Published online Feb 21, 2016. doi: 10.3748/wjg.v22.i7.2398
Peer-review started: September 16, 2015
First decision: October 14, 2015
Revised: November 3, 2015
Accepted: December 12, 2015
Article in press: December 12, 2015
Published online: February 21, 2016
Gastrointestinal duplications are uncommon congenital malformations that can occur anywhere along the gastrointestinal tract. Most cases are recognized before the age of 2 years, and those encountered in adults are rare. We describe here a case of ascending colon duplication in a 20-year-old male that caused intussusception and was treated laparoscopically. Although computed tomography revealed a cystic mass filled with stool-like material, the preoperative diagnosis was a submucosal tumor of the ascending colon. We performed a laparoscopic right colectomy, and the postoperative pathological diagnosis was duplication of the ascending colon, both cystic and tubular components. We conclude that gastrointestinal duplications, although rare, should be considered in the differential diagnosis of all abdominal and submucosal cystic lesions and that laparoscopy is a preferred approach for the surgical treatment of gastrointestinal duplications.
Core tip: Gastrointestinal duplications are uncommon congenital malformations and are rarely encountered in adults. We describe an adult case of ascending colon duplication resected by laparoscopic right colectomy. We conclude that gastrointestinal duplications should be included in the differential diagnosis of all abdominal and submucosal cystic lesions and that laparoscopy is a preferred approach for the surgical treatment of gastrointestinal duplications.
- Citation: Kyo K, Azuma M, Okamoto K, Nishiyama M, Shimamura T, Maema A, Shirakawa M, Nakamura T, Koda K, Yokoyama H. Laparoscopic resection of adult colon duplication causing intussusception. World J Gastroenterol 2016; 22(7): 2398-2402
- URL: https://www.wjgnet.com/1007-9327/full/v22/i7/2398.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i7.2398
Gastrointestinal duplications are uncommon congenital malformations and are estimated to occur in 1 of 4500 births[1]. These malformations can occur anywhere along the gastrointestinal tract from the mouth to the anus, but the ileum is the most common site (30%-35%) and colonic duplications are rare (7%-20%)[2,3]. Most cases (67%-80%) are recognized before the age of 2 years as an acute abdomen or bowel obstruction, and those condition is rarely encountered in adults[2,3]. We describe here a case of adult colon duplication that caused intussusception and was treated by laparoscopic resection.
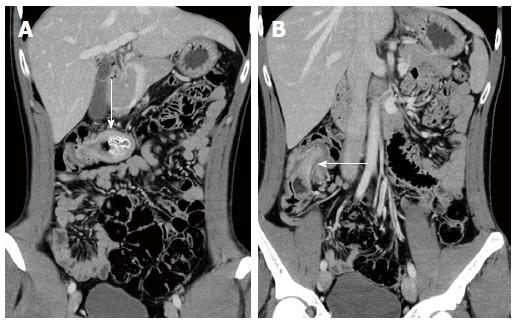
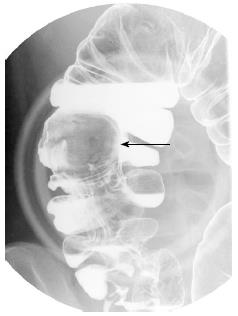
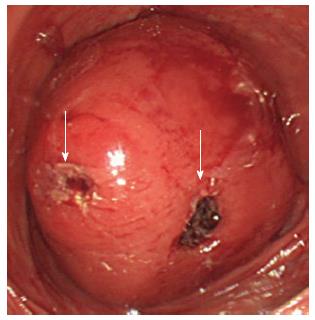
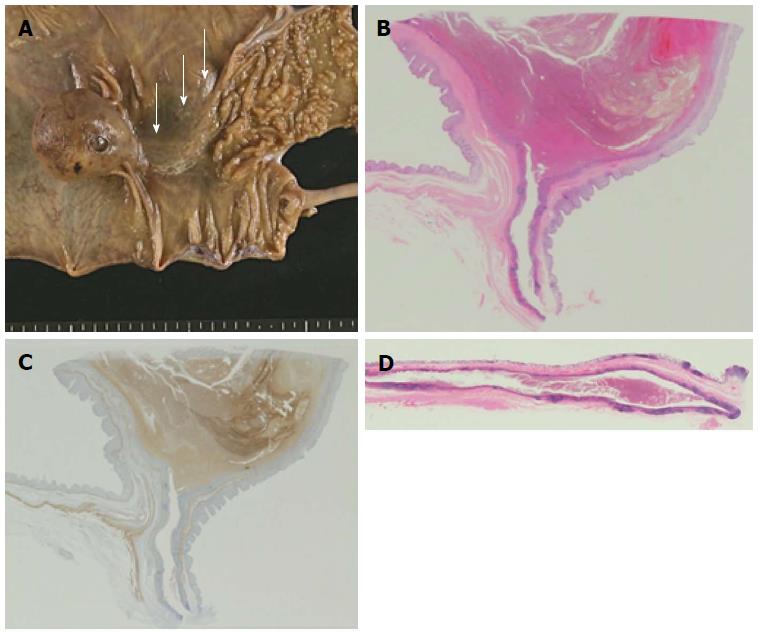
A 20-year-old otherwise healthy male was referred to our hospital because of a one-year history of intermittent right flank pain and a large submucosal mass in the ascending colon that had been observed by colonoscopy at a clinic. All laboratory tests performed resulted in values within the normal range. An abdominal computed tomography scan revealed intussusception of the right colon with a cystic mass 4 cm in diameter. Although stool-like material was observed within the mass, it did not lead to the diagnosis (Figure 1A and B). A barium enema showed a large submucosal mass in the ascending colon that originated near the ileocecal valve (Figure 2). Colonoscopy also revealed a large submucosal mass in the ascending colon, and two mucosal defects were observed on its surface (Figure 3). Histological examinations of biopsy specimens taken from one of the mucosal defects revealed only necrotic tissue. No other abnormalities were found in either physical or radiologic examinations. A neoplastic submucosal tumor causing intussusception was suspected, and a laparoscopic right colectomy with ileocolic anastomosis was performed. Intraoperatively, a round mass was observed in the hepatic flexure of the colon that caused an invagination of the ileocecal region into the ascending colon (Figure 4). No other abnormalities such as Meckel’s diverticulum or malrotation were found. Careful inspection of the resected specimen revealed not only a cystic submucosal mass 4 cm in diameter but also a submucosal tubular bulge measuring 5 cm in length and extending from the mass to the ileocecal valve (Figure 5A). Both the cystic and tubular parts of the lesion were on the mesenteric side. Histopathologically, both the cystic and tubular parts of the lesion were lined by with normal colonic mucosa; the cystic part had its own muscular layer, whereas the tubular part shared the muscular layer with the native ascending colon, which led to the diagnosis of colon duplication (Figure 5B-D). Both of the mucosal defects on the cystic lesion were communication sites with the native bowel, and the cystic lesion contained fecal material and blood clots. No neoplastic lesion or ectopic mucosa was identified. The postoperative course was uneventful, and the patient was discharged on post-operative day 7.
In 1876, Suppinger reported the first case of this congenital malformation, and in 1937, Ladd described in detail the clinical and pathological aspects of the lesions and recommended using the term “duplications of the alimentary tract”[4]. These lesions have 3 defined features: (1) well-formed smooth muscle layers; (2) an epithelial lining consisting of some portion of the alimentary tract; and (3) contiguity with a portion of the alimentary tract. There may or may not be communication with the gastrointestinal tract, and the dividing septum may be muscular or merely a double layer of epithelium[5]. Additionally, these malformations may be found in the intermuscular, submucosal or subserosal layer of the intestinal wall and are typically located on the mesenteric side of the bowel[6]. Duplications are divided into cystic (86%) and tubular types (14%), and the cystic lesion usually does not communicate with the lumen of the adjacent bowel and contains a sticky mucoid fluid that is chocolate or café au lait colored in some instances and almost colorless in others[2,4,7]. Tubular lesions often have one or more direct communications with the adjacent bowel and can appear either as double-barreled or Y-shaped forms. Gross et al[7] described four variations of the duplications: (1) a tubular structure that branches out from the intestine and extends for some distance between the mesenteric leaves; (2) a double-barreled structure communicating with the intestinal lumen at one or both ends; (3) a cystic structure lying free in the peritoneal cavity, attached only by a thin mesenteric stalk (this type is rare); and (4) most common, a spherical lesion contiguous with some part of the bowel, particularly along the ileum. Although both cystic and tubular parts were observed in the present case, we think it plausible that stool accumulation in the tubular duplication caused cystic dilatation that protruded into the intestinal lumen over the years; therefore, this case should be classified as a double-barreled tubular structure type. Similar cases have been reported in which the end of a Y-shaped tubular colonic duplication had become a large cystic mass containing stool[8,9].
Signs and symptoms of the duplications are nonspecific and depend on their location; oral and esophageal lesions may cause dysphagia and respiratory difficulties, and other intra-abdominal types may cause an abdominal mass, pain, constipation, intestinal obstruction, volvulus, intussusception, hemorrhage or perforation[2,6,7,10]. Hemorrhage often occurs from the ectopic ulcerating gastric mucosa in the duplication. Ectopic gastric mucosa was observed frequently in the duplications irrespective of their locations in the gastrointestinal tract (20%-50%) and was particularly common in esophageal duplications[2,3,6]. The occurrence of carcinoma in a duplicated cyst has also been reported, and 67% of malignancies occurred in colonic duplication, although colonic duplications are relatively rare[11].
Although no other abnormalities were found in the present case, 80% of patients with tubular colonic duplication have been reported to have associated anomalies; urogenital duplications are the most notable, and skeletal abnormalities, including malformations or duplications of the spine and sacrum, are also often observed[10,12]. The etiology of intestinal duplications and the associated anomalies is poorly understood, although several theories have been proposed[10].
The treatment of choice for duplications is surgical excision. Although the treatment strategy for asymptomatic cases is not clearly established, surgical excision is generally recommended to prevent the complications described above and the occurrence of malignancies. However, complete excision may not be possible for a long tubular duplication. In such a case, selective mucosal excision with preservation of the seromuscular layer[6,10,13] or distal internal drainage by excision of the common wall may be effective alternatives[2,3,10]. Although some recent studies have recommended the use of laparoscopy for the diagnosis and surgical treatment of gastrointestinal duplications, few have reported its use in surgery for duplications[2,14]. We believe that laparoscopic surgery, if possible, is a preferred approach because of its minimal invasiveness.
In conclusion, although gastrointestinal duplications, particularly adult cases are rare, they should be considered in the differential diagnosis of all abdominal and submucosal cystic lesions, and laparoscopy should be a preferred approach for the surgical treatment of gastrointestinal duplications. The differential diagnosis of other gastrointestinal cystic lesions can include heterotopic pancreas, lymphangiomas, cystic degeneration of solid tumors such as gastrointestinal stromal tumors and schwannomas, Brunner’s gland hyperplasia and gastritis cystica profunda[15-17]. The majority of duplications reported in the literature were unsuspected before surgery, and the diagnoses were established during or after the surgery. It is difficult to make a correct diagnosis without knowledge of the disease, and practitioners should be familiar with the characteristics of this disease.
A 20-year-old male was referred to our hospital because of a one-year history of intermittent right flank pain and a large submucosal mass in the ascending colon which had been observed by colonoscopy at a clinic.
Intermittent right flank pain.
A submucosal tumor of the ascending colon.
All labs were within normal limits.
CT showed intussusception of the right colon with a cystic mass 4 cm in diameter.
Ascending colon duplication.
Laparoscopic right colectomy.
Gastrointestinal duplications are uncommon congenital malformations, and those encountered in adults are rare. There are only a few reports on laparoscopic surgery for this condition.
Gastrointestinal duplications are uncommon congenital malformations that possess 3 defined features: (1) well-formed smooth muscle layers; (2) an epithelial lining consisting of some portion of the alimentary tract; and (3) contiguity with a portion of the alimentary tract.
Although gastrointestinal duplications, particularly adult cases are rare, they should be included in the differential diagnosis of all abdominal and submucosal cystic lesions.
This article presents a rare case of adult colon duplication that was treated by laparoscopic resection.
P- Reviewer: Kir G, Leao P, Leao P S- Editor: Yu J L- Editor: A E- Editor: Zhang DN
| 1. | Schalamon J, Schleef J, Höllwarth ME. Experience with gastro-intestinal duplications in childhood. Langenbecks Arch Surg. 2000;385:402-405. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 64] [Cited by in F6Publishing: 66] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 2. | Puligandla PS, Nguyen LT, St-Vil D, Flageole H, Bensoussan AL, Nguyen VH, Laberge JM. Gastrointestinal duplications. J Pediatr Surg. 2003;38:740-744. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 158] [Cited by in F6Publishing: 137] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 3. | Holcomb GW, Gheissari A, O’Neill JA, Shorter NA, Bishop HC. Surgical management of alimentary tract duplications. Ann Surg. 1989;209:167-174. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 218] [Cited by in F6Publishing: 243] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 4. | Ladd WE. Duplications of the alimentary tract. South Med J. 1937;30:363-371. [DOI] [Cited in This Article: ] [Cited by in Crossref: 88] [Cited by in F6Publishing: 89] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Smith JR. Accessory enteric formations: a classification and nomenclature. Arch Dis Child. 1960;35:87-89. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 45] [Cited by in F6Publishing: 49] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Iyer CP, Mahour GH. Duplications of the alimentary tract in infants and children. J Pediatr Surg. 1995;30:1267-1270. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 123] [Cited by in F6Publishing: 125] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 7. | Gross RE, Holcomb GW, Farber S. Duplications of the alimentary tract. Pediatrics. 1952;9:448-468. [PubMed] [Cited in This Article: ] |
| 8. | Chaiyasate K, Bruch S. Colonic duplication associated with anterior spinal bar and left-sided inferior vena cava. Surgery. 2007;141:823-825. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Ohno T, Shiogama T, Mochizuki S, Mizutani A, Tsurunaga Y, Fukui H, Aso N. Huge cystic communicating duplication of the right colon with perforated appendicitis. Surgery. 2005;137:477-479. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Stern LE, Warner BW. Gastrointestinal duplications. Semin Pediatr Surg. 2000;9:135-140. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 87] [Cited by in F6Publishing: 75] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 11. | Inoue Y, Nakamura H. Adenocarcinoma arising in colonic duplication cysts with calcification: CT findings of two cases. Abdom Imaging. 1998;23:135-137. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 45] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 12. | Yousefzadeh DK, Bickers GH, Jackson JH, Benton C. Tubular colonic duplication--review of 1876-1981 literature. Pediatr Radiol. 1983;13:65-71. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 67] [Cited by in F6Publishing: 68] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 13. | Ildstad ST, Tollerud DJ, Weiss RG, Ryan DP, McGowan MA, Martin LW. Duplications of the alimentary tract. Clinical characteristics, preferred treatment, and associated malformations. Ann Surg. 1988;208:184-189. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 145] [Cited by in F6Publishing: 158] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 14. | Kiu V, Liang JT. Laparoscopic resection of Y-shaped tubular duplication of the sigmoid colon: report of a case. Dis Colon Rectum. 2010;53:949-952. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 15. | Lee J, Park CM, Kim KA, Lee CH, Choi JW, Shin BK, Lee SJ, Choi D, Jang KT. Cystic lesions of the gastrointestinal tract: multimodality imaging with pathologic correlations. Korean J Radiol. 2010;11:457-468. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 23] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 16. | Deesomsak M, Aswakul P, Junyangdikul P, Prachayakul V. Rare adult gastric duplication cyst mimicking a gastrointestinal stromal tumor. World J Gastroenterol. 2013;19:8445-8448. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 16] [Cited by in F6Publishing: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 17. | Ikematsu Y, Nishiwaki Y, Kida H, Iwaoka Y, Nagashima S, Ozawa T, Hasegawa S, Okawada T, Waki S. Gastric outlet obstruction caused by a heterotopic pancreas in a pregnant woman: report of a case. Surg Today. 2003;33:952-955. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |