Published online Mar 16, 2017. doi: 10.4253/wjge.v9.i3.127
Peer-review started: June 17, 2016
First decision: July 27, 2016
Revised: August 18, 2016
Accepted: January 2, 2017
Article in press: January 3, 2017
Published online: March 16, 2017
To examine the utility of endoscopic retrograde cholangiopancreatography (ERCP) on biliopancreatic diseases in the patients with Billroth II-reconstructed stomach.
For 26 cases of biliopancreatic diseases in patients with Billroth II-reconstructed stomach, ERCP was conducted using a straight-view scope or a retrograde oblique-viewing endoscope. All the cases were patients aiming at selective insertion into the bile duct. One patient aimed at diagnosis, and 25 patients aimed at treatment. The cases in which the endoscope reached the duodenal papilla and anastomosis, and insertion into the bile duct became possible, were considered successful.
The rate of reaching the duodenal papilla and anastomosis was 84.7% (22/26 patients). Among the cases without reaching the duodenal papilla and anastomosis, there were 2 in which the endoscope did not pass due to tumor-induced duodenal infiltration. In 1 case, the fiber did not reach the duodenal papilla due to long afferent loop. The success rate of insertion into the bile duct in patients in which the endoscope reached the duodenal papilla and anastomosis was 90.9% (20/22 patients), and the success rate of procedures including treatment was 86.3% (19/22 patients). After treatment, mild cholangitis was observed in 1 patient (4.5%, 1/22 patients) but relieved conservatively. No other accidental symptom was observed.
It was considered that the ERCP for biliopancreatic diseases in patients with Billroth II-reconstructed stomach will become a less invasive, safe and useful examination and treatment approach.
Core tip: It was considered that the endoscopic retrograde cholangiopancreatography for biliopancreatic diseases in patients with Billroth II-reconstructed stomach will become a less invasive, safe and useful examination and treatment approach.
- Citation: Sakai Y, Tsuyuguchi T, Mikata R, Sugiyama H, Yasui S, Miyazaki M, Yokosuka O. Utility of endoscopic retrograde cholangiopancreatography on biliopancreatic diseases in patients with Billroth II-reconstructed stomach. World J Gastrointest Endosc 2017; 9(3): 127-132
- URL: https://www.wjgnet.com/1948-5190/full/v9/i3/127.htm
- DOI: https://dx.doi.org/10.4253/wjge.v9.i3.127
With the development of endoscopic techniques, equipment and treatment tools in recent years, the endoscopic approach for biliopancreatic diseases is rapidly evolving, and less invasive treatment has become possible. Moreover, it can be said that the necessity for endoscopic retrograde cholangiopancreatography (ERCP)-related procedures is increasing because of improvement of the results of surgical operation and postoperative careful follow-up in patients after gastrectomy. In patients after gastrectomy, however, the difficulty in procedures is high because the methods of approach to the papilla and anastomosis are different according to the anatomy by reconstruction method and because the physical relationship of the papilla is different endoscopically. In the present study, we performed ERCP on cases of biliopancreatic disease in patients with Billroth II-reconstructed stomach to examine its utility and safety.
The subjects included 26 patients with Billroth II-reconstructed stomach, who have biliopancreatic diseases and have attempted the ERCP 42 times in total from April 1999 to February 2010. There were 21 male and 5 female patients, with the mean age of 70.2-year-old (ranging from 59-year-old to 89-year-old). The diseases were bile duct stone in 20 patients, intrahepatic stone in 1 patient, papilla vater cancer in 1 patient, gallbladder cancer in 1 patient, cholangiocarcinoma in 1 patient, pancreatic cancer in 1 patient and biliary obstruction due to peritoneal metastasis of gastric cancer in 1 patient. One patient underwent diagnostic ERCP, and 25 patients underwent therapeutic ERCP (Table 1).
| Sex | 21 males5 females | |
| Age | 70.2 yr (range: 59-89 yr) | |
| Disease | Bile duct stone | 20 |
| Intrahepatic stone | 1 | |
| Papilla vater cancer | 1 | |
| Gallbladder cancer | 1 | |
| Cholangiocarcinoma | 1 | |
| Pancreatic cancer | 1 | |
| Metastatic biliary obstruction | 1 | |
| Target region | Bile duct | 25 |
| Pancreatic duct | 1 | |
| Purpose | Diagnosis | 1 |
| Treatment | 25 |
Among the 42 total procedures, a straight-view scope and a retrograde oblique-viewing endoscope were used 24 and 18 times, respectively (Q200, 230, 240, XQ200, PCF240, JF230 and JF240: Olympus Corp, Tokyo, Japan). For cannulation, catheters PR-104Q, R110Q-1 and PR233Q were used. A 0.025-inch or 0.035-inch guidewire (Jagwire by Microvasive, Boston Scientific Corp, Natick, MA, United States or Revo Wave by Olympus Corp) was used. For endoscopic papillary balloon dilatation (EPBD), the balloon was selected according to the diameter of the bile duct and dilated at 4 atmospheres until the notch disappeared (OLBERT by Maeadox Surgimed Corp, or QUANTUM by Boston Scientific Corp). Endoscopic sphincterotomy (EST) was conducted using a single electrosurgical current generator (PSD-20; Olympus Corp) at a power of 25 W. For incision, the needle-knife (KD10Q-1; Olympus Corp) was used.
When the endoscope reached the duodenal papilla or anastomosis, when insertion into the bile duct or pancreatic duct became possible and when the purposes, including treatment, were achieved, the cases were considered successful. The endoscopic nasobiliary drainage tube (ENBD) of 7 Fr was used (Flexima; Boston Scientific Corp, or SD9 by SILUX). The tube stents of 7 Fr and 8.5 Fr were used (FLEXIMA, SOLOPASS: Boston Scientific Corp). As a metal stent, Flexxus (Kobayashi Medical) uncovered-type was used. Basket catheters (FG-22Q; Olympus Corp) were used for stone quarry, and LBGT-7245S (ZEON Medical) was used for lithotripsy. The rate of reaching the duodenal papilla or anastomosis, the success rate of insertion into bile duct in patients with achievement and the success rate of treatment were examined.
The endoscope and procedures were selected at the discretion of the operating surgeon. All the patients had provided written informed consent before these diagnostic and therapeutic procedures. Iatrogenic morbidity was assessed according to the criteria of Cotton et al[1].
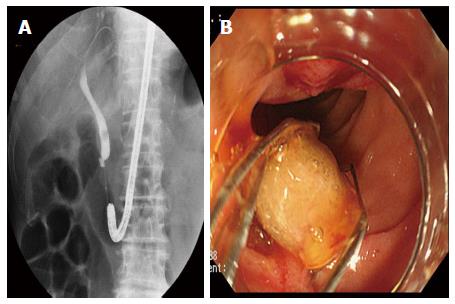
The rate of reaching the duodenal papilla or anastomosis was 84.7% (22/26 patients). The Braun anastomosis was observed at a rate of 38.5% (10/26 patients). Among the cases not reaching the papilla or anastomosis, there were 2 in which the endoscope did not pass due to tumor-induced duodenal infiltration. In 1 case, the fiber did not reach the duodenal papilla due to long afferent loop. The success rate of insertion into bile duct in the patients in which the endoscope reached the papilla or anastomosis was 90.9% (20/22 patients). As treatment of papilla, the EPBD and EST were conducted on 18 and 2 patients, respectively. The remaining 1 patient was a patient with intrahepatic stone, who underwent choledochojejunostomy, and since no stenosis of anastomosis was observed, the treatment was started with no procedure for the anastomosis. In the patients with bile duct stone (Figure 1), the mean diameter of stone was 8.6 mm (range of 0 mm to 16 mm), and the number of stones ranged from 0 to 1.5, with 2 patients having spontaneous elimination of stones and showing no stone in cholangiography. All these patients succeeded in collection of stones.
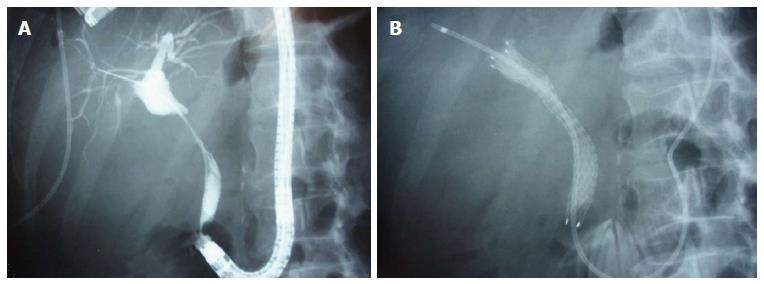
Among the 42 ERCP procedures conducted, drainage was performed 15 times, and the ENBD, placement of tube stent and placement of metallic stent were attempted 9 times, 5 times and 1 time, respectively (Figure 2), all of which were successful. The success rate of treatment was 86.3% (19/22 patients). The one patient who succeeded in cholangiography but failed in treatment was the one with intrahepatic stone who underwent choledochojejunostomy and who failed in lithotripsy because the guidewire passed through stones to the side of liver but the catheter did not pass. On that patient, percutaneous transhepatic cholangioscopic lithotripsy was performed after percutaneous transhepatic biliary drainage (PTBD), and the treatment was successful. In the present treatment, mild cholangitis was observed in 1 patient (4.5%, 1/22 patient) but was relieved conservatively. No other accidental symptom was observed. Among 4 patients in which the endoscope did not reach the duodenal papilla, 3 patients underwent PTBD. One patient had bile duct stone with no hepatic disorder, and surgery was conducted instead of PTBD. Among 2 patients in which the endoscope reached the papilla but the biliary cannulation was impossible, 1 patient underwent the PTBD and another patient was the one with gallbladder cancer showing no jaundice, and on this patient, the ERCP was conducted for the purpose of diagnosis, which was not successful, so the image of bile duct was substituted with magnetic resonance cholangiopancreatography (MRCP).
The patients with biliopancreatic diseases after gastrectomy have experienced open surgery once. In the non-gastrectomized patients, repeated open surgery for the diseases such as bile duct stone, in which the endoscopic treatment becomes the first option, puts a heavy strain on the patients. In recent years, both the rate of reaching the duodenal papilla and the success rate of the procedure have been reported to be relatively good from various institutions for the patients with Billroth II-reconstructed stomach[2-20]. Since the afferent loop is relatively short in the patients with Billroth II-reconstructed stomach, different from the Roux-en-Y-reconstructed stomach, reaching the papilla may frequently be possible even using a straight-view scope or a retrograde oblique-viewing endoscope.
In our present results, the rate of reaching the duodenal papilla and anastomosis was 87.5%, the success rate of cholangiography was 90.5%, and the procedural success rate was 85.7%. Among the patients in which the endoscope did not reach the duodenal papilla and anastomosis, the fiber did not pass due to tumor-induced infiltration in 2 patients. It is shown that, if there is no problem in the passage of fiber and if the fiber can reach the area, the procedure has a high probability of being successful. In the remaining 1 patient of our study, the fiber did not reach the duodenal papilla due to long afferent loop. When the fiber is too short to reach the papilla with a straight-view scope or a retrograde oblique-viewing endoscope, there is a possibility that this problem can be resolved by using a single balloon enteroscopy[18] or a double balloon[19,20] with a long effective length.
Concerning attainment to the duodenal papilla in the patients with the Billroth II-reconstructed stomach, moreover, it is said that the presence or absence of Braun anastomosis may have a large influence on the rate of reaching the papilla. The results in the patients with no Braun anastomosis are good, but those in the patients with Braun anastomosis are bad. Ciçek et al[11] reported that the rate of reaching the papilla was 29% in the patients with Braun anastomosis. In the patients with Braun anastomosis, when endoscopy is conducted indefinitely, it may induce repeated round trip of the same route and become a waste of time. It is integral to aim at attainment to the papilla having a clear strategy so as not to neglect to confirm the direction of movement at the anastomosis. Concerning the route into which the endoscope has ever entered, for example, it is considered necessary to mark with clips, etc.
As to the fiber, we used a straight-view scope or a retrograde oblique-viewing endoscope. With a straight-view scope, it is easy to secure the field of view of the lumen of the intestinal tract during insertion of the endoscope into the small intestine, which is superior to the retrograde oblique-viewing endoscope from the aspect of prevention of perforation. Since the usual straight view scope has a small inlet of forceps, however, the available devices have some limitations. With the retrograde oblique-viewing endoscope, on the other hand, it is difficult to obtain the field of view of the lumen of the gastrointestinal tract, and insertion of the endoscope into the small intestine is difficult. In the past, there have been a lot of reports of perforation of 0.7% to 18% with a retrograde oblique-viewing endoscope, compared with that of a straight-view endoscope[6-15]. In many cases, the blinded manipulation of endoscope may be associated with this. Since the retrograde oblique-viewing endoscope has a longer effective length than the straight-view endoscope and has a bending forceps device after reaching the papilla, however, it is effective for selective cannulation. In recent years, very good results have been obtained by an anterograde oblique-viewing endoscope having the same effective length and the same field of view as the straight-view scope and a bending forceps device[21,22]. At present, there is a problem of effective length, but in the case of Billroth II-reconstructed stomach, this fiber can become the first option.
In the patients with Billroth II-reconstructed stomach, however, this method may be difficult because the oppositely-oriented approach should be conducted different from the usual ERCP. In the patients for whom the fiber reached the papilla in this study, the success rate of cannulation was as high as 90.9%. This report does not have inferiority in comparison with the results of an anterograde oblique-viewing endoscope[21,22]. The reason why the success rate was high despite that this patient represented a case with difficulty in cannulation, in which the papilla existed on the opposite side from the usual one, was because the flexible tip catheter[23], etc., with which the angle can be changed in cannulation, was used. Since the success rate was not 100%, despite the high success rate, improved techniques of operators and further modification of treatment tools are required.
Concerning the treatment of papilla, the EST and EPBD have been performed. Different from the usual ERCP, it is difficult to perform EST with a needle knife because the oppositely-oriented approach should be performed. If we wish to perform EST because it is advantageous for subsequent treatment of giant bile duct stone, it should be used because there is a papillotome effective for the Billroth II-reconstructed stomach different from usual papillotome[5,10], if EST with a needle knife is technically difficult. Different from the EST, on the other hand, if a guidewire is placed in the bile duct, it may be possible to perform treatment easily with EPBD, even if using usual treatment tools. Therefore, choledocholithiasis in the patients with Billroth II-reconstructed stomach is considered a good indication for EPBD unless otherwise specified.
In the present study, however, we have not experienced cases with pancreatitis as an accidental symptom; but, since EPBD is a risk factor of post-ERCP pancreatitis[24,25], it is considered very important to perform prevention against pancreatitis due to placement of pancreatic stent[26,27] in the patients undergoing erroneous pancreatography or patients in whom a guidewire was erroneously inserted into the pancreatic duct. Considering that stones were spontaneously eliminated in 2 patients among the patients with bile duct stone in the present study, moreover, since attainment to the papilla and subsequent treatment are more difficult in the patients with Billroth II-reconstructed stomach than usual patients, it may be better to perform MRCP at first and then to follow-up the patients without conducting the ERCP, as much as possible, if no stone is identified[28-30]. The treatment with endoscope on biliopancreatic disease in the patients with Billroth II-reconstructed stomach is less invasive, which is considered the treatment to be tried at first. Since there are some patients who present difficulty in treatment with endoscope, however, we should consider percutaneous approaches and surgical treatment if the percutaneous method is difficult, without sticking to the endoscopic treatment exclusively.
In conclusion, it was considered that ERCP for biliopancreatic diseases in patients with Billroth II-reconstructed stomach will become a less invasive, safe and useful examination and treatment approach.
With the development of endoscopic techniques, equipment and treatment tools in recent years, the endoscopic approach for biliopancreatic diseases has been rapidly evolving and less invasive treatment has become possible. In the present study, the authors performed endoscopic retrograde cholangiopancreatography (ERCP) for biliopancreatic disease in patients with Billroth II-reconstructed stomach to examine its utility and safety.
The subjects were 26 patients with Billroth II-reconstructed stomach, who have biliopancreatic diseases and have attempted the ERCP a total of 42 times from April 1999 to February 2010.
The rate of reaching the duodenal papilla or anastomosis was 84.7% (22/26 patients). The success rate of treatment was 86.3% (19/22 patients). In the present treatment, mild cholangitis was observed in 1 patient (4.5%, 1/22 patient) but relieved conservatively.
Biliopancreatic disease in patients with Billroth II-reconstructed stomach.
It was considered that ERCP for biliopancreatic diseases in patients with Billroth II-reconstructed stomach will become a less invasive, safe and useful examination and treatment approach.
The authors conducted a retrospective study regarding the issue of ERCP in the treatment of biliopancreatic disease in patients with Billroth-II gastrectomy. This topic is interesting.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Japan
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Fogli L, Mentes O, Yan SL S- Editor: Gong XM L- Editor: A E- Editor: Wu HL
| 1. | Cotton PB, Lehman G, Vennes J, Geenen JE, Russell RC, Meyers WC, Liguory C, Nickl N. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991;37:383-393. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1890] [Cited by in F6Publishing: 1934] [Article Influence: 58.6] [Reference Citation Analysis (1)] |
| 2. | Safrany L. Endosocpy and retrograde cholangiopancreatography after Billroth II operation. Endoscopy. 1972;4:198-202. [DOI] [Cited in This Article: ] |
| 3. | Katon RM, Bilbao MK, Parent JA, Smith FW. Endoscopic retrograde cholangiopancreatography in patients with gastrectomy and gastrojejunostomy (Billroth II), A case for the forward look. Gastrointest Endosc. 1975;21:164-165. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 18] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Thon HJ, Löffler A, Buess G, Gheorghiu T. Is ERCP a reasonable diagnostic method for excluding pancreatic and hepatobiliary disease in patients with a Billroth II resection? Endoscopy. 1983;15:93-95. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 16] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Siegel JH, Yatto RP. ERCP and endoscopic papillotomy in patients with a Billroth II gastrectomy: report of a method. Gastrointest Endosc. 1983;29:116-118. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 14] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Costamagna G, Mutignani M, Perri V, Gabrielli A, Locicero P, Crucitti F. Diagnostic and therapeutic ERCP in patients with Billroth II gastrectomy. Acta Gastroenterol Belg. 1994;57:155-162. [PubMed] [Cited in This Article: ] |
| 7. | Kim MH, Lee SK, Lee MH, Myung SJ, Yoo BM, Seo DW, Min YI. Endoscopic retrograde cholangiopancreatography and needle-knife sphincterotomy in patients with Billroth II gastrectomy: a comparative study of the forward-viewing endoscope and the side-viewing duodenoscope. Endoscopy. 1997;29:82-85. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 85] [Cited by in F6Publishing: 93] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 8. | Osnes M, Rosseland AR, Aabakken L. Endoscopic retrograde cholangiography and endoscopic papillotomy in patients with a previous Billroth-II resection. Gut. 1986;27:1193-1198. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 82] [Cited by in F6Publishing: 84] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 9. | Nordback I, Airo I. Endoscopic retrograde cholangiopancreatography (ERCP) and sphincterotomy (EST) after BII resection. Ann Chir Gynaecol. 1988;77:64-69. [PubMed] [Cited in This Article: ] |
| 10. | Hintze RE, Veltzke W, Adler A, Abou-Rebyeh H. Endoscopic sphincterotomy using an S-shaped sphincterotome in patients with a Billroth II or Roux-en-Y gastrojejunostomy. Endoscopy. 1997;29:74-78. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 60] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 11. | Ciçek B, Parlak E, Dişibeyaz S, Koksal AS, Sahin B. Endoscopic retrograde cholangiopancreatography in patients with Billroth II gastroenterostomy. J Gastroenterol Hepatol. 2007;22:1210-1213. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 48] [Cited by in F6Publishing: 48] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 12. | Hintze RE, Adler A, Veltzke W, Abou-Rebyeh H. Endoscopic access to the papilla of Vater for endoscopic retrograde cholangiopancreatography in patients with billroth II or Roux-en-Y gastrojejunostomy. Endoscopy. 1997;29:69-73. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 145] [Cited by in F6Publishing: 158] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 13. | Faylona JM, Qadir A, Chan AC, Lau JY, Chung SC. Small-bowel perforations related to endoscopic retrograde cholangiopancreatography (ERCP) in patients with Billroth II gastrectomy. Endoscopy. 1999;31:546-549. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 105] [Cited by in F6Publishing: 118] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 14. | Elton E, Hanson BL, Qaseem T, Howell DA. Diagnostic and therapeutic ERCP using an enteroscope and a pediatric colonoscope in long-limb surgical bypass patients. Gastrointest Endosc. 1998;47:62-67. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 103] [Cited by in F6Publishing: 94] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 15. | Bergman JJ, van Berkel AM, Bruno MJ, Fockens P, Rauws EA, Tijssen JG, Tytgat GN, Huibregtse K. A randomized trial of endoscopic balloon dilation and endoscopic sphincterotomy for removal of bile duct stones in patients with a prior Billroth II gastrectomy. Gastrointest Endosc. 2001;53:19-26. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 117] [Cited by in F6Publishing: 121] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 16. | Lin LF, Siauw CP, Ho KS, Tung JC. ERCP in post-Billroth II gastrectomy patients: emphasis on technique. Am J Gastroenterol. 1999;94:144-148. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 68] [Cited by in F6Publishing: 74] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 17. | Park CH, Lee WS, Joo YE, Kim HS, Choi SK, Rew JS. Cap-assisted ERCP in patients with a Billroth II gastrectomy. Gastrointest Endosc. 2007;66:612-615. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47] [Cited by in F6Publishing: 52] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 18. | Itoi T, Ishii K, Sofuni A, Itokawa F, Tsuchiya T, Kurihara T, Tsuji S, Ikeuchi N, Umeda J, Moriyasu F. Single-balloon enteroscopy-assisted ERCP in patients with Billroth II gastrectomy or Roux-en-Y anastomosis (with video). Am J Gastroenterol. 2010;105:93-99. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 129] [Cited by in F6Publishing: 123] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 19. | Maaser C, Lenze F, Bokemeyer M, Ullerich H, Domagk D, Bruewer M, Luegering A, Domschke W, Kucharzik T. Double balloon enteroscopy: a useful tool for diagnostic and therapeutic procedures in the pancreaticobiliary system. Am J Gastroenterol. 2008;103:894-900. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 70] [Cited by in F6Publishing: 74] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 20. | Chu YC, Su SJ, Yang CC, Yeh YH, Chen CH, Yueh SK. ERCP plus papillotomy by use of double-balloon enteroscopy after Billroth II gastrectomy. Gastrointest Endosc. 2007;66:1234-1236. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 30] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 21. | Kikuyama M, Matsubayashi Y, Kageyama F, Sumiyoshi S, Kobayashi Y. Oblique-viewing endoscope facilitates endoscopic retrograde cholangiopancreatography and associated procedures in post Billroth II gastrectomy patients. Dig Endosc. 2005;17:9-12. [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 22. | Nakahara K, Horaguchi J, Fujita N, Noda Y, Kobayashi G, Ito K, Obana T, Takasawa O. Therapeutic endoscopic retrograde cholangiopancreatography using an anterior oblique-viewing endoscope for bile duct stones in patients with prior Billroth II gastrectomy. J Gastroenterol. 2009;44:212-217. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 23. | Igarashi Y, Tada T, Shimura J, Ukita T, Inoue H, Maetani I, Sakai Y. A new cannula with a flexible tip (Swing Tip) may improve the success rate of endoscopic retrograde cholangiopancreatography. Endoscopy. 2002;34:628-631. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 19] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 24. | Freeman ML, Nelson DB, Sherman S, Haber GB, Herman ME, Dorsher PJ, Moore JP, Fennerty MB, Ryan ME, Shaw MJ. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1996;335:909-918. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1716] [Cited by in F6Publishing: 1607] [Article Influence: 57.4] [Reference Citation Analysis (2)] |
| 25. | Freeman ML, Guda NM. Prevention of post-ERCP pancreatitis: a comprehensive review. Gastrointest Endosc. 2004;59:845-864. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 321] [Cited by in F6Publishing: 305] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 26. | Tsuchiya T, Itoi T, Sofuni A, Itokawa F, Kurihara T, Ishii K, Tsuji S, Kawai T, Moriyasu F. Temporary pancreatic stent to prevent post endoscopic retrograde cholangiopancreatography pancreatitis: a preliminary, single-center, randomized controlled trial. J Hepatobiliary Pancreat Surg. 2007;14:302-307. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 57] [Cited by in F6Publishing: 57] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 27. | Sofuni A, Maguchi H, Itoi T, Katanuma A, Hisai H, Niido T, Toyota M, Fujii T, Harada Y, Takada T. Prophylaxis of post-endoscopic retrograde cholangiopancreatography pancreatitis by an endoscopic pancreatic spontaneous dislodgement stent. Clin Gastroenterol Hepatol. 2007;5:1339-1346. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 115] [Cited by in F6Publishing: 126] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 28. | Sakai Y, Tsuyuguchi T, Tsuchiya S, Sugiyama H, Miyakawa K, Ebara M, Saisho H, Yokosuka O. Diagnostic value of MRCP and indications for ERCP. Hepatogastroenterology. 2007;54:2212-2215. [PubMed] [Cited in This Article: ] |
| 29. | Sakai Y, Tsuyuguchi T, Yukisawa S, Tsuchiya S, Sugiyama H, Miyakawa K, Ohara T, Ebara M, Miyazaki M, Yokosuka O. Diagnostic value of magnetic resonance cholangiopancreatography for clinically suspicious spontaneous passage of bile duct stones. J Gastroenterol Hepatol. 2008;23:736-740. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 19] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 30. | Sakai Y, Tsuyuguchi T, Ishihara T, Yukisawa S, Ohara T, Tsuboi M, Ooka Y, Kato K, Katsuura K, Kimura M. Is ERCP really necessary in case of suspected spontaneous passage of bile duct stones? World J Gastroenterol. 2009;15:3283-3287. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 6] [Cited by in F6Publishing: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |