Published online Oct 16, 2018. doi: 10.4253/wjge.v10.i10.274
Peer-review started: April 30, 2018
First decision: May 15, 2018
Revised: June 6, 2018
Accepted: June 28, 2018
Article in press: June 29, 2018
Published online: October 16, 2018
Caustic injury of the esophagus is a problematic condition challenging endoscopists worldwide. Although the caustic agents and motives are different among countries and age groups, endoscopy still plays an invaluable role in diagnosis and treatment. Endoscopy can determine the severity of caustic ingestion which is of great importance in choosing appropriate treatment. However, some aspects of endoscopy in diagnosis of caustic injury remain controversial. Whether or not all patients need endoscopy, when to perform endoscopy and how to assess the severity are just some examples of these controversies. Due to lack of randomized controlled trials, many findings and suggestions are inconclusive. Computerized tomography scan of the chest and abdomen gains popularity in assessing the severity of caustic injury and avoiding unnecessary surgery. If esophageal stricture eventually develops, endoscopic dilatation is a mainstay. Maneuvers such as steroid injection and esophageal stent may be used in a refractory stricture. Nevertheless, some patients have to undergo surgery in spite of vigorous attempts with esophageal dilatation. To date, caustic injury remains a difficult situation. This article reviews all aspects of caustic injury of the esophagus focusing on endoscopic role. Pre-endoscopic management, endoscopy and its technique in acute and late phase of caustic injury including the endoscopic management of refractory stricture, and the treatment outcomes following each endoscopic intervention are thoroughly discussed. Finally, the role of endoscopy in the long term follow-up of patients with esophageal caustic injury is addressed.
Core tip: This mini-review comprehensively covered evidence-based endoscopy for caustic injury of the esophagus including pre-endoscopic management, endoscopic role in the acute and late phase of caustic injury, endoscopic management of refractory stricture and its outcomes. Tips and tricks to perform diagnostic and therapeutic endoscopy in these patients are also discussed.
- Citation: Methasate A, Lohsiriwat V. Role of endoscopy in caustic injury of the esophagus. World J Gastrointest Endosc 2018; 10(10): 274-282
- URL: https://www.wjgnet.com/1948-5190/full/v10/i10/274.htm
- DOI: https://dx.doi.org/10.4253/wjge.v10.i10.274
Caustic injury of the upper gastrointestinal tract remains one of the most challenging conditions presented to both gastroenterologists and surgical endoscopists. Endoscopy plays a major role in diagnosing and assessing the severity of caustic injury as well as guiding an appropriate treatment. Recently, computerized tomography (CT) scan of the chest and abdomen is increasingly used as complementary tool in the evaluation of caustic injury. Despite of advances in emerging technologies and treatments, severe morbidities and even death following the ingestion of caustic agents are evident in clinical practices thus suggesting the complexity of this condition.
Esophageal necrosis with subsequent perforation requiring emergency surgery may develop in the acute phase of caustic injury. Meanwhile, esophageal stricture (often being a complex stricture) is a late sequela of caustic injury which can be difficult to treat. Understanding fundamental knowledge of this condition will ensure the endoscopist to pursue the best course for the patient.
Although optimal management in the caustic injury of the esophagus remains rather inconclusive due to the lack of large epidemiologic studies and randomized clinical trials in the field, this narrative review summarizes current evidence on the role of endoscopy in the diagnosis and treatment of caustic injury of the esophagus. For the literature review, we used standard search strategies involving two online databases (PubMed and Scopus) using key words of caustic injury, corrosive ingestion, esophagus, endoscopy, diagnosis, treatment, dilatation, and surgery.
Caustic injury of the esophagus is a world-wide phenomenon. It was reported that in 2016 there were 176828 cases of caustic injury in the Unites States-accounting for 9.28% of all poisoning cases. The majority occurred in children with accidental ingestion[1]. Alkali ingestion is often seen in western countries, while acid ingestion is more common in Asian countries[2]. In Thailand, caustic ingestion involved 19.5% of poisoning cases and its incidence has been increasing[3]. Morbidity following caustic ingestion was high with a mortality rate of 8%. About one-third of patients with caustic ingestion eventually required surgery[4].
Caustic injury occurs when substance with pH < 2 or pH > 12 is ingested. Due to the “liquefactive necrosis” of alkali substance, caustic injury from alkali can cause more damage to gastrointestinal tract than the “coagulative necrosis” of acid ingestion. Earlier report suggested that alkali usually destroyed the esophagus and acid mainly damaged the stomach[5]. However, later endoscopic study contradicted this notion by showing that among acid ingestion patients, esophageal injury was seen in 87.8% and gastric injury in 85.4% of the patients[6]. Recent evidence indicated that acid ingestion caused more injury to the stomach (31% vs 13%) while the incidence of esophageal injury was similar between acid and alkali ingestion[7]. Gastroesophageal reflux from impaired lower esophageal sphincter function[8] and loss of esophageal motility[9] are also results of a caustic damage to the esophagus. Meanwhile, caustic injury to the duodenum appeared to be infrequent and less severe owing to pyloric spasm.
Since a caustic injury to the esophagus usually starts within a few minutes after ingestion, any attempt to lavage or induce vomiting will cause the agent to reflux into the esophagus thus resulting in a further damage. A caustic injury to the esophagus can be divided into in 3 phases as following[10]: (1) Phase of acute necrosis and thrombosis occurs in 1-4 d after caustic ingestion; (2) phase of ulceration and granulation occurs in 3-12 d after caustic ingestion. During this period, mucosal sloughing, bacterial invasion and granulation formation are evident. The esophagus is in the most friable phase. Any manipulation such as endoscopic examination or dilatation should be done with great care; and (3) healing phase begins from 3 wk after injury. It usually takes 1-6 mo to complete wound healing. Attempt to perform surgery for stricture cases unamenable to dilatation should wait beyond this period.
Stabilization of the patient is an ultimate goal during acute injury. Signs for airway injury e.g., hoarseness, stridor and poor ventilation are diligently sought for and immediately treated (if any). An evaluation for laryngeal edema should be pursued by direct laryngoscopy. A careful history taking includes the substance ingested, the amount and time of ingestion, pre-hospital treatment and the cause of ingestion. In addition to airway management, other pre-endoscopic management includes volume resuscitation, nil per os (NPO), avoidance of emetics and neutralizing agents, no insertion of nasogastric tube, and administration of broad-spectrum intravenous antibiotics[11]. Chest and abdominal X-ray is often an initial investigation for evaluating an extension of injury. Psychiatry consultation should be done in case of suicidal attempt.
Since clinical signs such as drooling and oral burn are not accurate predictors for caustic injury to the esophagus[12,13], endoscopy is therefore considered as the most important investigation to diagnose of this injury. Early endoscopy is recommended because about 30% of patients with caustic ingestion will have no injury to the esophagus and can be discharged promptly. Endoscopy is usually done within 24-48 h after ingestion. However, many experts have recommended endoscopy as soon as possible[14,15] because delayed endoscopy was associated with prolonged hospital stay and increased hospital expense[16]. Although some reports confirm the safety of endoscopy performed up to 96 h after ingestion[17], initial endoscopy after 48 h of ingestion is not advised because the injured esophagus may enter the phase of ulceration and granulation - in which the esophagus becomes fragile and easily perforated[18]. Nevertheless, as long as the principles of gentle handling of the endoscopy are maintained, endoscopy after 48 h in selected cases might be possible.
In the past, endoscopists were not encouraged to pass the scope beyond circumferential burn due to the fear of esophageal perforation[19]. However, with advances in endoscopic examination and more skills in endoscopy, complete endoscopic evaluation beyond this point is possible with no complication[20]. Endoscopy is beneficial to confirm the followings: existence of injury, degree of injury, and area of injury - which could guide a treatment and predict a prognosis.
All adult patients (in which suicide attempt was the most common cause) should undergo endoscopy, but there is controversy regarding endoscopy in children (in which accidental ingestion was the most common cause)[21]. Most authors agreed that endoscopy should be done in children with signs of drooling, dysphagia, oral lesions, respiratory distress and intentional ingestion[22,23]. Beyond these scenarios, clinical observation may be appropriate.
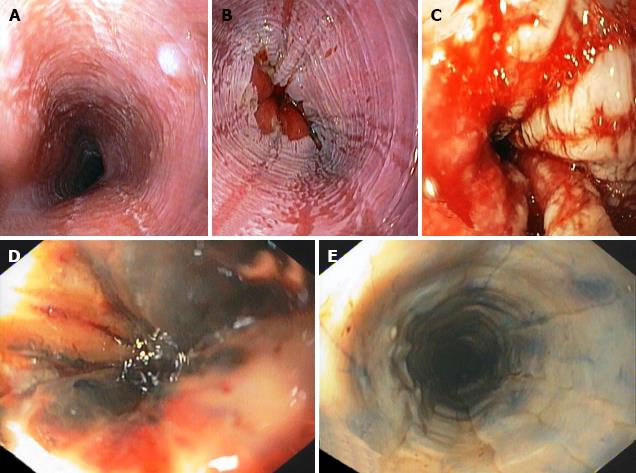
Endoscopy is contraindicated in patients with a suspicion of gastrointestinal perforation, necrosis of oral cavity and compromised airway. Gentle handling and avoidance of air over-insufflation is always recommended. The comparison of modified endoscopic findings classified by Zargar et al[17] (Figure 1) and CT grading by Ryu et al[24] are shown in Table 1.
| Grade | Endoscopic score[16] | score[21] |
| I | Edema and hyperemia of the mucosa | No definite swelling of esophagus wall (< 3 mm, within normal limit) |
| II | IIa: Friability, hemorrhages, erosion, blisters, whitish membranes, exudates and superficial ulcerations IIb: IIa with deep or circumferential ulceration | Edematous wall thickening (> 3 mm) without periesophageal soft tissue infiltration |
| III | IIIa: Small scattered areas of necrosis IIIb: Extensive necrosis | Edematous wall thickening with periesophageal soft tissue infiltration plus well-demarcated tissue interface |
| IV | Perforation | Edematous wall thickening with periesophageal soft tissue infiltration plus blurring of tissue interface or localized fluid collection around the esophagus or the descending aorta |
Classification and severity of caustic injury help predicting outcomes. Intentional ingestion, acid ingestion and high volume of ingestion were associated with a high grade of mucosal injury[4]. The patients with grade IIIb had longer hospital stay and higher rates of complication compared than those with grade IIIa[21]. However, a great variety of incidences in the degree of injury has been evident[4,7,11,12,18,21,25-28](Table 2). Discrepancy between inter-observers might reflect the difficulty to interpret the endoscopic findings especially when there was time lapsed before endoscopy. Treatment could be different according to the grading of severity as followings[11].
| Author | Year | Patients | Grade I | Grade II | Grade III |
| Alipour Faz et al[4] | 2017 | 313 | 42.5% | 16.9% | 20.1% |
| Ducoudray et al[7] | 2016 | n/a | n/a | n/a | 39.7% |
| Cabral et al[11] | 2012 | 315 | 12.7% | 22.9% | 29.2% |
| Chang et al[25] | 2011 | 389 | 14.7% | 39.3% | 42.4% |
| Cheng et al[21] | 2008 | 273 | n/a | n/a | 30% |
| Tohda et al[26] | 2008 | 95 | 49.4% | 26.3% | 13.7% |
| Havanond et al[12] | 2007 | 148 | 17% | 41% | 1% |
| Satar et al[27] | 2004 | 37 | 67.5% | n/a | 0% |
| Poley et al[18] | 2004 | 179 | 40% | 30% | 30% |
| Rigo et al[28] | 2002 | 210 | 32% | 13% | 6% |
Grade I (edema and erythema) or grade IIa (erosions and ulcers)
Since esophageal stricture will not occur in mild degree of injury, oral feeding can be resumed immediately and the patient can be discharged.
Grade IIb (circumferential ulceration)
Oral feeding can start once the patient can swallow saliva - often after 24-48 h after ingestion. Stricture will ensue in 30%-70% of these patients[29]. Therefore, barium swallowing is recommended at 3 wk after ingestion to detect the stricture and early dilatation will be performed accordingly.
Grade IIIa (scattered areas of necrosis)
Risk of perforation cannot be neglected in these patients and esophageal stricture may occur more than 90%.
Grade IIIb (extensive necrosis)
Emergency surgery is recommended. However, some physicians might use CT scan to confirm true necrosis of the esophagus because endoscopists may be unable to distinguish between superficial necrosis and transmural necrosis.
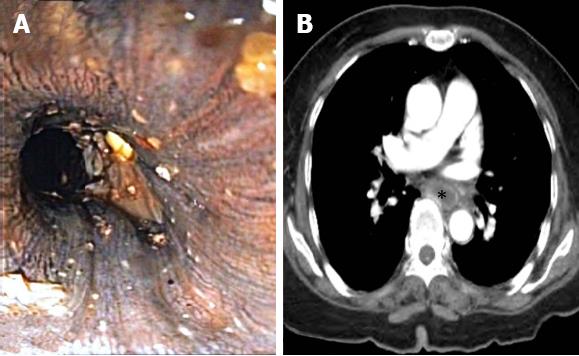
It is evident that endoscopy is not always accurate in determining the extent of caustic injury (Figure 2). Depending on the endoscopic findings alone, grade III injury would be over-estimated and unnecessary surgery was done in 15% of these patients[30]. Some authors showed that the accuracy in the diagnosis of grade II and III injury was 48% and 87%, respectively[31]. Recently, CT grading scores was developed in 2010 (Table 1) and shown to have a higher sensitivity and specificity than endoscopic score[24]. CT findings of transmural necrosis include esophageal wall blurring, peri-esophageal fat stranding and no enhancement of esophageal wall after intravenous contrast administrated. Recent studies showed that CT could prevent unnecessary esophagectomy in some patients with grade IIIb endoscopic score[32]. Although CT scan might underestimate the severity of caustic injury compared to endoscopy, it could provide further information about the involvement of adjacent organs e.g., lung and pleural cavity[33]. Nevertheless, CT scan cannot replace endoscopy in the evaluation of caustic injury especial in those with mucosal damage[34]. The combination of endoscopy and CT scan has been utilized in clinical setting - in which surgery could only be performed in case with grade IIIb endoscopy and CT score[35]. At present, combined use of endoscopy and CT scan, especially in case with grade IIIb endoscopic score, should help in the decision whether or not to operate.
Endoscopic ultrasonography (EUS) has some advantages over endoscopy and CT scan because it can delineate the layers of esophageal wall. If caustic injury is confined to submucosa in the EUS, the injured esophagus required a fewer sessions of esophageal dilatation than those with muscularis propria involvement[36]. Miniprobe EUS has been shown to predict stricture formation following caustic injury by visualizing the structure of esophageal wall[37]. However, the routine of EUS in clinical practice needs to be determined.
Endoscopy plays an important role in the treatment of caustic-related esophageal stricture. Caustic stricture is often complex and difficult to dilate[38]. Patients at risks for stricture were those with high endoscopic grade, ingestion of strong acid or alkali, leukocytosis and low thrombin ratio[39]. As acute inflammatory response to caustic agents lasts about 2 wk, early esophageal dilatation is usually done at 3 wk after caustic ingestion. After 8 wk, scar tissue is completely formed and the result of endoscopic dilatation is poor. Since good nutritional status is strongly related to a successful dilatation of esophageal stricture[40], early feeding via jejunostomy should start as soon as patients are clinically stable - especially in those with a significant damage in the esophagus and the stomach.
Practically, barium swallowing is done at 2-3 wk after caustic ingestion. Barium swallowing will provide crucial and relevant information on the stricture - which could determine the safety and success of endoscopic dilatation. This information includes:
(1) location and length of the stricture; (2) morphology of the stricture: tortuosity, angulation; (3) nature of the stricture: simple or complex; (4) complications of the stricture: concealed perforation, diverticulum; and (5) configuration of the stomach: any accompanying gastric stricture.
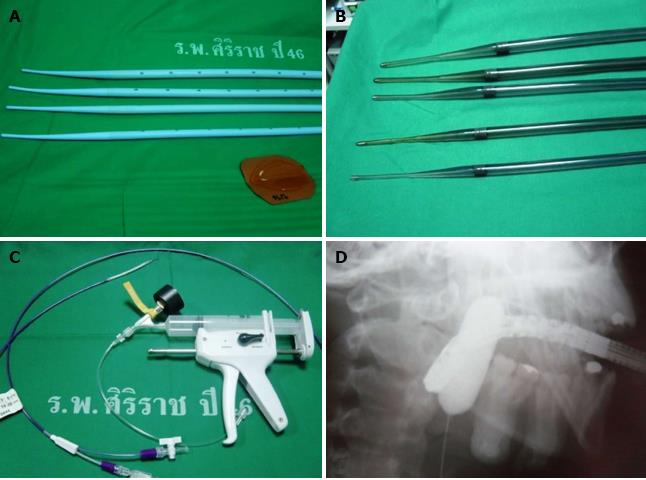
Esophageal dilatation can be done using various types of dilators. It can be performed under the combination endoscopy and fluoroscopy or endoscopy alone[41]. Commonly used esophageal dilatators are followings(Figure 3).
This dilator is easy to use but has no channel to insert guide-wire. It is suitable for short and straight stricture.
This dilator passes through the stricture via guide-wire under fluoroscopy. It is appropriate for tortuous, angulated and long stricture. Sensation of resistance during dilatation can be noted on this dilator thus resulting in protecting against over-dilatation.
This instrument can be used through-the-scope. It can reach area where Savary dilator cannot access. However, there is no sensation of resistance if over-dilatation occurs.
CRE balloon dilators achieve its dilatation effect by radial force while Savary and Maloney dilators exert its action via both radial and longitudinal forces. Although the mechanisms are different, all dilators seem to have comparable success rate and rate of perforation of 0.1%-0.4%[42]. Concerning the safety of an instrument, balloon dilator is preferred over Bougie dilator in children[43]. Techniques of esophageal dilatation are noted in Table 3.
| Early dilate (usually starting from 3 wk after caustic ingestion) |
| Use appropriate type and size of dilator |
| Maintain a dilator in lumen of the esophagus while dilating |
| Concern the rule of 3: Never dilate more than 3 dilators of progressively increasing diameter after considerable resistance is encountered |
| Weekly or bi-weekly dilate to obtain luminal competency at 40 Fr |
| Dilate per scheduled, not on demand |
| If chest pain occurs after dilatation, esophageal perforation must be rule out using contrast esophagography |
In order to prevent the over-dilatation of esophageal stricture, the rule of 3 is recommended as “never dilate more than 3 dilators of progressively increasing diameter after considerable resistance is encountered”[44]. Although some retrospective study showed that non-adherence to this rule did not increase the risk of esophageal perforation[45], we believe that the rule remains useful as a landmark during dilatation and a preventive measure of over-dilatation. Success rate of esophageal dilatation varied from 25% to 95% depending on the severity of caustic stricture[46-48].
Caustic stricture that could not be dilated to 14 mm over 5 sessions done with bi-week interval is defined as refractory stricture[49]. For refractory stricture, various modalities are advocated including electrocision, intralesional steroid injection, mitomycin-C injection, and esophageal stent.
Electrocautery could be applied to caustic stricture as it has been used in the treatment of Schatzki’s ring and anastomotic stricture with good results[50]. Multiple longitudinal incisions are made with needle knife through working channel of the endoscopy until the rim of the stenosis disappears. This maneuver proves to be a useful adjunct in esophageal dilatation.
In this method, prior to bougie dilatation, triamcinolone acetonide (40 mg/mL) 1 mL is diluted to 2 mL and injected at the stricture site in 4 quadrants. Combination of steroid injection and bougie dilatation could achieve more dilatation, improve dysphagia and reduce dilatation sessions[51].
Injection of mitomycin-C into the stricture site was shown to improve dysphagia score and easy passage of dilators[52-54] because mitomycin-C inhibited fibroblast proliferation and scar formation without interfering wound healing[55]. A randomized controlled trial showed a reduction in dilatation sessions if applying mitomycin-C during dilatation[56]. Mitomycin-C is beneficial in difficult or complex caustic stricture and can be combined with other modalities such as electrocision and esophageal stent[57].
Caustic stricture resistant to dilatation can be treated with esophageal stent insertion. Self-expandable plastic stent (SEPS) or fully-covered self-expandable metallic stent (FCSEMS) and recently, biodegradable stent are available. Practically, SEPS and FCSEMS are kept in place for 6 wk and should be removed before 12 wk. All types of esophageal stent have comparable efficacy but biodegradable stent has an advantage in non-requirement of stent removal. The clinical success of stent application in caustic stricture (i.e., free of dysphagia) was 33% with a migration rate of 40%[58,59]. Since its clinical success is about one-third and not last-longing, esophageal stent is considered as a last resource in the treatment of caustic injury.
Esophageal dilatation for caustic-induced stricture injury has lower success rate than esophageal stricture related to other etiologies[60]. Esophageal replacement is considered in patients who fail endoscopic therapy. Up to 50%-70% of patients with caustic stricture required surgery[46,61]. Stomach is used as a conduit if possible because it has less morbidity and mortality than colonic interposition[62]. If colonic interposition is required, transverso-splenic to ileocolic segment with blood supply via left colic artery provided excellent function in 75% of the patients[63]. In general, surgery should wait 6 mo after caustic ingestion for stabilizing patient, improving nutritional status, and allowing enough time to full attempt of endoscopic therapy.
Since caustic injury of the esophagus has been associated with 1000-fold increased risk of esophageal carcinoma[61], patients with high-graded caustic injury (especially that with esophageal stricture) should undergo endoscopic surveillance. The incidence of caustic-associated esophageal cancer ranges from 0%-30% and bypass surgery seems to have no influence on cancer development[64]. The time interval between caustic injury and malignant transformation of the esophagus was reported to be several decades[65]. As a result, endoscopic surveillance of the injured esophagus should start at about 15-20 years after an injury and it should be done every 2 or 3 years[66].
Endoscopy plays a crucial role in the diagnosis, assessment of severity, treatment and surveillance in patients with caustic injury of the esophagus. Meanwhile, CT scan of chest and abdomen has been increasingly used to improve accuracy in the diagnosis and severity assessment in difficult cases of esophageal caustic injury. Choice of endoscopic management and surveillance are considered mainly based on the grading of mucosal severity. Patients with high-graded mucosal injury are associated with increased risk of caustic-induced esophageal stricture which could be difficult to dilate due to its complex anatomy and extensive fibrosis. Better techniques or instruments for endoscopic dilation need to be developed to overcome this problem. Since caustic injury significantly increased risk of esophageal carcinoma, scheduled endoscopic surveillance every 2 or 3 years should perform at 15-20 years after an injury-especially in individuals with high-graded mucosal injury or those with esophageal stricture. Due to the complex nature of disease, caustic injury of the esophagus remains one of the most challenging clinical conditions presented to endoscopists.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Thailand
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Durand L, Ntanasis-Stathopoulos I S- Editor: Cui LJ L- Editor: A E- Editor: Wu YXJ
| 1. | Gummin DD, Mowry JB, Spyker DA, Brooks DE, Fraser MO, Banner W. 2016 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 34th Annual Report. Clin Toxicol (Phila). 2017;55:1072-1252. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 296] [Cited by in F6Publishing: 279] [Article Influence: 39.9] [Reference Citation Analysis (1)] |
| 2. | Rafeey M, Ghojazadeh M, Mehdizadeh A, Hazrati H, Vahedi L. Intercontinental comparison of caustic ingestion in children. Korean J Pediatr. 2015;58:491-500. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 3. | Saoraya J, Inboriboon PC. Acute Poisoning Surveillance in Thailand: The Current State of Affairs and a Vision for the Future. ISRN Emergency Medicine. 2013;2013:1-9. [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Alipour Faz A, Arsan F, Peyvandi H, Oroei M, Shafagh O, Peyvandi M, Yousefi M. Epidemiologic Features and Outcomes of Caustic Ingestions; a 10-Year Cross-Sectional Study. Emerg (Tehran). 2017;5:e56. [PubMed] [Cited in This Article: ] |
| 5. | Nicosia JF, Thornton JP, Folk FA, Saletta JD. Surgical management of corrosive gastric injuries. Ann Surg. 1974;180:139-143. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 33] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Zargar SA, Kochhar R, Nagi B, Mehta S, Mehta SK. Ingestion of corrosive acids. Spectrum of injury to upper gastrointestinal tract and natural history. Gastroenterology. 1989;97:702-707. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 147] [Cited by in F6Publishing: 109] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 7. | Ducoudray R, Mariani A, Corte H, Kraemer A, Munoz-Bongrand N, Sarfati E, Cattan P, Chirica M. The Damage Pattern to the Gastrointestinal Tract Depends on the Nature of the Ingested Caustic Agent. World J Surg. 2016;40:1638-1644. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Mutaf O, Genç A, Herek O, Demircan M, Ozcan C, Arikan A. Gastroesophageal reflux: a determinant in the outcome of caustic esophageal burns. J Pediatr Surg. 1996;31:1494-1495. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 56] [Cited by in F6Publishing: 58] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 9. | Genç A, Mutaf O. Esophageal motility changes in acute and late periods of caustic esophageal burns and their relation to prognosis in children. J Pediatric Surgery. 2002;37:1526-1528. [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 41] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 10. | Dafoe CS, Ross CA. Acute corrosive oesophagitis. Thorax. 1969;24:291-294. [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 18] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Cabral C, Chirica M, de Chaisemartin C, Gornet JM, Munoz-Bongrand N, Halimi B, Cattan P, Sarfati E. Caustic injuries of the upper digestive tract: a population observational study. Surg Endosc. 2012;26:214-221. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 42] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 12. | Havanond C, Havanond P. Initial signs and symptoms as prognostic indicators of severe gastrointestinal tract injury due to corrosive ingestion. J Emerg Med. 2007;33:349-353. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 37] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 13. | Boskovic A, Stankovic I. Predictability of gastroesophageal caustic injury from clinical findings: is endoscopy mandatory in children? Eur J Gastroenterol Hepatol. 2014;26:499-503. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 20] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 14. | Weigert A, Black A. Caustic ingestion in children. Continuing Education in Anaesthesia Critical Care and Pain. 2005;5:5-8. [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 21] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 15. | Kluger Y, Ishay OB, Sartelli M, Katz A, Ansaloni L, Gomez CA, Biffl W, Catena F, Fraga GP, Di Saverio S. Caustic ingestion management: world society of emergency surgery preliminary survey of expert opinion. World J Emerg Surg. 2015;10:48. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 38] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 16. | Abbas A, Brar TS, Zori A, Estores DS. Role of early endoscopic evaluation in decreasing morbidity, mortality, and cost after caustic ingestion: a retrospective nationwide database analysis. Dis Esophagus. 2017;30:1-11. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 17] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 17. | Zargar SA, Kochhar R, Mehta S, Mehta SK. The role of fiberoptic endoscopy in the management of corrosive ingestion and modified endoscopic classification of burns. Gastrointest Endosc. 1991;37:165-169. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 325] [Cited by in F6Publishing: 251] [Article Influence: 7.6] [Reference Citation Analysis (2)] |
| 18. | Poley JW, Steyerberg EW, Kuipers EJ, Dees J, Hartmans R, Tilanus HW, Siersema PD. Ingestion of acid and alkaline agents: outcome and prognostic value of early upper endoscopy. Gastrointest Endosc. 2004;60:372-377. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 139] [Cited by in F6Publishing: 150] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 19. | Thompson JN. Corrosive esophageal injuries. I. A study of nine cases of concurrent accidental caustic ingestion. Laryngoscope. 1987;97:1060-1068. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 17] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 20. | Temiz A, Oguzkurt P, Ezer SS, Ince E, Hicsonmez A. Predictability of outcome of caustic ingestion by esophagogastroduodenoscopy in children. World J Gastroenterol. 2012;18:1098-1103. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 45] [Cited by in F6Publishing: 41] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 21. | Cheng HT, Cheng CL, Lin CH, Tang JH, Chu YY, Liu NJ, Chen PC. Caustic ingestion in adults: the role of endoscopic classification in predicting outcome. BMC Gastroenterol. 2008;8:31. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 110] [Cited by in F6Publishing: 107] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 22. | Millar AJ, Cox SG. Caustic injury of the oesophagus. Pediatr Surg Int. 2015;31:111-121. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 32] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 23. | Bosnali O, Moralioglu S, Celayir A, Pektas OZ. Is rigid endoscopy necessary with childhood corrosive ingestion? a retrospective comparative analysis of 458 cases. Dis Esophagus. 2017;30:1-7. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 24. | Ryu HH, Jeung KW, Lee BK, Uhm JH, Park YH, Shin MH, Kim HL, Heo T, Min YI. Caustic injury: can CT grading system enable prediction of esophageal stricture? Clin Toxicol (Phila). 2010;48:137-142. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 56] [Cited by in F6Publishing: 41] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 25. | Chang JM, Liu NJ, Pai BC, Liu YH, Tsai MH, Lee CS, Chu YY, Lin CC, Chiu CT, Cheng HT. The role of age in predicting the outcome of caustic ingestion in adults: a retrospective analysis. BMC Gastroenterol. 2011;11:72. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 32] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 26. | Tohda G, Sugawa C, Gayer C, Chino A, McGuire TW, Lucas CE. Clinical evaluation and management of caustic injury in the upper gastrointestinal tract in 95 adult patients in an urban medical center. Surg Endosc. 2008;22:1119-1125. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 40] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 27. | Satar S, Topal M, Kozaci N. Ingestion of caustic substances by adults. Am J Ther. 2004;11:258-261. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 33] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 28. | Rigo GP, Camellini L, Azzolini F, Guazzetti S, Bedogni G, Merighi A, Bellis L, Scarcelli A, Manenti F. What is the utility of selected clinical and endoscopic parameters in predicting the risk of death after caustic ingestion? Endoscopy. 2002;34:304-310. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 44] [Cited by in F6Publishing: 40] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 29. | Katz A, Kluger Y. Caustic Material Ingestion Injuries- Paradigm Shift in Diagnosis and Treatment. Health Care: Current Reviews. 2015;3. [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 30. | Chirica M, Resche-Rigon M, Bongrand NM, Zohar S, Halimi B, Gornet JM, Sarfati E, Cattan P. Surgery for caustic injuries of the upper gastrointestinal tract. Ann Surg. 2012;256:994-1001. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 52] [Cited by in F6Publishing: 50] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 31. | Alipour-Faz A, Yousefi M, Peyvandi H. Accuracy of Endoscopy in Predicting the Depth of Mucosal Injury Following Caustic Ingestion; a Cross-Sectional Study. Emerg (Tehran). 2017;5:e72. [PubMed] [Cited in This Article: ] |
| 32. | Chirica M, Resche-Rigon M, Pariente B, Fieux F, Sabatier F, Loiseaux F, Munoz-Bongrand N, Gornet JM, Brette MD, Sarfati E. Computed tomography evaluation of high-grade esophageal necrosis after corrosive ingestion to avoid unnecessary esophagectomy. Surg Endosc. 2015;29:1452-1461. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 40] [Cited by in F6Publishing: 38] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 33. | Lurie Y, Slotky M, Fischer D, Shreter R, Bentur Y. The role of chest and abdominal computed tomography in assessing the severity of acute corrosive ingestion. Clin Toxicol (Phila). 2013;51:834-837. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 34. | Bonnici KS, Wood DM, Dargan PI. Should computerised tomography replace endoscopy in the evaluation of symptomatic ingestion of corrosive substances? Clin Toxicol (Phila). 2014;52:911-925. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 35. | Chirica M, Bonavina L, Kelly MD, Sarfati E, Cattan P. Caustic ingestion. Lancet. 2017;389:2041-2052. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 90] [Cited by in F6Publishing: 76] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 36. | Rana SS, Bhasin DK, Singh K. Role of endoscopic ultrasonography (EUS) in management of benign esophageal strictures. Ann Gastroenterol. 2011;24:280-284. [PubMed] [Cited in This Article: ] |
| 37. | Kamijo Y, Kondo I, Kokuto M, Kataoka Y, Soma K. Miniprobe ultrasonography for determining prognosis in corrosive esophagitis. Am J Gastroenterol. 2004;99:851-854. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 31] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 38. | Rodrigues-Pinto E, Pereira P, Ribeiro A, Lopes S, Moutinho-Ribeiro P, Silva M, Peixoto A, Gaspar R, Macedo G. Risk factors associated with refractoriness to esophageal dilatation for benign dysphagia. Eur J Gastroenterol Hepatol. 2016;28:684-688. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 39. | Le Naoures P, Hamy A, Lerolle N, Métivier E, Lermite E, Venara A. Risk factors for symptomatic esophageal stricture after caustic ingestion-a retrospective cohort study. Dis Esophagus. 2017;30:1-6. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 40. | Contini S, Swarray-Deen A, Scarpignato C. Oesophageal corrosive injuries in children: a forgotten social and health challenge in developing countries. Bull World Health Organ. 2009;87:950-954. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 60] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 41. | Jaiswal D, Krishna MV, Krishna M, Siddeshi ER. Safety and outcome using endoscopic dilation for benign esophageal stricture without fluoroscopy. J Digestive Endoscopy. 2015;6:55. [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 42. | Scolapio JS, Pasha TM, Gostout CJ, Mahoney DW, Zinsmeister AR, Ott BJ, Lindor KD. A randomized prospective study comparing rigid to balloon dilators for benign esophageal strictures and rings. Gastrointest Endosc. 1999;50:13-17. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 153] [Cited by in F6Publishing: 112] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 43. | Vandenplas Y. Management of Benign Esophageal Strictures in Children. Pediatr Gastroenterol Hepatol Nutr. 2017;20:211-215. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 17] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 44. | Riley SA, Attwood SE. Guidelines on the use of oesophageal dilatation in clinical practice. Gut. 2004;53 Suppl 1:i1-i6. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 68] [Cited by in F6Publishing: 57] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 45. | Rodrigues-Pinto E, Pereira P, Macedo G. Benign esophageal strictures: rule of 3 in esophageal dilation does not need to be a rule. Gastrointestinal Endoscopy. 2017;85:869-870. [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 46. | Tharavej C, Pungpapong SU, Chanswangphuvana P. Outcome of dilatation and predictors of failed dilatation in patients with acid-induced corrosive esophageal strictures. Surg Endosc. 2018;32:900-907. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 47. | Youn BJ, Kim WS, Cheon JE, Kim WY, Shin SM, Kim IO, Yeon KM. Balloon dilatation for corrosive esophageal strictures in children: radiologic and clinical outcomes. Korean J Radiol. 2010;11:203-210. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 30] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 48. | Singhal S, Kar P. Management of acid- and alkali-induced esophageal strictures in 79 adults by endoscopic dilation: 8-years’ experience in New Delhi. Dysphagia. 2007;22:130-134. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 49. | Kochman ML, McClave SA, Boyce HW. The refractory and the recurrent esophageal stricture: a definition. Gastrointest Endosc. 2005;62:474-475. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 182] [Cited by in F6Publishing: 172] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 50. | Hordijk ML, Siersema PD, Tilanus HW, Kuipers EJ. Electrocautery therapy for refractory anastomotic strictures of the esophagus. Gastrointest Endosc. 2006;63:157-163. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 93] [Cited by in F6Publishing: 84] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 51. | Nijhawan S, Udawat HP, Nagar P. Aggressive bougie dilatation and intralesional steroids is effective in refractory benign esophageal strictures secondary to corrosive ingestion. Dis Esophagus. 2016;29:1027-1031. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 27] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 52. | Nagaich N, Nijhawan S, Katiyar P, Sharma R, Rathore M. Mitomycin-C: ‘a ray of hope’ in refractory corrosive esophageal strictures. Dis Esophagus. 2014;27:203-205. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 53. | Divarci E, Kilic O, Dokumcu Z, Ozcan C, Erdener A. Topical Mitomycin C Application Is Effective Even in Esophageal Strictures Resistant to Dilatation Therapy in Children. Surg Laparosc Endosc Percutan Tech. 2017;27:e96-e100. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 54. | Uhlen S, Fayoux P, Vachin F, Guimber D, Gottrand F, Turck D, Michaud L. Mitomycin C: an alternative conservative treatment for refractory esophageal stricture in children? Endoscopy. 2006;38:404-407. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 76] [Cited by in F6Publishing: 80] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 55. | Türkyilmaz Z, Sönmez K, Demirtola A, Karabulut R, Poyraz A, Gülen S, Dinçer S, Başaklar AC, Kale N. Mitomycin C prevents strictures in caustic esophageal burns in rats. J Surg Res. 2005;123:182-187. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 42] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 56. | El-Asmar KM, Hassan MA, Abdelkader HM, Hamza AF. Topical mitomycin C application is effective in management of localized caustic esophageal stricture: A double-blinded, randomized, placebo-controlled trial. J Pediatric Surgery. 2013;48:1621-1627. [DOI] [Cited in This Article: ] [Cited by in Crossref: 54] [Cited by in F6Publishing: 55] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 57. | Bartel MJ, Seeger K, Jeffers K, Clayton D, Wallace MB, Raimondo M, Woodward TA. Topical Mitomycin C application in the treatment of refractory benign esophageal strictures in adults and comprehensive literature review. Dig Liver Dis. 2016;48:1058-1065. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 58. | Suzuki T, Siddiqui A, Taylor LJ, Cox K, Hasan RA, Laique SN, Mathew A, Wrobel P, Adler DG. Clinical Outcomes, Efficacy, and Adverse Events in Patients Undergoing Esophageal Stent Placement for Benign Indications: A Large Multicenter Study. J Clin Gastroenterol. 2016;50:373-378. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 37] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 59. | Repici A, Small AJ, Mendelson A, Jovani M, Correale L, Hassan C, Ridola L, Anderloni A, Ferrara EC, Kochman ML. Natural history and management of refractory benign esophageal strictures. Gastrointest Endosc. 2016;84:222-228. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 52] [Cited by in F6Publishing: 59] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 60. | Siersema PD, de Wijkerslooth LR. Dilation of refractory benign esophageal strictures. Gastrointest Endosc. 2009;70:1000-1012. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 110] [Cited by in F6Publishing: 91] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 61. | Contini S, Scarpignato C. Caustic injury of the upper gastrointestinal tract: a comprehensive review. World J Gastroenterol. 2013;19:3918-3930. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 231] [Cited by in F6Publishing: 183] [Article Influence: 16.6] [Reference Citation Analysis (6)] |
| 62. | Harlak A, Yigit T, Coskun K, Ozer T, Mentes O, Gülec B, Kozak O. Surgical treatment of caustic esophageal strictures in adults. Int J Surg. 2013;11:164-168. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 63. | Knezević JD, Radovanović NS, Simić AP, Kotarac MM, Skrobić OM, Konstantinović VD, Pesko PM. Colon interposition in the treatment of esophageal caustic strictures: 40 years of experience. Dis Esophagus. 2007;20:530-534. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 69] [Cited by in F6Publishing: 73] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 64. | Kay M, Wyllie R. Caustic ingestions in children. Curr Opin Pediatr. 2009;21:651-654. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 102] [Cited by in F6Publishing: 106] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 65. | Ntanasis-Stathopoulos I, Triantafyllou S, Xiromeritou V, Bliouras N, Loizou C, Theodorou D. Esophageal remnant cancer 35 years after acidic caustic injury: A case report. Int J Surg Case Rep. 2016;25:215-217. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 66. | ASGE Standards of Practice Committee, Evans JA, Early DS, Fukami N, Ben-Menachem T, Chandrasekhara V, Chathadi KV, Decker GA, Fanelli RD, Fisher DA, Foley KQ, Hwang JH, Jain R, Jue TL, Khan KM, Lightdale J, Malpas PM, Maple JT, Pasha SF, Saltzman JR, Sharaf RN, Shergill A, Dominitz JA, Cash BD; Standards of Practice Committee of the American Society for Gastrointestinal Endoscopy. The role of endoscopy in Barrett’s esophagus and other premalignant conditions of the esophagus. Gastrointest Endosc. 2012;76:1087-1094. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 262] [Cited by in F6Publishing: 234] [Article Influence: 19.5] [Reference Citation Analysis (1)] |