority of these patients the trigger is unkown[22].
ES is an arrhythmic emergency related to recurrent consecutive episodes of ventricular arrhythmia, with low likelihood of spontaneous termination.
The clinical scenario of ES is the result of a combination of various factors: in patients with structural heart disease affected by chronic heart failure, ES causes worsening of heart failure with high risk of pulmonary edema/cardiogenic shock. These events are much more frequent and severe, less stable the arrhythmic condition and the functional status are. ICD therapies even if allow arrhythmic episodes termination and prevent sudden cardiac death, do not play any role in stabilizing the clinical scenario. Moreover, the continuous intervention of ICD, implies unfavorable hemodynamic effects[3], also resulting in psychological distress, adrenergic hyperactivity, and patient discomfort[22,23].
No reproducible data on acute mortality in ES are available. It should be reminded that acute mortality represents a common cause of death in patients with severe structural heart disease, in most of cases as cardiogenic shock or electromechanical dissociation in the setting of unmanageable arrhythmias[3]. Literature data show that patients with ES present an increased risk of sudden arrhythmic or cardiac death in the mid-term follow up[8-10,16,24]; furthermore, these findings were not confirmed just in few papers[7,13]. The MADIT II trial showed that patients with VT episodes interrupted by ICD have a significantly higher risk of sudden and non-sudden cardiac death. Moreover, patients who have survived ventricular arrhythmias have an increased risk of worsening heart failure and of mortality related to it[25]. Specifically, in the MADIT II trial, Sesselberg et al[11] have shown that ES is the most important independent predictor of mid-term cardiac death (increased risk of 7-fold), resulting particularly significant in the first 3 mo after ES (increasing risk of 18-fold). The results of SCD-HeFT trial are comparable, in addition, Poole et al[26] observed that not only appropriate shocks - directly related with arrhythmic events - but also inappropriate shocks impact on an increased mortality. More specifically the authors reported a significant increase of death in patients with appropriate (HR = 5.68; P < 0.001) and inappropriate shocks (HR = 1.98; P = 0.002). In particular, multiple shocks were associated with a 8-fold risk of death (HR = 8.23; P < 0.001).
These findings support the hypothesis that the recurrence of frequent arrhythmic events (and even more ES) strongly impacts on the evolution of patients’ clinical history, particularly by worsening the cardiac function. In this setting multiple shocks could have their own etiopathogenetic role related to repeated myocardial injury.
Patients with ES require a diagnostic evaluation of their structural heart disease, the type of arrhythmia and the presence of clinical triggers. The most common triggering factors are acute myocardial ischemia, electrolytic disorders and adverse drug effects. Identification of triggers is a key point: sometimes it allows the suppression of arrhythmias through simple therapeutic interventions, such as in case of hypokalaemia. Acute myocardial ischemia must be accurately identified and excluded through clinical and non-invasive diagnostic parameters. However, in most patients with coronary artery disease and previous history of myocardial infarction presenting with ES, myocardial ischemia is just a secondary effect of the arrhythmias. Myocardial ischemia should therefore be interpreted and consequently treated with the aid of pharmacological and/or interventional therapies in the presence of acute coronary syndrome. In the majority of cases, however, ES represents the evolution of an arrhythmogenic substrate in patients with previous VT/VF episodes.
Therapeutic interventions first depend on the arrhythmic pattern and on the hemodynamic stability of patients. ICD interrogation is the preliminary diagnostic step to evaluate the appropriateness of shock delivery and arrhythmic parameters (heart rate, electrogram analysis, trigger). ICD reprogramming is mandatory in order to both limit ICD shock delivery and attempt VT/VF interruption with antitachycardia pacing[27,28]. The accuracy of the diagnosis of ventricular arrhythmia may only occasionally show interpretative troubles in single-chamber ICD recipients in whom the comparison between basal and arrhythmic electrograms should be carried out carefully privileging reading from multiple recording channels.
ES patients require hospitalization. A continuous ECG and vital signs monitoring must be performed in the Coronary Intensive Care Unit or in a dedicated Emergency Arrhythmia Unit. During the evaluation phase, the possibility to document and characterize different morphologies of VT responsible for the clinical scenario is relevant, also with regard to a possible ablative treatment[20].
Hemodynamic and metabolic evaluations are needed in order to perform urgent interventions through intravenous therapies, such as inotropic agents or hydro-electrolytic infusion.
In the acute setting, prevention of arrhythmic recurrence should be as efficient as possible, by means of: (1) amiodarone is the first choice drug, unless contraindicated (presence of hyperthyroidism, long QT interval)[29]; (2) beta-blocker administration plays an important role because of its antiarrhythmic and antiadrenergic effect. Beta-blockers administration should be limited in patients with labile hemodynamic compensation or severe reduction of LV function; (3) lidocaina and azimilide are second choice drugs, useful in case of contraindications to previous medications[14,30]; (4) verapamile should be used as drug of choice in case of premature ventricular beats originating from His-Purkinje system; and (5) finally, atrial or sequential atrio-(bi)ventricular pacing are useful to avoid bradycardia[31,32].
Sedation is pivotal to stabilize patients with ES, but hemodynamic and/or respiratory instability can limit the use of sedation drugs, such as benzodiazepine. In these cases mechanical ventilation with oro-tracheal intubation are absolutely required in refractory forms of ES. In some cases mechanical ventilation allows safer drugs administration otherwise not tolerated.
The role of catheter ablation (CA) in patients with VT is becoming more and more relevant, as a definite treatment of multiple forms of arrhythmias and a complementary intervention in cases of high electrical instability, thus improving prognosis and quality of life in patients with advanced forms of heart disease. This observation creates the rationale to investigate the possibility to apply CA in patients with frequently recurring ventricular arrhythmias and ES[33].
Preliminary reports regarding the role of CA in the treatment of ES are limited to patients with specific clinical characteristics and/or small case series. Silva et al[34] reported a success rate of 80% in an ES population with recurrent hemodynamic stable VT; Schreieck et al[35] reported acute success in most of cases of a selected population undergoing CA of hemodynamic unstable arrhythmias guided by substrate mapping. Also Bänsch et al[16] described CA in patients with acute myocardial infarction and ES in whom VF was triggered by premature ventricular contractions, targeted by CA.
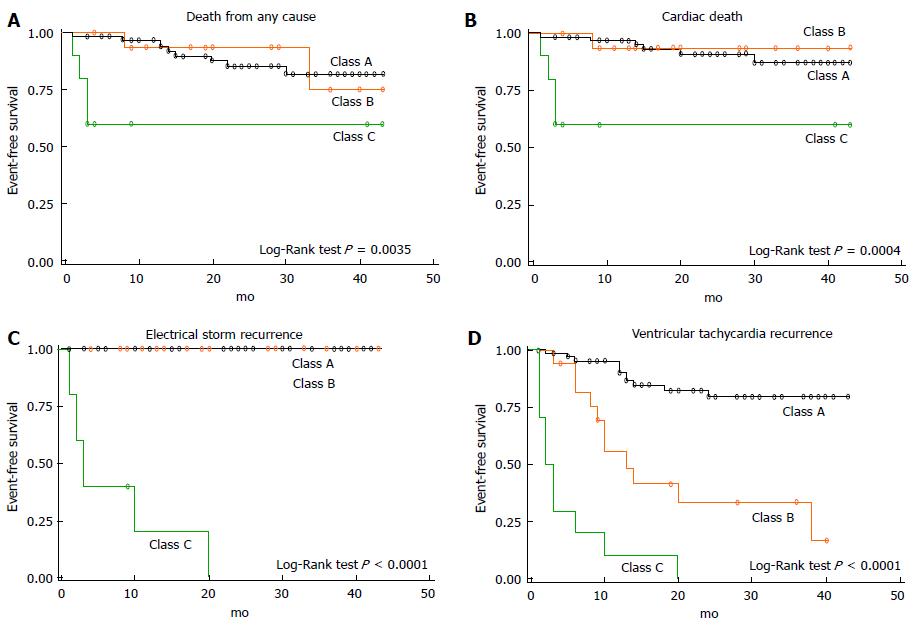
The ability to assess the feasibility and effectiveness of CA in a wider ES population arises from more recent experiences, which better represent the profile of patients with complex, hemodynamically non-tolerated, drug-refractory ventricular arrhythmias, mostly in the setting of structural heart disease with severe impairment of left ventricular function. In this population, Carbucicchio et al[20] have described for the first time VT suppression in 90% of patient undergoing one or more CA procedures with or without the use of haemodynamic mechanical support. Moreover, the authors have shown that non-inducibility of VT at the end of the procedure was predictive of no recurrence of ES or VT at 2 years follow-up; accordingly, CA survival was improved in arrhythmia-free patients (Figure 1). This experience once again shows that ES represents a turning point in the natural history of patients with dilated cardiomyopathy and ventricular arrhythmias and that the treatment of arrhythmic burden plays a favourable effect on the clinical history of these patients both in terms of arrhythmic death and acute heart failure. More recent studies have confirmed that CA of ES is effective in reducing mortality in the middle-term follow up[18,36].
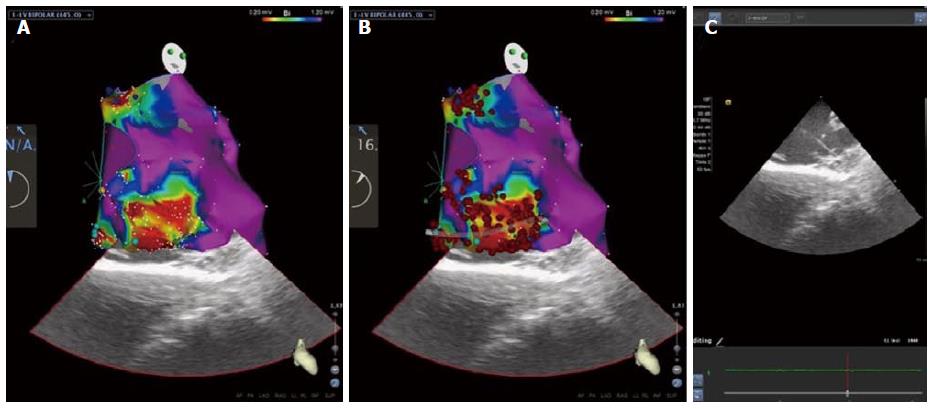
Regarding management of patients with ES or with recurrent VT following points must be taken in account: (1) clinical management in this setting is highly demanding. It requires an experienced Intensive Care Unit staff and a multidisciplinary approach that includes anesthesiological and psychological support; (2) advanced CA strategies in these patients are particularly complex (Figure 2). Obviously, the use of electroanatomical mapping (EAM) to guide CA is mandatory, and a substrate-guided approach is commonly more efficient, limiting activation mapping manoeuvres[37]. An epicardial approach should be preferred in all patients with non-ischemic cardiomyopathy to minimize recurrences. In patients with unstable VT or very depressed cardiac function, or in those presenting with cardiogenic shock, hemodynamic mechanical support allows patients stabilization and enhances efficacy and safety of CA, and can be used both during intraprocedurally as in the post-procedural period[38]; and (3) in selected patients, requiring concomitant surgical indications or in whom a percutaneous approach is not feasible, surgical ablation guided by EAM (endo- and/or epicardial) may be taken into account, in an experienced and multidisciplinary setting.
ES is an “extreme” ventricular arrhythmia affecting ICD patients with structural heart disease and is a major predictor of cardiac death in the short-term follow-up. Problems related to the treatment of ES patients are complex, depending on the type of patient as well as on the treatment of cardiac emergency, and require high standard facilities and specialized skills.
CA for the treatment of ES is particularly promising and should be considered the elective form of treatment to achieve long-term rhythm stabilization and to prevent heart failure. The possibility to modify the arrhythmic substrate by CA in an early phase, thus preventing critical situations deriving from repetitive ICD interventions, looks promising, but necessitates further corroborations.
P- Reviewer: Falconi M, Said SAM, Sakabe K S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | Natale A, Raviele A, Al-Ahmad A, Alfieri O, Aliot E, Almendral J, Breithardt G, Brugada J, Calkins H, Callans D. Venice Chart International Consensus document on ventricular tachycardia/ventricular fibrillation ablation. J Cardiovasc Electrophysiol. 2010;21:339-379. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 79] [Cited by in F6Publishing: 86] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 2. | Kowey PR. An overview of antiarrhythmic drug management of electrical storm. Can J Cardiol. 1996;12 Suppl B:3B-8B; discussion 27B-28B. [PubMed] [Cited in This Article: ] |
| 3. | Mitchell LB, Pineda EA, Titus JL, Bartosch PM, Benditt DG. Sudden death in patients with implantable cardioverter defibrillators: the importance of post-shock electromechanical dissociation. J Am Coll Cardiol. 2002;39:1323-1328. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 164] [Cited by in F6Publishing: 171] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 4. | Zipes DP, Camm AJ, Borggrefe M, Buxton AE, Chaitman B, Fromer M, Gregoratos G, Klein G, Moss AJ, Myerburg RJ. ACC/AHA/ESC 2006 guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: a report of the American College of Cardiology/American Heart Association Task Force and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Develop Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death). J Am Coll Cardiol. 2006;48:e247-e346. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 916] [Cited by in F6Publishing: 863] [Article Influence: 47.9] [Reference Citation Analysis (0)] |
| 5. | Villacastín J, Almendral J, Arenal A, Albertos J, Ormaetxe J, Peinado R, Bueno H, Merino JL, Pastor A, Medina O. Incidence and clinical significance of multiple consecutive, appropriate, high-energy discharges in patients with implanted cardioverter-defibrillators. Circulation. 1996;93:753-762. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 103] [Cited by in F6Publishing: 105] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 6. | Credner SC, Klingenheben T, Mauss O, Sticherling C, Hohnloser SH. Electrical storm in patients with transvenous implantable cardioverter-defibrillators: incidence, management and prognostic implications. J Am Coll Cardiol. 1998;32:1909-1915. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 263] [Cited by in F6Publishing: 246] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 7. | Greene M, Newman D, Geist M, Paquette M, Heng D, Dorian P. Is electrical storm in ICD patients the sign of a dying heart? Outcome of patients with clusters of ventricular tachyarrhythmias. Europace. 2000;2:263-269. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 94] [Cited by in F6Publishing: 90] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 8. | Exner DV, Pinski SL, Wyse DG, Renfroe EG, Follmann D, Gold M, Beckman KJ, Coromilas J, Lancaster S, Hallstrom AP. Electrical storm presages nonsudden death: the antiarrhythmics versus implantable defibrillators (AVID) trial. Circulation. 2001;103:2066-2071. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 258] [Cited by in F6Publishing: 242] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 9. | Verma A, Kilicaslan F, Marrouche NF, Minor S, Khan M, Wazni O, Burkhardt JD, Belden WA, Cummings JE, Abdul-Karim A. Prevalence, predictors, and mortality significance of the causative arrhythmia in patients with electrical storm. J Cardiovasc Electrophysiol. 2004;15:1265-1270. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 120] [Cited by in F6Publishing: 126] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 10. | Gatzoulis KA, Andrikopoulos GK, Apostolopoulos T, Sotiropoulos E, Zervopoulos G, Antoniou J, Brili S, Stefanadis CI. Electrical storm is an independent predictor of adverse long-term outcome in the era of implantable defibrillator therapy. Europace. 2005;7:184-192. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 116] [Cited by in F6Publishing: 123] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 11. | Sesselberg HW, Huang DT, Zareba W, Andrews M, McNitt S, McClinitic B, Daubert J, Moss AJ. Storms of ventricular tachycardia/fibrillation in MADIT II patients. Heart Rhythm. 2005;2:S205. [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 12. | Arya A, Haghjoo M, Dehghani MR, Fazelifar AF, Nikoo MH, Bagherzadeh A, Sadr-Ameli MA. Prevalence and predictors of electrical storm in patients with implantable cardioverter-defibrillator. Am J Cardiol. 2006;97:389-392. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 66] [Cited by in F6Publishing: 59] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 13. | Brigadeau F, Kouakam C, Klug D, Marquié C, Duhamel A, Mizon-Gérard F, Lacroix D, Kacet S. Clinical predictors and prognostic significance of electrical storm in patients with implantable cardioverter defibrillators. Eur Heart J. 2006;27:700-707. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 89] [Cited by in F6Publishing: 97] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 14. | Hohnloser SH, Al-Khalidi HR, Pratt CM, Brum JM, Tatla DS, Tchou P, Dorian P. Electrical storm in patients with an implantable defibrillator: incidence, features, and preventive therapy: insights from a randomized trial. Eur Heart J. 2006;27:3027-3032. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 120] [Cited by in F6Publishing: 115] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 15. | Fries R, Heisel A, Huwer H, Nikoloudakis N, Jung J, Schäfers HJ, Schieffer H, Ozbek C. Incidence and clinical significance of short-term recurrent ventricular tachyarrhythmias in patients with implantable cardioverter-defibrillator. Int J Cardiol. 1997;59:281-284. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 25] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 16. | Bänsch D, Böcker D, Brunn J, Weber M, Breithardt G, Block M. Clusters of ventricular tachycardias signify impaired survival in patients with idiopathic dilated cardiomyopathy and implantable cardioverter defibrillators. J Am Coll Cardiol. 2000;36:566-573. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 97] [Cited by in F6Publishing: 106] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 17. | Chalvidan T, Deharo JC, Dieuzaide P, Defaye P, Djiane P. Near fatal electrical storm in a patient equipped with an implantable cardioverter defibrillator for Brugada syndrome. Pacing Clin Electrophysiol. 2000;23:410-412. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 22] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 18. | Arya A, Bode K, Piorkowski C, Bollmann A, Sommer P, Gaspar T, Wetzel U, Husser D, Kottkamp H, Hindricks G. Catheter ablation of electrical storm due to monomorphic ventricular tachycardia in patients with nonischemic cardiomyopathy: acute results and its effect on long-term survival. Pacing Clin Electrophysiol. 2010;33:1504-1509. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 46] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 19. | Streitner F, Kuschyk J, Veltmann C, Mahl E, Dietrich C, Schimpf R, Doesch C, Streitner I, Wolpert C, Borggrefe M. Predictors of electrical storm recurrences in patients with implantable cardioverter-defibrillators. Europace. 2011;13:668-674. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 26] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 20. | Carbucicchio C, Santamaria M, Trevisi N, Maccabelli G, Giraldi F, Fassini G, Riva S, Moltrasio M, Cireddu M, Veglia F. Catheter ablation for the treatment of electrical storm in patients with implantable cardioverter-defibrillators: short- and long-term outcomes in a prospective single-center study. Circulation. 2008;117:462-469. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 324] [Cited by in F6Publishing: 338] [Article Influence: 21.1] [Reference Citation Analysis (0)] |
| 21. | Haïssaguerre M, Shoda M, Jaïs P, Nogami A, Shah DC, Kautzner J, Arentz T, Kalushe D, Lamaison D, Griffith M. Mapping and ablation of idiopathic ventricular fibrillation. Circulation. 2002;106:962-967. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 502] [Cited by in F6Publishing: 438] [Article Influence: 19.9] [Reference Citation Analysis (0)] |
| 22. | Israel CW, Barold SS. Electrical storm in patients with an implanted defibrillator: a matter of definition. Ann Noninvasive Electrocardiol. 2007;12:375-382. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 82] [Cited by in F6Publishing: 88] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 23. | Nademanee K, Taylor R, Bailey WE, Rieders DE, Kosar EM. Treating electrical storm: sympathetic blockade versus advanced cardiac life support-guided therapy. Circulation. 2000;102:742-747. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 323] [Cited by in F6Publishing: 294] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 24. | Pacifico A, Ferlic LL, Cedillo-Salazar FR, Nasir N, Doyle TK, Henry PD. Shocks as predictors of survival in patients with implantable cardioverter-defibrillators. J Am Coll Cardiol. 1999;34:204-210. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 49] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 25. | Goldenberg I, Moss AJ, McNitt S, Zareba W, Andrews ML, Hall WJ, Greenberg H, Case RB. Relations among renal function, risk of sudden cardiac death, and benefit of the implanted cardiac defibrillator in patients with ischemic left ventricular dysfunction. Am J Cardiol. 2006;98:485-490. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 162] [Cited by in F6Publishing: 139] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 26. | Poole JE, Johnson GW, Hellkamp AS, Anderson J, Callans DJ, Raitt MH, Reddy RK, Marchlinski FE, Yee R, Guarnieri T. Prognostic importance of defibrillator shocks in patients with heart failure. N Engl J Med. 2008;359:1009-1017. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1126] [Cited by in F6Publishing: 1078] [Article Influence: 67.4] [Reference Citation Analysis (0)] |
| 27. | Huang DT, Traub D. Recurrent ventricular arrhythmia storms in the age of implantable cardioverter defibrillator therapy: a comprehensive review. Prog Cardiovasc Dis. 2008;51:229-236. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 40] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 28. | Santomauro M, Duilio C, Tecchia LB, Di Mauro P, Iapicca G, Auricchio L, Filardi PP. Management of electrical storm in implantable cardioverter-defibrillator recipients. G Ital Cardiol (Rome). 2010;11:37S-41S. [PubMed] [Cited in This Article: ] |
| 29. | Kowey PR, Levine JH, Herre JM, Pacifico A, Lindsay BD, Plumb VJ, Janosik DL, Kopelman HA, Scheinman MM. Randomized, double-blind comparison of intravenous amiodarone and bretylium in the treatment of patients with recurrent, hemodynamically destabilizing ventricular tachycardia or fibrillation. The Intravenous Amiodarone Multicenter Investigators Group. Circulation. 1995;92:3255-3263. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 201] [Cited by in F6Publishing: 206] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 30. | Fuchs T, Groysman R, Meilichov I. Use of a combination of class III and class Ic antiarrhythmic agents in patients with electrical storm. Pharmacotherapy. 2008;28:14-19. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 31. | Nordbeck P, Seidl B, Fey B, Bauer WR, Ritter O. Effect of cardiac resynchronization therapy on the incidence of electrical storm. Int J Cardiol. 2010;143:330-336. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 23] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 32. | Gasparini M, Lunati M, Landolina M, Santini M, Padeletti L, Perego G, Vincenti A, Curnis A, Carboni A, Denaro A. Electrical storm in patients with biventricular implantable cardioverter defibrillator: incidence, predictors, and prognostic implications. Am Heart J. 2008;156:847-854. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 24] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 33. | Kuck KH, Schaumann A, Eckardt L, Willems S, Ventura R, Delacrétaz E, Pitschner HF, Kautzner J, Schumacher B, Hansen PS. Catheter ablation of stable ventricular tachycardia before defibrillator implantation in patients with coronary heart disease (VTACH): a multicentre randomised controlled trial. Lancet. 2010;375:31-40. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 551] [Cited by in F6Publishing: 533] [Article Influence: 38.1] [Reference Citation Analysis (0)] |
| 34. | Silva RM, Mont L, Nava S, Rojel U, Matas M, Brugada J. Radiofrequency catheter ablation for arrhythmic storm in patients with an implantable cardioverter defibrillator. Pacing Clin Electrophysiol. 2004;27:971-975. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 46] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 35. | Schreieck J, Zrenner B, Deisenhofer I, Schmitt C. Rescue ablation of electrical storm in patients with ischemic cardiomyopathy: a potential-guided ablation approach by modifying substrate of intractable, unmappable ventricular tachycardias. Heart Rhythm. 2005;2:10-14. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 43] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 36. | Peichl P, Cihák R, Kozeluhová M, Wichterle D, Vancura V, Kautzner J. Catheter ablation of arrhythmic storm triggered by monomorphic ectopic beats in patients with coronary artery disease. J Interv Card Electrophysiol. 2010;27:51-59. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 44] [Cited by in F6Publishing: 43] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 37. | Carbucicchio C, Ahmad Raja N, Di Biase L, Volpe V, Dello Russo A, Trivedi C, Bartoletti S, Zucchetti M, Casella M, Russo E. High-density substrate-guided ventricular tachycardia ablation: role of activation mapping in an attempt to improve procedural effectiveness. Heart Rhythm. 2013;10:1850-1858. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 26] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 38. | Carbucicchio C, Della Bella P, Fassini G, Trevisi N, Riva S, Giraldi F, Baratto F, Marenzi G, Sisillo E, Bartorelli A. Percutaneous cardiopulmonary support for catheter ablation of unstable ventricular arrhythmias in high-risk patients. Herz. 2009;34:545-552. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 32] [Article Influence: 2.3] [Reference Citation Analysis (0)] |