Published online Sep 28, 2017. doi: 10.3748/wjg.v23.i36.6733
Peer-review started: July 18, 2017
First decision: August 10, 2017
Revised: August 17, 2017
Accepted: August 25, 2017
Article in press: August 25, 2017
Published online: September 28, 2017
To prospectively evaluate the effect of local wound infiltration with ropivacaine on postoperative pain relief and stress response reduction after open hepatectomy.
A total of 56 patients undergoing open hepatectomy were randomly divided into two groups: a ropivacaine group (wound infiltration with ropivacaine solution) and a control group (infiltration with isotonic saline solution). A visual analog scale (VAS) at rest and on movement was used to measure postoperative pain for the first 48 h after surgery. Mean arterial pressure (MAP), heart rate (HR), time to bowel recovery, length of hospitalization after surgery, cumulative sufentanil consumption, and incidence of nausea and vomiting were compared between the two groups. Surgical stress hormones (epinephrine, norepinephrine, and cortisol) were detected using enzyme-linked immunosorbent assay, and the results were compared.
VAS scores both at rest and on movement at 24 h and 48 h were similar between the two groups. Significantly lower VAS scores were detected at 0, 6, and 12 h in the ropivacaine group compared with the control group (P < 0.05 for all). MAP was significantly lower at 6, 12, and 24 h (P < 0.05 for all); HR was significantly lower at 0, 6, 12, and 24 h (P < 0.05 for all); time to bowel recovery and length of hospitalization after surgery (P < 0.05 for both) were significantly shortened; and cumulative sufentanil consumption was significantly lower at 6, 12, 24, and 36 h (P < 0.05 for all) in the ropivacaine group than in the control group, although the incidence of nausea and vomiting showed no significant difference between the two groups. The levels of epinephrine, norepinephrine, and cortisol were significantly lower in the ropivacaine group than in the control group at 24 and 48 h (P < 0.01 for all).
Local wound infiltration with ropivacaine after open hepatectomy can improve postoperative pain relief, reduce surgical stress response, and accelerate postoperative recovery.
Core tip: This study prospectively evaluated the effect of local wound infiltration with ropivacaine on postoperative pain relief and stress response reduction after open hepatectomy. Wound infiltration with ropivacaine could provide more effective analgesia both at rest and on movement in the first 48 h after surgery, with lower mean arterial pressure, heart rate and sufentanil consumption, accelerated postoperative recovery, and reduced stress response. These results suggest that local wound infiltration with ropivacaine is a simple, convenient and effective analgesic method that can provide postoperative analgesia and short-term benefits after open hepatectomy.
- Citation: Sun JX, Bai KY, Liu YF, Du G, Fu ZH, Zhang H, Yang JH, Wang B, Wang XY, Jin B. Effect of local wound infiltration with ropivacaine on postoperative pain relief and stress response reduction after open hepatectomy. World J Gastroenterol 2017; 23(36): 6733-6740
- URL: https://www.wjgnet.com/1007-9327/full/v23/i36/6733.htm
- DOI: https://dx.doi.org/10.3748/wjg.v23.i36.6733
Postoperative pain is an important issue for surgeons, anesthetists, patients, and other related personnel. The intensive pain caused by upper abdominal laparotomy may influence postoperative recovery, prolong hospitalization, and cause stress response and complications, including respiratory and cardiovascular depression and gastrointestinal and neuroendocrine dysfunction[1,2]. Currently, intravenous analgesia or epidural analgesia (EA) with a patient-controlled analgesia pump is the most common analgesic approach for controlling postoperative pain after laparotomy[3]. Although favored after major laparotomy, patient-controlled intravenous analgesia (PCIA) can delay postoperative recovery because of nausea and vomiting, excessive sedation, and dizziness; moreover, this analgesic mode involves the risk of addiction with large opioid dosages over long periods[4,5]. As to EA, which provides better analgesia than PCIA, it is restricted by contraindications, epidural puncture failure, and side effects[6,7]. Therefore, finding other analgesic strategies with fewer potentially serious adverse effects will be beneficial for patients suffering from postoperative pain.
Postoperative analgesia is a crucial section of perioperative management, and local anesthetic methods are more effective than systemic analgesia regardless of the operation type[8]. Currently, wound infiltration with local anesthetics, which is a simple, effective, and inexpensive method, is performed in various surgical procedures and provides satisfactory analgesia without major side effects[9]. Ropivacaine and bupivacaine, as long-acting local anesthetics, are commonly used for local anesthesia and pain management in China[10]. Ropivacaine has the same analgesic effects as bupivacaine and levobupivacaine, but it is associated with a low incidence of motor block[11]. Thus, ropivacaine appears to be an important component for local anesthesia and postoperative analgesia. Meanwhile, surgical pain frequently increases the systemic stress response during the perioperative period, which can induce the excessive release of catecholamines (epinephrine and norepinephrine) and cortisol. Optimistically, local anesthesia provides considerable advantages over general anesthesia by suppressing catecholamines and cortisol levels[12].
In this study, we aimed to assess the effect of local wound infiltration with ropivacaine on postoperative pain control, mean arterial pressure (MAP), heart rate (HR), cumulative sufentanil consumption, incidence of nausea and vomiting, time to bowel recovery, and length of hospitalization after open hepatectomy. The changes of three stress hormones, namely, epinephrine, norepinephrine, and cortisol, were evaluated in patients undergoing wound infiltration with and without ropivacaine.
A total of 56 patients undergoing open hepatectomy, which was performed by the same experienced surgical team at the Department of Hepatobiliary Surgery of Qilu Hospital of Shandong University from January 2016 to March 2017, participated in this study. The study was approved by the Medical Ethics Committee of Qilu Hospital of Shandong University (No. 2017052), and written informed consent was obtained from all patients. The inclusion criteria included adult patients (aged 18-75 years) who would undergo open hepatectomy and were classified as grades I-III according to the American Society of Anesthesiologists (ASA) Physical Status Classification System. Patients with a history of known allergy to local anesthetics, chronic preoperative opioid consumption, or any other analgesic treatment for chronic pain before surgery, psychiatric or neurological diseases, or acquired or genetic hemostatic abnormality were excluded from the study.
On the day of surgery, the patients were randomly divided into two groups with a table of random numbers. Surgeons and patients were kept blinded to the assigned treatment groups throughout the study. Wound infiltration was performed with a 7.5 mg/mL ropivacaine solution in the ropivacaine group and with an isotonic saline solution in the control group. Solutions were prepared and provided by the anesthetist, and surgeons were blinded to patient allocation. When closing the abdomen at the end of the surgical procedure, 20 mL of the prearranged solution was used to infiltrate the subcutaneous tissues, deep muscular fascia, and parietal peritoneum. Moreover, one or two drainage tubes were routinely placed near the cutting surface of the liver and then pulled out and fixed on the abdominal skin. In the presence of tube incision or pulling of the tube during movement or when turning over, the surrounding tissues of the tube were also infiltrated with the solution. Infiltration was performed under direct vision by the surgeon. All patients were given unrestricted access to sufentanil through a 100 mL disposable patient-controlled analgesic (PCA) device containing 1 μg/mL sufentanil that was delivered at a rate of 2 μg/h and a bolus of 0.5 μg with a 15 min lockout time. When the skin was closed, the PCA pump was connected to the venous catheter and routinely removed 36 h after the operation.
The intensity of postoperative pain at rest was measured on a visual analogue scale (VAS) graded from 0 (no pain) to 10 (very severe pain) for the first 48 h after surgery. Movement pain was scored using VAS when coughing or turning over. Pain scores were recorded both by nurses and surgeons blinded to patient allocation. Pain measurements were performed at 0, 6, 12, 24, and 48 h after the surgery. Other variables were recorded, including time to bowel recovery, length of hospitalization after surgery, hemodynamic data represented by MAP and HR, cumulative sufentanil consumption, and postoperative nausea and vomiting (PONV). The three surgical stress hormones, namely, epinephrine, norepinephrine, and cortisol, were detected using commercial enzyme-linked immunosorbent assay kits (Cusabio Biotech Co., Ltd., Wuhan, China). Time to bowel recovery was defined as the time to first anal exhaust. PONV was recorded with a three-point rating scale: 1, no nausea and vomiting; 2, nausea without vomiting; 3, nausea with vomiting.
Statistical analyses were performed with SPSS 19.0 (SPSS Inc., Chicago, IL, United States). All data were checked for normal distribution and the results are expressed as mean ± SD for continuous variables. The t test, χ2 test, Fisher’s exact test, or analysis of variance was carried out where appropriate. P < 0.05 was considered statistically significant.
All patients successfully received the surgical procedure, including the wound infiltration with a prearranged solution. However, three patients (two in the ropivacaine group and one in the control group) were dropped from the study for postoperative bleeding and bile leakage; finally, 26 patients were enrolled in the ropivacaine group and 27 enrolled in the control group. The demographic characteristics of the patients assigned to the two groups were comparable in terms of age, gender, weight, ASA grade, incision length, and postoperative pathology, except for operation type, which showed a statistical difference but had no clinical significance (Table 1).
| Characteristic | Ropivacaine group | Control group | t/χ2 | P value |
| Age (yr) | 48.38 ± 11.74 | 49.59 ± 12.42 | -0.36 | 0.7176 |
| Gender | ||||
| Male/female | 18/8 | 18/9 | 0.04 | 0.8415 |
| Weight (kg) | 63.04 ± 9.21 | 66.04 ± 9.86 | -1.14 | 0.2583 |
| ASA grade | ||||
| I/II/III | 4/17/5 | 7/15/5 | 0.92 | 0.6298 |
| Incision length (cm) | 24.65 ± 1.83 | 24.22 ± 2.76 | 0.67 | 0.5075 |
| Operation type | ||||
| Left hepatectomy | 8 | 5 | 0.0086 | |
| Right hepatectomy | 13 | 8 | ||
| Mesohepatectomy | 1 | 0 | ||
| Caudate lobectomy | 2 | 1 | ||
| Irregular hepatectomy | 2 | 13 | ||
| Postoperative pathology | ||||
| Hepatocellular carcinoma | 22 | 18 | 0.3292 | |
| Intra-and extrahepatic cholangiolithiasis | 3 | 7 | ||
| Hepatic focal nodular hyperplasia | 1 | 1 | ||
| Hepatocellular adenoma | 0 | 1 |
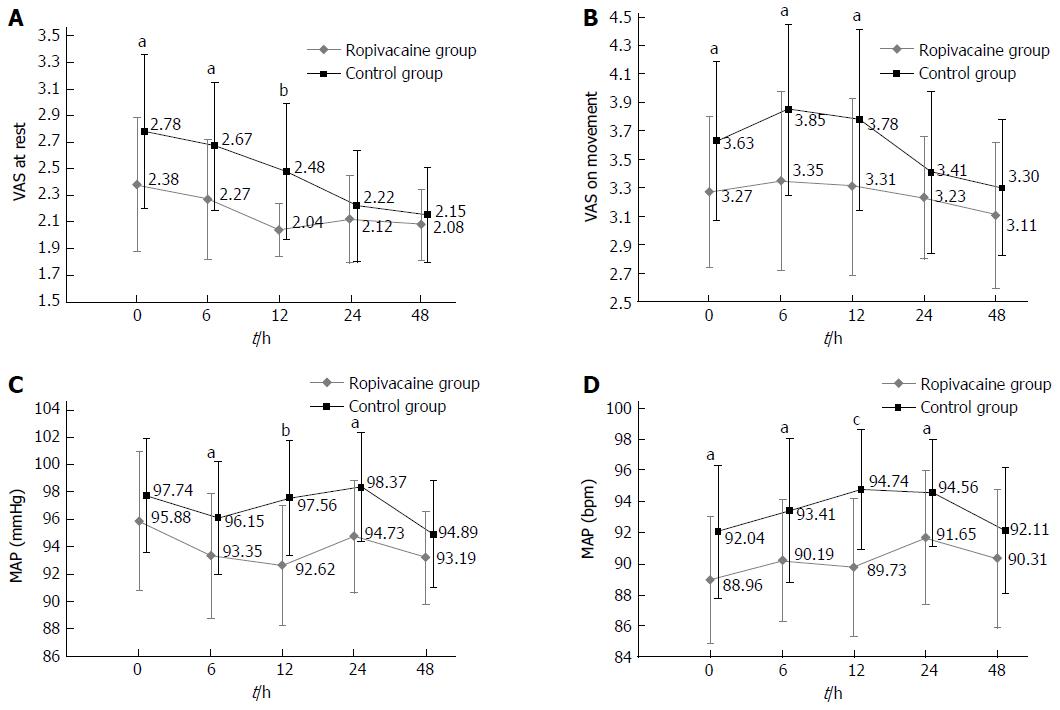
The VAS scores both at rest and on movement were similar between the two groups at 24 h and 48 h after open hepatectomy (Figure 1A and B). Significant differences in VAS scores at rest were detected at 0 h (P = 0.0106), 6 h (P = 0.0032), and 12 h (P = 0.0002). Moreover, significant differences in VAS scores on movement were observed at 0 h (P = 0.0208), 6 h (P = 0.0043), and 12 h (P = 0.0089). The details are shown in Table 2.
| Characteristic | 0 h | 6 h | 12 h | 24 h | 48 h1 |
| VAS at rest | |||||
| Ropivacaine group | 2.38 ± 0.50 | 2.27 ± 0.45 | 2.04 ± 0.20 | 2.12 ± 0.33 | 2.08 ± 0.27 |
| Control group | 2.78 ± 0.58 | 2.67 ± 0.48 | 2.48 ± 0.51 | 2.22 ± 0.42 | 2.15 ± 0.36 |
| t | -2.65 | -3.17 | -4.21 | -1.03 | -0.81 |
| P value | 0.0106 | 0.0032 | 0.0002 | 0.3096 | 0.4230 |
| VAS on movement | |||||
| Ropivacaine group | 3.27 ± 0.53 | 3.35 ± 0.63 | 3.31 ± 0.62 | 3.23 ± 0.43 | 3.11 ± 0.52 |
| Control group | 3.63 ± 0.56 | 3.85 ± 0.60 | 3.78 ± 0.64 | 3.41 ± 0.57 | 3.30 ± 0.47 |
| t | -2.39 | -2.99 | -2.72 | -1.27 | -1.34 |
| P value | 0.0208 | 0.0043 | 0.0089 | 0.2110 | 0.1857 |
| MAP (mmHg) | |||||
| Ropivacaine group | 95.88 ± 5.08 | 93.35 ± 4.63 | 92.62 ± 4.43 | 94.73 ± 4.16 | 93.19 ± 3.41 |
| Control group | 97.74 ± 4.17 | 96.15 ± 4.14 | 97.56 ± 4.23 | 98.37 ± 3.99 | 94.89 ± 3.90 |
| t | -1.46 | -2.32 | -4.16 | -3.25 | -1.69 |
| P value | 0.1515 | 0.0241 | 0.0001 | 0.0020 | 0.0981 |
| HR (bpm) | |||||
| Ropivacaine group | 88.96 ± 4.12 | 90.19 ± 3.92 | 89.73 ± 4.45 | 91.65 ± 4.30 | 90.31 ± 4.45 |
| Control group | 92.04 ± 4.27 | 93.41 ± 4.62 | 94.74 ± 3.88 | 94.56 ± 3.43 | 92.11 ± 4.05 |
| t | -2.66 | -2.73 | -4.37 | -2.72 | -1.54 |
| P value | 0.0103 | 0.0087 | < 0.0001 | 0.0089 | 0.1289 |
| Cumulative sufentanil consumption (μg) | |||||
| Ropivacaine group | 0 | 14.94 ± 2.56 | 30.40 ± 5.39 | 56.75 ± 6.20 | 83.02 ± 7.05 |
| Control group | 0 | 17.06 ± 3.81 | 35.50 ± 6.91 | 65.31 ± 7.09 | 91.39 ± 7.34 |
| t | -2.36 | -2.99 | -4.67 | -4.23 | |
| P value | 0.0220 | 0.0043 | < 0.0001 | < 0.0001 |
Hemodynamic data are presented in Figure 1C and D and Table 2. MAP was significantly lower in the ropivacaine group than in the control group at 6 h (P = 0.0241), 12 h (P = 0.0001), and 24 h (P = 0.002). In the ropivacaine group, HR was significantly lower at 0 h (P = 0.0103), 6 h (P = 0.0087), 12 h (P < 0.0001), and 24 h (P = 0.0089).
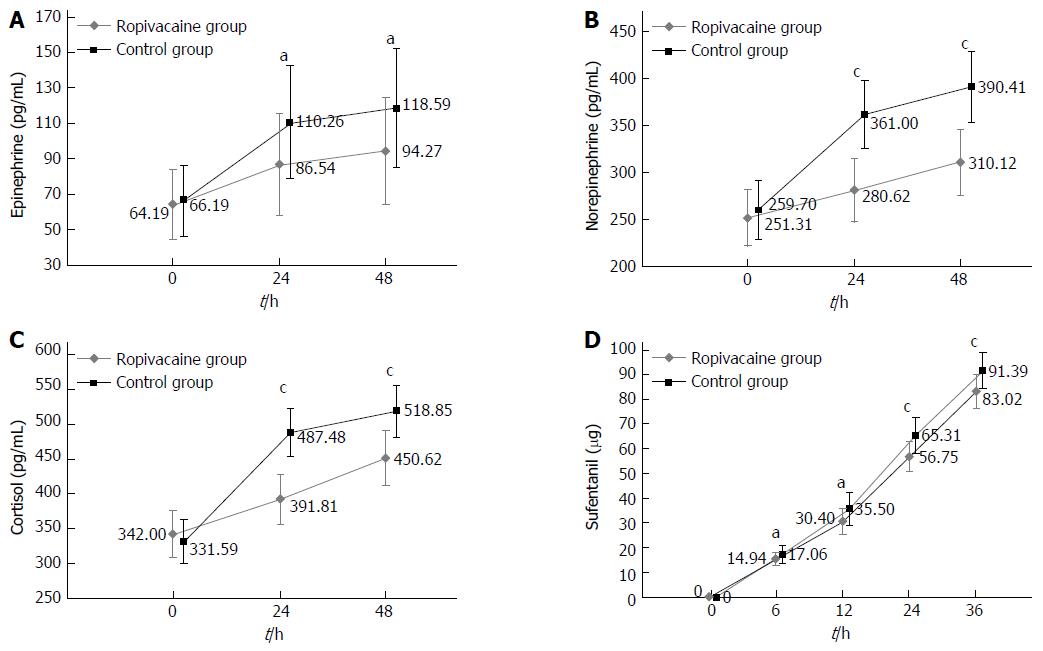
No statistically significant difference was observed in baseline levels (0 h) of epinephrine, norepinephrine, or cortisol between the two groups. The levels of epinephrine at 24 and 48 h were significantly lower in the ropivacaine group than in the control group (P = 0.0064, P = 0.0078). Similarly, the values of norepinephrine and cortisol at 24 and 48 h were significantly reduced in the ropivacaine group (P < 0.0001 for all), as shown in Figure 2A-C and Table 3.
| Stress hormone | 0 h | 24 h | 48 h |
| Epinephrine | |||
| Ropivacaine group | 64.19 ± 19.62 | 86.54 ± 28.64 | 94.27 ± 30.10 |
| Control group | 66.19 ± 20.30 | 110.26 ± 31.88 | 118.59 ± 33.65 |
| t | -0.36 | -2.85 | -2.77 |
| P value | 0.7180 | 0.0064 | 0.0078 |
| Norepinephrine | |||
| Ropivacaine group | 251.31 ± 30.19 | 280.62 ± 34.22 | 310.12 ± 35.15 |
| Control group | 259.70 ± 31.72 | 361.00 ± 36.06 | 390.41 ± 37.73 |
| t | -0.99 | -8.32 | -8.01 |
| P value | 0.3286 | < 0.0001 | < 0.0001 |
| Cortisol | |||
| Ropivacaine group | 342.00 ± 33.72 | 391.81 ± 36.53 | 450.62 ± 39.39 |
| Control group | 331.59 ± 31.92 | 487.48 ± 34.36 | 518.85 ± 38.21 |
| t | 1.15 | -9.82 | -6.40 |
| P value | 0.2537 | < 0.0001 | < 0.0001 |
Cumulative sufentanil consumption at 36 h after surgery is presented in Figure 2D and Table 2. The consumption was significantly lower in the ropivacaine group than in the control group at 6 h (P = 0.022), 12 h (P = 0.0043), 24 h (P < 0.0001), and 36 h (P < 0.0001). Even so, the incidence of nausea and vomiting, the side effects of sufentanil, between the two groups had no significant difference (Table 4). Moreover, in the ropivacaine group, time to bowel recovery (P = 0.0133) and hospitalization after surgery (P = 0.0289) were significantly shortened (Table 4).
| Characteristic | Ropivacaine group | Control group | t/χ2 | P value |
| Time to bowel recovery (d) | 3.15 ± 1.01 | 3.93 ± 1.17 | -2.56 | 0.0133 |
| PONA | ||||
| No PONA | 7 | 3 | 0.2729 | |
| Nausea without vomiting | 16 | 18 | ||
| Nausea with vomiting | 3 | 6 | ||
| Hospitalization (d) | 8.65 ± 2.43 | 10.52 ± 3.49 | -2.25 | 0.0289 |
Laparoscopic hepatectomy is commonly adopted in clinical settings because of its many advantages, including little trauma, low pain, fast recovery, and short hospitalization; however, open hepatectomy remains irreplaceable, especially in the presence of lesions close to or invading the root of the hepatic veins or the inferior vena cava, history of previous hepatectomy or any previous surgery potentially causing severe adhesion around the liver, and concomitant cardiopulmonary disease[13]. A right subcostal incision or reversed L-shaped incision (> 20 cm) is often made for open hepatectomy, and either of these two incision types is the most important source of postoperative pain. Thus, finding an effective way to reduce postoperative pain is urgent and necessary.
Local anesthetic wound infiltration is a useful and important component of a multimodality approach to postoperative pain control, and it can be applied in many types of surgery, including lumbar spine surgery, breast surgery, and inguinal hernia repair[9,14,15]. Local anesthetics used in the wound can block parietal afferents, reduce the sensitization of spinal dorsal horn neurons, and provide analgesia by inhibiting the transmission of noxious impulses from the incision[16]. Moreover, local anesthetics can suppress local inflammatory responses to incision injury that could sensitize nociceptive receptors and contribute to hyperalgesia[17]. Ropivacaine, a pure levorotatory stereoisomer and long-acting amide local anesthetic agent, has been widely used for local anesthesia and postoperative analgesia, and its reduced lipophilicity is associated with decreased incidence of central nervous system toxicity and cardiotoxicity[18]. Postoperative pain comes from superficial structures and deep muscular-peritoneal components; therefore, ropivacaine infiltrated not only the subcutaneous tissues but also the parietal peritoneum and deep muscular fasciae in our study. Our results showed that in the first 12 h after surgery, the local anesthetic ropivacaine significantly relieved the pain intensity at rest and on movement, demonstrating the potential of local wound infiltration with ropivacaine as a reliable analgesic strategy after open hepatectomy.
Surgical stress could cause a spectrum of changes in the body, involving the neuroendocrine, metabolic, immunological, and hematological systems[12]. The body’s surgical stress response is mainly determined by the surgical wound severity, including the length of the incision in the abdominal wall from the skin to the parietal peritoneum[19]. The incision of open hepatectomy often exceeds 20 cm, and the surgical stress is thought to be high. Therefore, using local anesthetics to block surgical stress is feasible. Surgical stress response to injury causes a series of hormone changes; moreover, catecholamines (epinephrine and norepinephrine) and cortisol, as the main and most reliable peripheral hormones, correlate well with the extent of surgical stress. In this study, surgical stress was significantly reduced in the first 48 h after surgery as revealed by the levels of epinephrine, norepinephrine, and cortisol. Changes in MAP and HR were recorded, and the results demonstrated that the indexes of the ropivacaine group were obviously decreased. These results indicate that local wound infiltration with ropivacaine could also reduce surgical stress responses.
Opioids are commonly used for postoperative analgesia via venous access. However, they are associated with a potential risk of addiction, especially in large doses over long periods. Moreover, opioids possess potentially serious side effects, such as nausea, vomiting, constipation, respiratory depression, excessive sedation, and liver function impairment; hence, sparing opioids may reduce the incidence of the above side effects[20]. Reducing the dosage and duration of opioid usage is regarded suitable for avoiding potentially serious adverse effects. Wound infiltration, as part of an opioid-sparing, multimodal analgesic regime, should therefore be recommended. Our current study showed that cumulative sufentanil consumption was significantly reduced in the ropivacaine group. Moreover, the time to bowel recovery was shorter in the ropivacaine group than in the control group. This may be caused by a combination of several reasons. First, sufentanil inhibits gut motility and propulsive activity by combining the μ-2 and κ receptors in the digestive tract[21]. Second, a previous animal study demonstrated that catecholamines reduce gut motility[22] and that the level of catecholamines in the ropivacaine group was reduced. Finally, ropivacaine could accelerate postoperative intestinal motility by reducing the inflammatory response.
The current study may have some limitations. The sample size was relatively small, and thus, more patients are needed in future studies to confirm our results. Compared with a previous study using catheters as a continuous wound infiltration method to deliver ropivacaine into the wound[23], we used single-shot ropivacaine infiltration into the superficial and deep muscular-peritoneal layers to achieve an analgesic effect. In our study, the drainage tube was routinely placed beside the liver resection surface and fixed outside. Movement and turning over could drag the tube and cause intensive pain, and thus, infiltration around the tube was highly effective. Moreover, the catheter under the wound could bring potential risks, such as infection and delayed wound healing, and the delivery rates and volumes of local anesthetics remain unidentified. Thus, single-shot infiltration with ropivacaine is a simple, convenient, and effective analgesic method that can bring short-term benefits for patients who underwent open hepatectomy. A previous study suggested that local anesthesia and stress response reduction could decrease cancer formation and that local anesthesia and analgesia may improve overall patient survival after oncologic surgery[24]. Thus, future research about local anesthesia, tumor recurrence, and patient survival after open hepatectomy is required.
In conclusion, local wound infiltration with ropivacaine after open hepatectomy can decrease acute postoperative pain and surgical stress response. This simple, convenient, and effective analgesic method provides postoperative analgesia and short-term benefits after open hepatectomy.
The postoperative pain caused by laparotomy delays patients’ recovery and incurs stress response. Although commonly used to control pain, intravenous analgesia and epidural analgesia still have their contraindications and side effects. Local wound infiltration is a simple and effective method that can provide satisfactory analgesia without major side effects. The current study was designed to evaluate the effect of local wound infiltration with ropivacaine on postoperative pain and stress response after open hepatectomy.
Postoperative analgesia is an indispensable component of fast track surgery for surgical patients, especially those who undergo laparotomy. Local anesthetics can effectively provide analgesia by inhibiting the transmission of noxious impulses from the wound and suppress local inflammatory responses to wound injury.
Wound infiltration with ropivacaine could provide effective analgesia in the first 48 h after open hepatectomy, with lower mean arterial pressure, heart rate and sufentanil consumption, accelerated postoperative recovery, and reduced stress response. These results suggest that this method is a simple, convenient and effective analgesic method that can provide postoperative analgesia and short-term benefits after open hepatectomy.
This study provides additional evidence supporting that local wound infiltration with ropivacaine after open hepatectomy can improve postoperative pain relief, reduce surgical stress response, and accelerate postoperative recovery.
The intensity of postoperative pain at rest was measured on a visual analogue scale graded from 0 (no pain) to 10 (very severe pain) after surgery. Postoperative nausea and vomiting was recorded with a three-point rating scale: 1, no nausea and vomiting; 2, nausea without vomiting; 3, nausea with vomiting.
The study was well written and its findings are informative. Local wound infiltration with ropivacaine has good effects for pain relief and stress response reduction after open hepatectomy.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Hashimoto N S- Editor: Gong ZM L- Editor: Wang TQ E- Editor: Zhang FF
| 1. | Wightman JA. A prospective survey of the incidence of postoperative pulmonary complications. Br J Surg. 1968;55:85-91. [PubMed] [Cited in This Article: ] |
| 2. | Latimer RG, Dickman M, Day WC, Gunn ML, Schmidt CD. Ventilatory patterns and pulmonary complications after upper abdominal surgery determined by preoperative and postoperative computerized spirometry and blood gas analysis. Am J Surg. 1971;122:622-632. [PubMed] [Cited in This Article: ] |
| 3. | Zhu Z, Wang C, Xu C, Cai Q. Influence of patient-controlled epidural analgesia versus patient-controlled intravenous analgesia on postoperative pain control and recovery after gastrectomy for gastric cancer: a prospective randomized trial. Gastric Cancer. 2013;16:193-200. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 38] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 4. | Hankin CS, Schein J, Clark JA, Panchal S. Adverse events involving intravenous patient-controlled analgesia. Am J Health Syst Pharm. 2007;64:1492-1499. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 45] [Cited by in F6Publishing: 47] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 5. | Choi JB, Shim YH, Lee YW, Lee JS, Choi JR, Chang CH. Incidence and risk factors of postoperative nausea and vomiting in patients with fentanyl-based intravenous patient-controlled analgesia and single antiemetic prophylaxis. Yonsei Med J. 2014;55:1430-1435. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 31] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 6. | Mohta M, Ophrii LE, Agarwal D, Bhatt S, Sethi AK, Chilkoti G. Vocal cord palsy: an unusual complication of paravertebral block. Anaesth Intensive Care. 2011;39:969-971. [PubMed] [Cited in This Article: ] |
| 7. | Lucas SD, Higdon T, Boezaart AP. Unintended epidural placement of a thoracic paravertebral catheter in a patient with severe chest trauma. Pain Med. 2011;12:1284-1289. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Wu CL, Cohen SR, Richman JM, Rowlingson AJ, Courpas GE, Cheung K, Lin EE, Liu SS. Efficacy of postoperative patient-controlled and continuous infusion epidural analgesia versus intravenous patient-controlled analgesia with opioids: a meta-analysis. Anesthesiology. 2005;103:1079-1088; quiz 1109-1110. [PubMed] [Cited in This Article: ] |
| 9. | Scott NB. Wound infiltration for surgery. Anaesthesia. 2010;65 Suppl 1:67-75. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 74] [Cited by in F6Publishing: 72] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 10. | Tam KW, Chen SY, Huang TW, Lin CC, Su CM, Li CL, Ho YS, Wang WY, Wu CH. Effect of wound infiltration with ropivacaine or bupivacaine analgesia in breast cancer surgery: A meta-analysis of randomized controlled trials. Int J Surg. 2015;22:79-85. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 30] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 11. | Li M, Wan L, Mei W, Tian Y. Update on the clinical utility and practical use of ropivacaine in Chinese patients. Drug Des Devel Ther. 2014;8:1269-1276. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Iwasaki M, Edmondson M, Sakamoto A, Ma D. Anesthesia, surgical stress, and “long-term” outcomes. Acta Anaesthesiol Taiwan. 2015;53:99-104. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 48] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 13. | Kawaguchi Y, Otsuka Y, Kaneko H, Nagai M, Nomura Y, Yamamoto M, Otani M, Ohashi Y, Sugawara K, Koike D. Comparisons of financial and short-term outcomes between laparoscopic and open hepatectomy: benefits for patients and hospitals. Surg Today. 2016;46:535-542. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 14. | Byager N, Hansen MS, Mathiesen O, Dahl JB. The analgesic effect of wound infiltration with local anaesthetics after breast surgery: a qualitative systematic review. Acta Anaesthesiol Scand. 2014;58:402-410. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 47] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 15. | Kjærgaard M, Møiniche S, Olsen KS. Wound infiltration with local anesthetics for post-operative pain relief in lumbar spine surgery: a systematic review. Acta Anaesthesiol Scand. 2012;56:282-290. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 39] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 16. | Brennan TJ, Zahn PK, Pogatzki-Zahn EM. Mechanisms of incisional pain. Anesthesiol Clin North America. 2005;23:1-20. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 110] [Cited by in F6Publishing: 122] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 17. | Kawamata M, Takahashi T, Kozuka Y, Nawa Y, Nishikawa K, Narimatsu E, Watanabe H, Namiki A. Experimental incision-induced pain in human skin: effects of systemic lidocaine on flare formation and hyperalgesia. Pain. 2002;100:77-89. [PubMed] [Cited in This Article: ] |
| 18. | Kuthiala G, Chaudhary G. Ropivacaine: A review of its pharmacology and clinical use. Indian J Anaesth. 2011;55:104-110. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 172] [Cited by in F6Publishing: 194] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 19. | Krikri A, Alexopoulos V, Zoumakis E, Katsaronis P, Balafas E, Kouraklis G, Karayannacos PE, Chrousos GP, Skalkeas G. Laparoscopic vs. open abdominal surgery in male pigs: marked differences in cortisol and catecholamine response depending on the size of surgical incision. Hormones (Athens). 2013;12:283-291. [PubMed] [Cited in This Article: ] |
| 20. | White PF. The changing role of non-opioid analgesic techniques in the management of postoperative pain. Anesth Analg. 2005;101:S5-S22. [PubMed] [Cited in This Article: ] |
| 21. | Ducrotté P, Caussé C. The Bowel Function Index: a new validated scale for assessing opioid-induced constipation. Curr Med Res Opin. 2012;28:457-466. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 35] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 22. | Fruhwald S, Herk E, Petnehazy T, Scheidl S, Holzer P, Hammer F, Metzler H. Sufentanil potentiates the inhibitory effect of epinephrine on intestinal motility. Intensive Care Med. 2002;28:74-80. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 23. | Xin Y, Hong Y, Yong LZ. Efficacy of postoperative continuous wound infiltration with local anesthesia after open hepatectomy. Clin J Pain. 2014;30:571-576. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 24. | Cata JP, Hernandez M, Lewis VO, Kurz A. Can regional anesthesia and analgesia prolong cancer survival after orthopaedic oncologic surgery? Clin Orthop Relat Res. 2014;472:1434-1441. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 27] [Article Influence: 2.7] [Reference Citation Analysis (0)] |