Published online Sep 15, 2017. doi: 10.4239/wjd.v8.i9.436
Peer-review started: January 23, 2017
First decision: April 14, 2017
Revised: May 9, 2017
Accepted: May 30, 2017
Article in press: May 31, 2017
Published online: September 15, 2017
To determine if retinal and foot checks are carried out on patients with diabetes receiving haemodialysis.
Eighty-four patients with diabetes receiving haemodialysis were asked if they recalled having eye and foot screening in the last year, and if so, by whom was the check done.
Seventy-seven (91.7%) patients recalled having an eye check in the preceding 12 mo. Of these, 52 (67.5%) did so in an ophthalmology clinic, 17 (22%) in retinal screening, three (3.9%) in an optician clinic. Three patients (3.9%) went to both ophthalmology and retinal screening, and two (2.6%) attended an ophthalmology and optician. Seventy (83.3%) patients recalled having a foot check in the preceding 12 mo. Of these, 33 (47.1%) were done by practice nurse, 14 (20%) by a diabetes nurse, 11 (15.7%) by a general practitioner, eight (11.4%) by a chiropodist, and four (5.7%) were each checked by renal nurse, diabetes consultant, junior doctor, or unknown person at a foot clinic.
Most patients with diabetes on haemodialysis are able to recall having an eye check in the last year, although 8.3% could not. A significant proportion of patients could not recall having a foot check (16.7%) in the last year. This baseline audit suggests that an improvement in the rate of foot screening is important to achieve in patients with diabetes on haemodialysis in our unit.
Core tip: Diabetes is the commonest cause of end stage renal failure in many countries. Patients with diabetes on haemodialysis are at high risk of retinal and foot problems, and need regular screening to ensure they do not develop problems related to these complications. Our survey suggests that most patients are getting eye checks, but a significant number are not getting foot checks. This is an important area for all dialysis units to consider. We recommend that patients have foot screening whilst on dialysis, which may require further training for dialysis nurses.
- Citation: Mothojakan NB, Hussain S, McCafferty K, Yaqoob MM, Chowdhury TA. Eye and foot checks in patients with diabetes on haemodialysis: Are they done, and who does them? World J Diabetes 2017; 8(9): 436-439
- URL: https://www.wjgnet.com/1948-9358/full/v8/i9/436.htm
- DOI: https://dx.doi.org/10.4239/wjd.v8.i9.436
Diabetic nephropathy is the leading cause of end-stage renal failure in the United Kingdom[1]. Screening programmes enable detection of early changes associated with microvascular complications of diabetes, including diabetic retinopathy and peripheral neuropathy. Many national guidelines recommend that all patients with diabetes have yearly screening of feet and eyes to reduce the risk of blindness and avoidable limb amputations[2,3]. With the increasing prevalence of diabetes, attendance at screening programmes is of the utmost importance in order to reduce the risk of complications.
Patients with diabetes who have end stage renal failure (ESRF) on regular haemodialysis attend hospital for dialysis very frequently, and as a result find it difficult to attend other appointments. We have previously noted poor attendance to other clinics and appointments in patients on haemodialysis. East London is an area of high social deprivation, and many patients are elderly, with multiple co-morbidities, whose first language is often not English, and these factors may affect their ability to access healthcare[4]. Patients with diabetes on haemodialysis are at particular risk of foot and eye problems[5]. Microvascular complications of diabetes arise due to poor glycaemic control, and indeed haemodialysis patients with poor glycaemic control have been found to have poorer survival compared to those with good glycaemic control[6].
Recent United Kingdom guidelines highlight the need for annual foot and eye screening for patients with diabetes on haemodialysis[4]. The aim of this study was to determine if patients with diabetes on our haemodialysis unit could recall having retinal screening and foot surveillance in the past year, and to find out who had performed this.
This retrospective study was carried out on the dialysis unit of the Royal London Hospital, a tertiary centre which serves a large cohort of renal patients in East London, United Kingdom. A brief questionnaire was designed for patients with diabetes receiving dialysis, asking whether patients recalled having “a diabetes eye check” or “diabetes foot check” in the past 12 mo. Patients who had received a diabetes eye check were asked where this had taken place: At an optician, eye clinic, retinal screening service or elsewhere. Patients who had a diabetes foot check where asked who had performed the procedure; a doctor, diabetes nurse, renal nurse or podiatrist.
Participants were recruited to the study from August to September 2015, whilst receiving haemodialysis on the renal unit. Inclusion criteria for the study included: Patient currently receiving haemodialysis, patient was diagnosed with diabetes for at least a year and able to receive care in the community. Patients were excluded from the study if they had communication difficulties.
All statistical analysis and graphs were performed using GraphPad Prism 7 (GraphPad software inc, California, United States) software. Quantitative data were expressed as frequencies or mean ± SD as appropriate. Qualitative data were expressed as frequencies.
Eighty-four patients met the inclusion criteria and agreed to participate in the study. Patient characteristics are shown in Table 1. Sixty point seven percent of the participants were male and 39.3% were female. The mean age of the cohort was 63.9 ± 10.35 years. Insulin only therapy was used by 53.6% of the participants. The remaining participants were diet-controlled (11.9%), on medication only (19%) or medication and insulin (15.5%).
| Variables | Patients |
| Gender | |
| Male | 51 (60.7) |
| Female | 33 (39.3) |
| Age (mean ± SD) | 63.9 ± 10.35 |
| Ethnicity | |
| African - Caribbean | 38 (45.2) |
| Asian - Bangladeshi | 22 (26.2) |
| Asian - Indian | 4 (4.8) |
| Asian - Pakistani | 2 (2.4) |
| Asian - Other | 4 (4.8) |
| White - British | 9 (10.7) |
| White - Other | 2 (2.4) |
| Other | 3 (3.6) |
| Treatment regimen | |
| Diet only treated | 10 (11.9) |
| Oral hypoglycaemic only treated | 16 (19.0) |
| Insulin + oral hypoglycaemic treated | 13 (15.5) |
| Insulin only treated | 45 (53.6) |
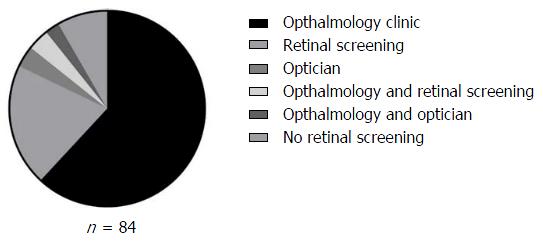
Figure 1 shows eye check uptake in the patients surveyed. Seventy-seven (91.7%) of patients reported having an eye check in the last 12 mo. Of these, 52 (67.5%) did so in an ophthalmology clinic, 17 (22%) in retinal screening, three (3.9%) in an optician, three (3.9%) went to both ophthalmology and retinal screening, and two (2.6%) attended an ophthalmology and optician.
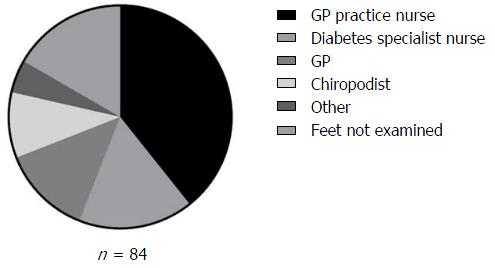
Figure 2 shows foot check uptake in the patients surveyed. Seventy (83.3%) patients recalled having a foot check in the previous 12 mo. Of these, 33 (47.1%) were carried out by a practice nurse, 14 (20%) by a diabetes specialist nurse, 11 (15.7%) by the general practitioner (GP), eight (11.4%) by a chiropodist, and four (5.7%) had been a renal nurse, a diabetes consultant, a junior doctor, or unknown person at a foot clinic.
Screening programmes have an important role in the prevention and early detection of retinopathy and neuropathy. We are unaware of any previous studies investigating the uptake of screening programmes in haemodialysis patients. In the United Kingdom in 2012-2013, 80.2% of patients offered diabetic eye screening attended. Recent recommendations suggest that is should be possible for a minimum of 85% of those offered digital retinal screening to attend. Screening uptake in 2012-2013 was lower than the results of our study, where we found that 91.7% of patients attended an eye check in the previous last year, suggesting that patients with diabetes on haemodialysis are aware of the need to undertake eye checks on a regular basis.
The United Kingdom National Diabetes Audit 2015-2016, found that 86.7% of patients with diabetes had foot surveillance that year[7], which was slightly higher than in our patient survey (83.3%). This is of some concern, particularly as patients with diabetes on haemodialysis are at high risk of foot problems. Recent guidelines recommend that patients have their feet screened every 3 mo with a locally agreed tool, and by staff on the dialysis unit[4].
In the United Kingdom, co-ordination of screening programmes for eyes and feet are led in the community by primary care health professionals. Retinal screening programmes are locally commissioned within Clinical Commissioning Group, and call and recall is organised by review of primary care records. Most retinal screening occurs via the retinal screening programme, although patients with established significant retinopathy may attend a medical retinal clinic as well. In the present study, it was found that the ophthalmology clinic was the most common place for eye checks, accounting for 67.5% of all patients. This is unsurprising as many patients on haemodialysis also have other microvascular complications such as retinopathy. A small proportion of patients had eye checks carried out by an optician, which, whilst useful, means that such patients may not be accessing a formal retinopathy screening programme. Interestingly, 7.1% of patients had an eye check carried out more than once in the past year, suggesting some duplication.
Foot checks for people with diabetes are generally performed by trained clinical staff in the primary care centre, which is often the practice nurse. Our study confirmed that nurses in the community were the most common group to carry out diabetic foot checks, with 67.1% of foot checks carried out by the nurses in primary care. Very few patients stated that their feet had ever been examined on the dialysis unit during dialysis. Patients on haemodialysis have logistical difficulties that make it difficult for them to attend appointments elsewhere. Perhaps this may account for patients missing screening appointments. A lack of co-ordination between the health care professionals caring for the patients may have also resulted in missed screening opportunities, as it is assumed that they have been carried out elsewhere. Patients spend significant amounts of time on dialysis, and this may provide an excellent opportunity for screening of feet and eyes to be undertaken opportunistically, as well as reducing the need for patients to attend hospital in between dialysis sessions. This is specifically mentioned as an important aim in recent United Kingdom guidelines, and clearly needs to be addressed in our haemodialysis unit[4]. These guidelines recommend that annual checks are documented, and made available to all those involved in the care of these patients.
The introduction of a robust system of documentation, would ensure that individuals involved are aware of recent checks and when they last took place, avoiding unnecessary duplication. Furthermore, access to a named link worker on the dialysis unit who would ensure that screening is carried out, which could ensure that patients have received eye and foot screening, and are also educated in looking for early signs of significant foot problems, and highlight these to health professionals at an early stage. Inter-professional learning between diabetes and renal specialists may facilitate improvements in care.
There are some limitations to this study, including a small patient cohort and the fact that it was carried out at a single tertiary centre. Patients with communication difficulties were excluded from the study, and it is possible that this group of patients may have had difficulty accessing healthcare, and may also be more likely to miss screening appointments. The study did not examine the barriers to patients attending screening appointments.
Patients with diabetes on dialysis are at risk of microvascular complications, and due to logistical issues have difficulties attending other appointments. Most patients had an eye check in the last year, with a lower percentage of recalling a foot check in the last year. It is hoped that the introduction of recent guidelines will improve the uptake of screening.
Patients with diabetes on haemodialysis are at high risk of diabetes complications including foot and eye problems. It is not known whether patients with diabetes on haemodialysis attend regular screening appointments for foot and eye checks. This survey aimed to determine this information.
It is increasingly recognised that prevention of diabetic complications in patients on haemodialysis is important. At the moment, it is unknown whether improving glucose control or other risk factors will reduce morbidity and mortality in such patients.
Recent United Kingdom guidelines suggest a more proactive approach to managing patients with diabetes on haemodialysis. It is hoped that with more structured care, better outcomes will be seen.
The authors show that most patients with diabetes on haemodialysis attend for eye checks, but that foot checks may be neglected. The authors propose that foot checks on dialysis would be an effective way to ensure proactive management of foot problems in patients on dialysis.
Mothojakan et al report the findings of a retrospective study of whether foot and eye screening is being done on diabetic patients undergoing hemodialysis. The paper has been revised in light of a previous review and is well written, easy to follow and without any obvious errors or unfounded claims.
Manuscript source: Invited manuscript
Specialty type: Endocrinology and metabolism
Country of origin: United Kingdom
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Ali O, Miller S, Qi L, Tamemoto H S- Editor: Song XX L- Editor: A E- Editor: Li D
| 1. | Caskey F, Cullen R. UK Renal Registry 18th Annual Report: Introduction. Nephron. 2016;132 Suppl 1:1-8. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 2. | National Institute for Health and Care Excellence. Diabetic foot problems: prevention and management. NICE guideline NG19. Available from: http://www.nice.org.uk/guidance/ng19; Accessed 04.05.17. [Cited in This Article: ] |
| 3. | Standards of Medical Care in Diabetes-2017: Summary of Revisions. Diabetes Care. 2017;40:S4-S5. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 280] [Cited by in F6Publishing: 356] [Article Influence: 50.9] [Reference Citation Analysis (0)] |
| 4. | Frankel A, Kazempour-Ardebili S, Bedi R, Chowdhury TA, De P, El-Sherbini N, Game F, Gray S, Hardy D, James J. Management of adults with diabetes on the haemodialysis unit: summary of new guidance from the Joint British Diabetes Societies and Renal Association. British J Diabetes. 2016;16:69-77. [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Ndip A, Rutter MK, Vileikyte L, Vardhan A, Asari A, Jameel M, Tahir HA, Lavery LA, Boulton AJ. Dialysis treatment is an independent risk factor for foot ulceration in patients with diabetes and stage 4 or 5 chronic kidney disease. Diabetes Care. 2010;33:1811-1816. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 112] [Cited by in F6Publishing: 100] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 6. | Morioka T, Emoto M, Tabata T, Shoji T, Tahara H, Kishimoto H, Ishimura E, Nishizawa Y. Glycemic control is a predictor of survival for diabetic patients on hemodialysis. Diabetes Care. 2001;24:909-913. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 172] [Cited by in F6Publishing: 180] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 7. | National Diabetes Audit 2015-6. 1. Care processes and treatment targets. Available from: http://www.content.digital.nhs.uk/catalogue/PUB23241/nati-diab-rep1-audi-2015-16.pdf Accessed 04.05.17. [Cited in This Article: ] |