Published online Aug 27, 2012. doi: 10.4240/wjgs.v4.i8.199
Revised: July 29, 2012
Accepted: August 2, 2012
Published online: August 27, 2012
Haemangiomas are the most common solitary benign neoplasm of the liver with an incidence ranging from 5% to 20%. Although usually small and asymptomatic, they may reach considerable proportions and rarely give rise to life-threatening complications. Surgical intervention is required for incapacitating symptoms, established complications, and diagnostic uncertainty. The resection of haemangiomas demands meticulous surgical technique, owing to their high vascularity and the concomitant risk of intra-operative haemorrhage. Laparoscopic resection of giant haemangiomas is even more challenging, and has only been reported twice. We here report the case of a giant 10 cm liver haemangioma which was successfully resected laparoscopically using the laparoscopic HabibTM 4×, a bipolar radiofrequency device, without clamping major vessels and with minimal blood loss. Transfusion of blood or blood products was not required. The patient had an uneventful recovery and was asymptomatic at 7-mo follow-up.
- Citation: Acharya M, Panagiotopoulos N, Bhaskaran P, Kyriakides C, Pai M, Habib N. Laparoscopic resection of a giant exophytic liver haemangioma with the laparoscopic Habib 4× radiofrequency device. World J Gastrointest Surg 2012; 4(8): 199-202
- URL: https://www.wjgnet.com/1948-9366/full/v4/i8/199.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v4.i8.199
Haemangiomas are the most common benign liver tumours[1], the majority representing incidental findings on routine abdominal imaging. Giant haemangiomas however, defined as those exceeding 5 cm in diameter, may present with abdominal pain, nausea, vomiting, or obstructive jaundice[2]. They often necessitate an extended hepatectomy with the associated risk of massive intra-operative haemorrhage.
Laparoscopic surgery for liver haemangiomas is further compounded by the significant difficulty in controlling bleeding when it occurs. Nevertheless, the laparoscopic Habib™ 4X[3,4] (LH4X) (Angiodynamics, Inc., NY, Uinted States), a recently-developed bipolar radiofrequency device which reduces blood loss in laparoscopic liver resection, has demonstrated encouraging results.
We here present the case of a symptomatic 37-year-old woman who underwent successful laparoscopic resection of a giant exophytic liver haemangioma using the LH4X bipolar resection device.
A 37-year-old woman was referred to our department with a six-month history of epigastric pain radiating to the right upper quadrant, associated with dyspepsia and weight loss. There was no past medical history of note, no risk factors for viral hepatitis and no family history of liver disease. She did not drink alcohol or smoke tobacco. Physical examination revealed epigastric fullness and tenderness on deep palpation; she had no splenomegaly, scleral jaundice or other stigmata of hepatobiliary disease.
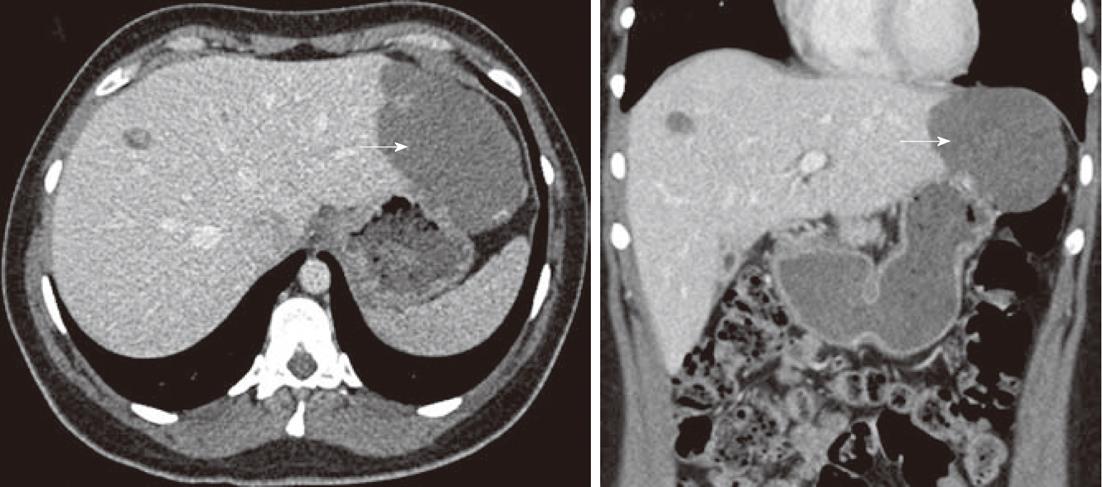
Laboratory investigations showed: haemoglobin 12 g/dL, white cell count 7.6 × 109/L, platelets 353 × 109/L, C-reactive protein 143 mg/L, bilirubin 6 μmol/L, alanine transaminase 76 IU/L, alkaline phosphatase 52 IU/L, gamma glutamyl transpeptidase 19 IU/L, albumin 42 g/L, prothrombin time 10.9 s, and fibrinogen 5.4 g/L. Computed tomography (CT) scan of the abdomen (Figure 1) demonstrated a 10 cm exophytic lesion within segments 2 and 3 of the liver, consistent with a haemangioma, which was displacing the lesser curve of the stomach. Six other smaller haemangiomas (0.5 cm to 1.5 cm) were also noted throughout the rest of the liver.
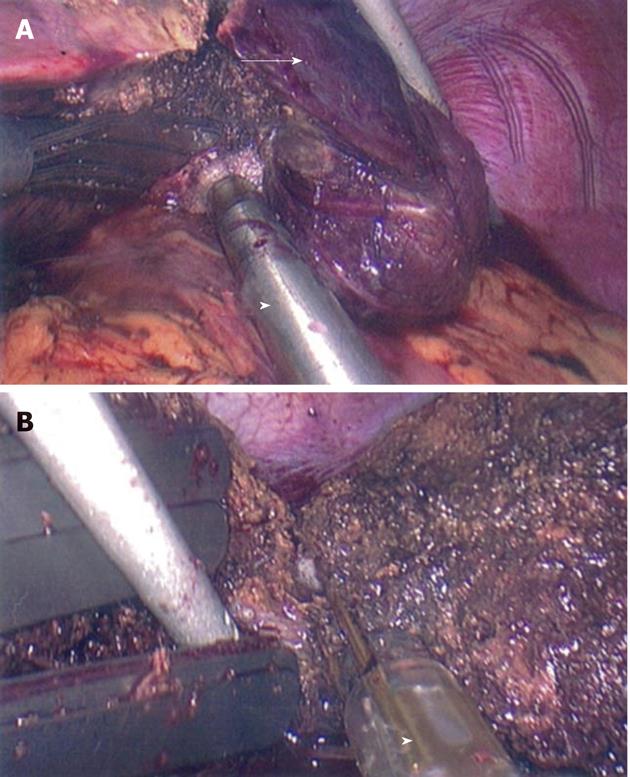
A decision was made to operate in view of the patient’s symptoms after discussion at the multi-disciplinary meeting. At laparoscopy, the left lobe of the liver was mobilised by division of the left triangular ligament. A resection line was demarcated with diathermy after identification of the larger 10 cm haemangioma using intra-operative ultrasound. The LH4X (Figure 2) was introduced into the peritoneal cavity via the 10 mm epigastric port. Radiofrequency energy was applied along the pre-determined line, at small intervals, to induce hyperthermic coagulative necrosis. After each application of radiofrequency energy, laparoscopic dissection scissors were used for progressive transection. The surgical specimen (Figure 3) was then extracted using the Endo Catch™ Specimen Retrieval System (Autosuture, United States Surgical Corporation, Norwalk, CT). A 20F drain was placed adjacent to the resection margin. Operative time was 90 min, and total blood loss was less than 50 mL. Transfusion of blood or blood products was not required.
The patient had an uneventful recovery and was discharged five days later. Histopathological examination of the resected lesion revealed a cavernous haemangioma with areas of thrombosis and recanalization, with only reactive changes in the background liver. The patient was asymptomatic at 7 mo follow-up, when CT scanning demonstrated the radiofrequency resection margin with normal appearances of the rest of the liver and unchanged dimensions of the smaller haemangiomas.
Haemangiomas are the most common solitary benign neoplasm of the liver with an incidence ranging from 5% to 20%[1]. They are commonly diagnosed between the ages of 40 and 60 years, and are 3 to 5 times more frequent in women[5]. Macroscopically, haemangiomas are hypervascular and compressible lesions, with a well-defined ring of compressed liver parenchyma separating them from normal tissue[6]. They may present as an exophytic growth, whereby the tumour originates from the liver, but its centre lies beyond the confines of the liver[6].
Smaller tumours seldom produce symptoms, remain stable in size[7] and do not require long-term surveillance or specific treatment[8]. Giant haemangiomas however may be complicated by intra-lesional thrombosis, infarction, spontaneous or traumatic rupture, or a consumptive coagulopathy known as Kasabach-Merritt syndrome[2,9].
Surgical intervention for giant haemangioma is warranted for established complications, severe symptomatic disease and diagnostic uncertainty, particularly regarding malignancy[2,10,11]. In such circumstances, surgical management options include liver resection, enucleation, hepatic artery ligation and liver transplantation. Enucleation is the preferred treatment option for anterior and superficial haemangiomas, achieving low mortality, reduced intra-operative blood loss and bile leak rates, and optimal preservation of hepatic parenchymal function[12-14]. Partial liver resection should be considered for larger haemangiomas in peripheral segments, whilst multiple or giant haemangiomas may necessitate extended hepatectomy[3].
Tumour size in patients with giant liver haemangiomas has been shown to be highly correlated with intra-operative blood loss[15], which in turn influences post-operative outcome. In one study, patients with haemangiomas exceeding 10 cm in size required an average of 15 units of blood transfusion[15]. Liver surgery has traditionally been associated with a high risk of intra-operative haemorrhage and the requirement for numerous blood transfusions. Open liver resection for haemangioma represents an even greater bleeding hazard, owing to the intrinsic hypervascularity and soft texture of the tumour. Laparoscopic liver surgery, whilst offering patients the benefits of a more conservative incision, further greatly increases the potential for significant haemorrhagic complications, since effective haemostasis is impeded within the tight confines of a closed abdomen.
The LH4X is a bipolar radiofrequency device that minimises blood loss during laparoscopic liver resection[3]. It consists of a 5 cm long, 2 × 2 rectangular array of electrodes mounted on a 45 cm shaft, which is introduced via a 10-12 mm laparoscopic port. The device uses up to 250 Watts of radiofrequency power to induce coagulative necrosis along an intended line of parenchymal transection. The LH4X device thus allows laparoscopic liver resection to be performed safely, without clamping of major vessels, and with minimal blood loss. In our patient, operative blood loss was less than 50 mL; Pringle manoeuvre or hepatic inflow occlusion was not necessary.
Laparoscopic resection of a giant liver haemangioma has only been reported twice before in medical literature[16,17]. Lanthaler et al[16] performed pre-operative hepatic arterial embolisation followed by hepatic parenchymal transection of a 20 cm liver haemangioma using harmonic scalpel (Ethicon, Cincinatti, OH). There was no significant blood loss. Our patient, however, did not undergo selective arterial embolisation pre-operatively. Gadiyaram et al[17] recently described the successful laparoscopic resection of an 18 cm liver haemangioma utilising the LH4X probe for parenchymal transection with 50 mL blood loss.
In conclusion, we describe the successful laparoscopic resection of a giant 10 cm haemangioma using the LH4X bipolar resection device. Whilst the laparoscopic resection of giant haemangiomas mandates meticulous surgical technique, owing to the significant risk of intra-operative haemorrhage and difficulty in achieving haemostasis, careful application of the LH4X device minimises blood loss, thus avoiding transfusion and facilitating enhanced patient outcomes.
Peer reviewer: Calogero Iacono, Professor, Department of Surgery, University of Verona Medical School, University Hospital "GB Rossi", 37134 Verona, Italy
S- Editor Song XX L- Editor A E- Editor Xiong L
| 1. | Koszka AJ, Ferreira FG, de Aquino CG, Ribeiro MA, Gallo AS, Aranzana EM, Szutan LA. Resection of a rapid-growing 40-cm giant liver hemangioma. World J Hepatol. 2010;2:292-294. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 2. | Duxbury MS, Garden OJ. Giant haemangioma of the liver: observation or resection? Dig Surg. 2010;27:7-11. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 47] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 3. | Ayav A, Jiao LR, Habib NA. Bloodless liver resection using radiofrequency energy. Dig Surg. 2007;24:314-317. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 30] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Pai M, Navarra G, Ayav A, Sommerville C, Khorsandi SK, Damrah O, Jiao LR, Habib NA. Laparoscopic Habib 4X: a bipolar radiofrequency device for bloodless laparoscopic liver resection. HPB (Oxford). 2008;10:261-264. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 22] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 5. | Berloco P, Bruzzone P, Mennini G, Della Pietra F, Iappelli M, Novelli G, Rossi M. Giant hemangiomas of the liver: surgical strategies and technical aspects. HPB (Oxford). 2006;8:200-201. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Bader TR, Braga L, Semelka RC. Exophytic benign tumors of the liver: appearance on MRI. Magn Reson Imaging. 2001;19:623-628. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 27] [Article Influence: 1.2] [Reference Citation Analysis (1)] |
| 7. | Yamagata M, Kanematsu T, Matsumata T, Utsunomiya T, Ikeda Y, Sugimachi K. Management of haemangioma of the liver: comparison of results between surgery and observation. Br J Surg. 1991;78:1223-1225. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 40] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Erdogan D, Busch OR, van Delden OM, Bennink RJ, ten Kate FJ, Gouma DJ, van Gulik TM. Management of liver hemangiomas according to size and symptoms. J Gastroenterol Hepatol. 2007;22:1953-1958. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 56] [Cited by in F6Publishing: 57] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 9. | Hall GW. Kasabach-Merritt syndrome: pathogenesis and management. Br J Haematol. 2001;112:851-862. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 215] [Cited by in F6Publishing: 178] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 10. | Choi J, Lee YJ, Hwang DW, Chon SH, Nagpal A, Park KM. Surgical treatment of giant hepatic hemangiomas: technical point of view. Am Surg. 2011;77:48-54. [PubMed] [Cited in This Article: ] |
| 11. | Uetama T, Yoshida H, Hirakata A, Yokoyama T, Maruyama H, Suzuki S, Matsutani T, Matsushita A, Sasajima K, Uchida E. A symptomatic giant hepatic hemangioma treated with hepatectomy. J Nippon Med Sch. 2011;78:34-39. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 12. | Popescu I, Ciurea S, Brasoveanu V, Hrehoret D, Boeti P, Georgescu S, Tulbure D. Liver hemangioma revisited: current surgical indications, technical aspects, results. Hepatogastroenterology. 2001;48:770-776. [PubMed] [Cited in This Article: ] |
| 13. | Ozden I, Emre A, Alper A, Tunaci M, Acarli K, Bilge O, Tekant Y, Ariogul O. Long-term results of surgery for liver hemangiomas. Arch Surg. 2000;135:978-981. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 57] [Cited by in F6Publishing: 52] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 14. | Kuo PC, Lewis WD, Jenkins RL. Treatment of giant hemangiomas of the liver by enucleation. J Am Coll Surg. 1994;178:49-53. [PubMed] [Cited in This Article: ] |
| 15. | Hanazaki K, Kajikawa S, Matsushita A, Monma T, Hiraguri M, Koide N, Nimura Y, Adachi W, Amano J. Giant cavernous hemangioma of the liver: is tumor size a risk factor for hepatectomy? J Hepatobiliary Pancreat Surg. 1999;6:410-413. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 19] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 16. | Lanthaler M, Freund M, Nehoda H. Laparoscopic resection of a giant liver hemangioma. J Laparoendosc Adv Surg Tech A. 2005;15:624-626. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 18] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 17. | Gadiyaram S, Shetty N. Laparoscopic resection of giant liver hemangioma using laparoscopic Habib probe for parenchymal transection. J Minim Access Surg. 2012;8:59-61. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |