Published online Aug 21, 2016. doi: 10.3748/wjg.v22.i31.6987
Peer-review started: May 2, 2016
First decision: May 30, 2016
Revised: June 9, 2016
Accepted: July 6, 2016
Article in press: July 6, 2016
Published online: August 21, 2016
Pancreatic cancer is an extremely aggressive disease; although progress has been made in the last few years, the prognosis of these patients remains dismal. FOLFIRINOX is now considered a standard treatment in first-line setting, since it demonstrated an improved overall and progression-free survival vs gemcitabine alone. However, the enthusiasm over the benefit of this three-drug regimen is tempered by the associated increased toxicity profile, and many efforts have been made to improve the feasibility of this schedule. After a more recent phase III trial showing an improved outcome over gemcitabine, the combination of gemcitabine/nab-paclitaxel emerged as another standard first-line treatment. However, this treatment is also associated with more side effects. In addition, despite initial promising data on the predictive role of SPARC levels, recent studies showed that these levels are not associated with nab-paclitaxel efficacy. The choice to use this treatment over FOLFIRINOX is therefore a topic of debate, also because no validated biomarkers to guide FOLFIRINOX treatment are available. In the era of actionable mutations and target agents it would be desirable to identify molecular factors or biomarkers to predict response to therapy in order to maximize the efficacy of treatment and avoid useless toxic effects for non-responding patients. However, until today the milestone of treatment for pancreatic cancer remains chemotherapy combinations, without predictive or monitoring tools existing to optimize therapy. This review analyzes the state-of-the-art treatments, promises and limitations of targeted therapies, ongoing trials and future perspectives, including potential role of microRNAs as predictive biomarkers.
Core tip: The present manuscript is a review of the state of the art treatments, focusing on biomarkers, target therapies and future perspectives in order to develop personalized treatments.
- Citation: Caparello C, Meijer LL, Garajova I, Falcone A, Le Large TY, Funel N, Kazemier G, Peters GJ, Vasile E, Giovannetti E. FOLFIRINOX and translational studies: Towards personalized therapy in pancreatic cancer. World J Gastroenterol 2016; 22(31): 6987-7005
- URL: https://www.wjgnet.com/1007-9327/full/v22/i31/6987.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i31.6987
Pancreatic cancer is estimated to be the fourth leading cause of cancer-related death in the United States in both sexes; the prognosis in these patients is dismal with a 5-year relative survival rate of only 7%[1].
Because of nonspecific symptoms and its aggressive biological behavior, pancreatic cancer often presents as a locally advanced or metastatic disease.
Some progress has been made in the last few years leading to a longer overall survival (OS) in metastatic patients undergoing first-line chemotherapy treatment, although not all patients will benefit from this intense therapy. Currently, no predictive factors of response exist. Furthermore no genetic alterations in pancreatic cancer have been found that can be tackled with targeted therapy. Multiple targeted agents have been registered or are under promising clinical trials for several tumor types, but similar success has not occurred in pancreatic cancer. This therapeutic failure can be attributed to several causes, including a strong inter- and intra-tumor genetic and microenvironmental heterogeneity. Immunotherapy showed encouraging results in preclinical models, but often failed to demonstrate clear benefits in clinical trials for pancreatic cancer patients[2]. In a phase I study the CD40 agonist CP870893, was well tolerated in combination with gemcitabine, with 4 partial responses achieved among the 22 patients treated, warranting future phase II trials[3]. Similarly, the combination of chemotherapy and immunotherapy using two granulocyte macrophage colony-stimulating factor-secreting pancreatic cancer cell lines (CG8020/CG2505) alone or in sequence with cyclophosphamide showed minimal treatment-related toxicity associated with antitumor activity[4]. More recently, a trial on prime/boost vaccination with GVAX and CRS-207 showed a significantly longer survival (2.2 mo) compared with Cy/GVAX alone in patients with metastatic pancreatic cancer[5]. These results, showing a synergistic interaction between effects mediated by chemotherapy and the immune system, raise the question as to whether the success of FOLFIRINOX is potentially related to the combination of chemotherapy with additional, although not intentionally given for this purpose, immune modulation via G-CSF, which is administered to prevent neutropenia. These observations should guide further studies to investigate the right combination of immunotherapies and chemotherapy.
However, up to now the standard therapeutic approach in pancreatic cancer is represented by chemotherapy alone, and new biomarkers to optimize treatment selection are urgently warranted. The present review summarizes the main therapeutic options for pancreatic cancer, mostly focusing on recent regimens that represent the new standards in metastatic disease. Moreover, we describe biomarkers that have been reported to predict drug activity in pancreatic cancer, as well as novel potential biomarkers, such as microRNA (miRNA).
Until a few years ago, gemcitabine was considered as a standard of treatment for metastatic pancreatic cancer as it seemed to be more effective in clinical benefit than 5-fluorouracil (5-FU)[6]. However, the median OS with gemcitabine was 5.65 mo with a probability of surviving beyond 12 mo of 18% and a very low response rate of 5.4%.
Many attempts have been made in order to evaluate gemcitabine-based combinations: the combination of gemcitabine and capecitabine seemed to improve response rate and progression free survival (PFS) vs gemcitabine alone, but showed only a trend towards improved OS. Only the meta-analysis of two additional studies involving 935 patients showed a significantly improved survival[7]. Similarly, the combination of cisplatin and gemcitabine demonstrated a prolonged OS and PFS over gemcitabine alone, but not in a statistically significant measure[8]. The most recent meta-analysis, including 26 studies and 8808 patients, confirmed this result and showed only a trend and no statistically significant differences when comparing all the combinations with fluoropyrimidine and platinum compounds to gemcitabine monotherapy[9].
Of note, the EGFR tyrosine kinase inhibitor erlotinib showed a slightly increased OS and PFS when it was tested in combination with gemcitabine in a phase III study on 569 patients with unresectable pancreatic cancer[10]. The advantage, although statistically significant, was clinically not significant enough to change the clinical practice. Although skin rash was initially proposed as a surrogate marker of efficacy, it failed to identify patients with clinical benefit in a randomized phase II dose-escalation trial[11]. Therefore no predictive factor has yet been found to be related to the clinical response to erlotinib.
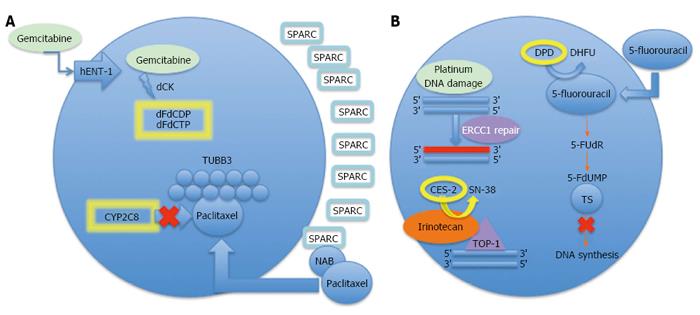
Several studies evaluated potential predictive factors of response to gemcitabine (Figure 1A). Because of its hydrophilic nature, gemcitabine does not cross the cellular membrane by diffusion, and it is transported by membrane nucleoside transporters[12]. After uptake in the tumor cells, gemcitabine is phosphorylated to its active diphosphate (dFdCDP) and triphosphate (dFdCTP) metabolites, which inhibit the enzyme ribonucleotide reductase (RR) and DNA synthesis, respectively[13].
The enzyme deoxycytidine kinase (dCK) catalyzes the rate-limiting step in the biotransformation of gemcitabine in its active phosphorylated form gemcitabine triphosphate (dFdCTP). Several studies have suggested that dCK plays a key role in gemcitabine activity, because its deficiency is critically involved in acquired resistance in different in vitro models[14,15]. Moreover, pretreatment dCK expression and activity levels could be used to predict tumor sensitivity; as observed with a clear correlation between dCK activity and gemcitabine sensitivity in tumor xenografts[16]. However, the fact that the transfection of the dCK gene in kinase-deficient cells only partially overcomes the resistance, suggesting the presence of additional mechanisms of resistance[17]. Clinically, low tumor dCK expression levels were associated with a significantly shorter OS and PFS in advanced pancreatic cancer patients treated with gemcitabine[18], but this evidence is limited by the small number of patients and failure to perform multivariate analysis.
Since dCK is saturated at relatively low gemcitabine levels and in vitro sensitivity to gemcitabine is most optimal at prolonged exposure to low drug levels in the nanomolar range[19], it was reasoned that prolonged infusion of gemcitabine would be advantageous. The fixed dose rate of 10 mg/m2/min infusion of gemcitabine gives this pharmacodynamic advantage, resulting in the optimal intracellular accumulation of dFdCTP, and several phase I trials evaluated the possibility to prolong the infusion duration[20-22]. Remarkably, a randomized phase II trial demonstrated that prolonged infusion at 10 mg/m2/min, compared to the standard dosing regimen, was associated with a significant increase in response rate and a trend for increased survival in metastatic pancreatic cancer[23]. However, this pharmacological advantage failed to translate into a survival advantage in the succeeding phase III study[24].
The most studied biomarker for gemcitabine activity in pancreatic cancer is the human equilibrative nucleoside transporter 1 (hENT1), which has been correlated to in gemcitabine responsiveness in both in vitro and in in vivo models of pancreatic cancer. Several clinical studies in patients with pancreatic carcinoma treated with gemcitabine demonstrated that the overexpression of hENT1 mRNA and protein correlated with significantly longer survival[25-27]. Furthermore the retrospective analysis of the phase III trials RTOG-9704 and ESPAC-1/3 demonstrated its role as a predictive biomarker of adjuvant gemcitabine efficacy: OS was significantly longer in patients treated with gemcitabine with high-hENT1 expression vs low-hENT1 expression. Importantly, these results were not seen in patients treated with 5-FU[27,28], suggesting a predictive more than prognostic role.
However, the first biomarker stratified trial (LEAP) with prospective analysis of hENT1 expression comparing gemcitabine vs its lipophilic analog CO-101 failed to demonstrate this correlation in metastatic disease[29]. In addition, immunohistochemistry analysis of the expression of hENT1 with the rabbit monoclonal antibody SP120 in patients’ tumor samples from the CONKO-001 phase III trial, that compared gemcitabine vs observation in adjuvant treatment, had similar results: no correlation between hENT1 expression and disease free survival (DFS) or OS was observed[30]. The reasons for these conflicting results are still unclear, and might either be due to the use of different types of hENT1 antibodies between studies, or to nonlinear protein expression pattern changes related to the disease-stage, since tumor genetic landscapes are highly dynamic during cancer progression. A validated immunohistochemical protocol and appropriate sampling, using metastatic cohorts, are required to further evaluate the role of hENT1 in predicting response to gemcitabine.
All the other studies evaluating various potential biomarkers for gemcitabine activity are retrospective, monocentric, without multiple correction or validation in broader populations. Moreover, most studies used different methods and specimens, without appropriate validation as well as evaluation of tumor heterogeneity and possible evolution of cancer cells after relapse[31]. In conclusion, after almost twenty years of use in the clinical practice, currently no prognostic biomarkers are available to stratify survival outcomes for pancreatic cancer patients receiving gemcitabine.
FOLFIRINOX is a combination of the chemotherapy agents 5-FU, leucovorin, irinotecan and oxaliplatin. This schedule was introduced as a novel standard in first-line treatment of metastatic pancreatic cancer after the publication of the PRODIGE 4/ACCORD 11 trial, which compared FOLFIRINOX with gemcitabine. The combination was first investigated in a phase I trial assessing the feasibility of FOLFIRINOX: most of the objective responses were found in gastrointestinal malignancies, in particular in two cases of pancreatic cancer[32]. In a phase II trial 46 patients receiving FOLFIRINOX for advanced pancreatic cancer showed a response rate of 26%, including 4% complete response. Median time to progression was 8.2 mo and median OS was 10.2 mo[33]. This regimen was further investigated in a phase III trial enrolling patients with metastatic pancreatic cancer, who were randomly assigned to receive FOLFIRINOX regimen or gemcitabine monotherapy. This randomized controlled trial consisting of 342 patients demonstrated an increased OS (11.1 mo vs 6.8 mo, P < 0.001) and PFS (6.4 mo vs 3.3 mo, P < 0.001) in favor of FOLFIRINOX, with an objective response rate of 31.6%. According to EORTC QLQ-C30, the quality of life was similar in both arms, but the time to deterioration of quality of life was significantly longer in FOLFIRINOX group for almost all domains. Unfortunately, FOLFIRINOX has shown a severe grade 3-4 toxicity profile with 45.7% of neutropenia, 5.4% of febrile neutropenia, 9.1% of thrombocytopenia, 14.5% of vomiting and 12.7% of diarrhea[34].
The doubts arising about the tolerability of FOLFIRINOX regimen prompted a review of the clinical data concerning the use of this regimen outside clinical trials[35]. Many attempts have been made in order to reduce the toxic effects, mostly related to the presence of a bolus of 5-FU. A modified FOLFIRINOX schedule has been used with concomitant prophylactic pegfilgrastim on 60 patients, showing a decrease of the incidence of grade 3-4 neutropenia to 3%, with a satisfactory response rate of about 30%[36]. The toxic effects decreased as well by lowering the starting dose of FOLFIRINOX to 80% and using the granulocyte growth factor. The efficacy of treatment was similar to the original schedule: 40% of the patients with metastatic disease achieved partial response[37].
FOLFORIXI is a similar schedule with minimal adjustments that was developed for colorectal cancer. FOLFORIXI does not include the 5-FU bolus, while it includes a higher dose of 5-FU continuous infusion and a slightly lower dose of irinotecan[38-40]. The FOLFOXIRI regimen (irinotecan 165 mg/m2, oxaliplatin 85 mg/m2, leucovorin 200 mg/m2 followed by fluorouracil 3200 mg/m2 as a 48-h continuous infusion) and a modified schedule (irinotecan 150 mg/m2, oxaliplatin 85 mg/m2, leucovorin 200 mg/m2 followed by 5-FU 2800 mg/m2 as a 48-h continuous infusion) were recently used in 137 stage III and IV pancreatic cancer patients. One complete response (0.6%) and 52 (38%) partial responses were observed in the whole study population, with a disease control rate of 72.2%, median OS was 12 mo in the entire study population and median PFS 8 mo. The toxicity profile was manageable: the main hematologic grade 3-4 toxicity was neutropenia (35.7%), but only one patient (0.7%) experienced febrile neutropenia. The main grade 3-4 non-hematological adverse events were grade 3 diarrhea in 11 (8%), nausea in 10 (7.3%), stomatitis in 9 (6.5%) and liver toxicity in 6 (4.4%) patients[41].
Several clinical prognostic factors have been identified in the FOLFIRINOX phase III trial: in the univariate analysis ECOG PS 1, male gender, body or tail primary tumor, hepatic metastases, synchronous metastases, and low baseline albumin were identified as independent negative prognostic factors[34]. However, in the multivariate analysis synchronous metastases, hepatic metastases, low baseline albumin level (< 3.5 g/dL) and age > 65 years were identified as independent negative prognostic factors for overall survival, using the Cox regression model stratified on ECOG performance status and location of primary tumor and adjusted on pulmonary metastases, as summarized in the Table 1.
| Prognostic factors for metastatic pancreatic patients treated with | |
| Gemcitabine-nab-paclitaxel | FOLFIRINOX |
| Age < 65 yr | Age > 65 yr |
| (HR = 0.81; P = 0.019) | (HR = 1.47; P < 0.019) |
| Hepatic metastases | Hepatic metastases |
| (HR = 1.81; P < 0.001) | (HR = 1.58; P = 0.051) |
| Number of metastatic sites > 3 | Synchronous metastases |
| (HR = 1.08; P = 0.86) | (HR = 2.47; P < 0.003) |
| KPS score, 70-80 vs 90-100 | Low baseline albumin level |
| (HR = 1.60; P < 0.001) | (HR = 1.85; P < 0.001) |
| Region - Eastern Europe | |
| (HR = 1.22; P = 0.077) | |
Similar to the previous gemcitabine-based regimens, clinicians are lacking predictive biological markers to help choosing which individual patient will benefit from FOLFIRINOX or FOLFIRINOX-modified treatments.
Potential candidates include determinants of drug metabolism and activity (Figure 1B), such as the enzyme of 5-FU catabolism dihydropyrimidine dehydrogenase (DPD), and the target enzyme thymidylate synthase (TS)[42]. For instance, Kurata et al[43] analyzed 15 pancreatic cancer cell lines and two 5-FU-resistant sub-lines to demonstrate a significant association between 5-FU sensitivity and the mRNA expression of both TS and DPD. These data suggests that pancreatic cancer cells with high TS and/or DPD levels are more resistant to 5-FU. An immunohistochemical analysis of 68 resected pancreatic cancer tissues showed that patients with low DPD protein levels reached a significantly higher survival rate when treated with adjuvant 5-FU liver perfusion chemotherapy[44]. However, no data on the prognostic value of DPD are currently available for the metastatic disease. Another immunohistochemical study evaluated TS expression both in primary and metastatic lesions. Surprisingly, in resectable patients, high TS expression levels were significantly correlated with a longer OS rate, vs lower OS for negative or low TS expression levels. Conversely, high TS immunoreactivity did not significantly influence the OS of the patients with unresectable tumors, nor was an independent prognostic factor[45].
Data on potential biomarkers for the efficacy of platinum compounds in metastatic pancreatic cancer are still unclear (Figure 1B). It has been demonstrated that cells able to repair platinum-DNA adducts present a profile of resistance to these drugs. The nucleotide excision repair (NER) system, which consists of at least 30 identified polypeptides, including ERCC1 and XPD, play a key role in removal of damaged DNA[46]. A recent study in patients receiving upfront off-protocol gemcitabine/oxaliplatin plus erlotinib, showed that high ERCC1 expression correlated with response rate. However, due to the small number of patients (n = 51) evaluable for immunohistochemical staining, the correlation with OS did not reach the level of statistical significance[47]. Furthermore, the clinical role of ERCC1 staining as a biomarker for resistance to platinum drugs is limited by methodological issues since immunohistochemical analysis with the currently available ERCC1 antibodies is not specific to detect the unique functional ERCC1 isoform[48]. Previous studies in more than 240 metastatic patients treated with cisplatin/capecitabine/gemcitabine-based polychemotherapeutic regimens showed that patients harboring the XPD Gln751Gln genotype had a worse prognosis[49,50]. A subgroup of patients treated with gemcitabine monotherapy lacked a correlation between XPD-Lys751Gln polymorphism and outcome, suggesting that the NER system does not affect the repair of gemcitabine-induced DNA damage. No data are available on subgroups of patients treated only with platinum compounds. Therefore, the role of this specific polymorphism in the activity of regimens with platinum compounds combined with different anticancer agents is yet unclear.
Finally, a few studies evaluated some potential biomarkers of irinotecan in pancreatic cancer cells and tissues (Figure 1B). Resistant pancreatic tumor cells have shown decreased mRNA levels of the irinotecan target topoisomerase-I (TOP1) compared to their parental cell lines[51]. However, neither expression of TOP1, nor expression of the molecules that are involved in its export (ABCB1, ABCC2) or inactivation (CYP3A4, CYP3A5, UGT1A10), yielded a statistically significant correlation with irinotecan sensitivity in a panel of pancreatic cancer cell lines[52]. A recent study showed that 30% of pancreatic cancer tissues have increased TOP1 copy numbers suggesting further analyses on the association between TOP1 gene copy number and irinotecan efficacy in the clinical setting[53]. A more comprehensive study including in vitro, in vivo models as well as extensive analyses of genetic databases, proteomics and tissue microarrays (TMAs) focused on carboxyl esterase-2 (CES2), which activates irinotecan into SN-38. This study showed that high expression of CES2 was associated with longer OS and PFS in resectable and borderline resectable patients treated with FOLFIRINOX in the neoadjuvant setting[52]. Remarkably, this is the first study reporting the associating of molecular features of pancreatic tumors and outcome of FOLFIRINOX treatment. However, the univariate and multivariate analyses were limited by the small number of patients (n = 22). Moreover, the expression data of resectable patients might not be comparable to the data from a population of patients suffering from metastatic disease. Therefore, other potential biomarkers of FOLFIRINOX therapy remain to be explored, especially in the metastatic setting.
In September 2013, the United States Food and Drug Administration approved the cytotoxic agent nab-paclitaxel for first-line treatment of patients with metastatic adenocarcinoma of the pancreas in combination with gemcitabine.
Nab-paclitaxel is a nanoparticle albumin-bound paclitaxel, which seems to achieve an higher tumor accumulation vs paclitaxel, by both of the lack of drug-sequestering solvent micelles and the albumin-mediated transcytosis[54]. The presence of albumin-binding proteins, such as secreted protein acidic and rich in cysteine (SPARC), which is overexpressed in the stromal fibroblasts surrounding the tumor tissue, is another hypothesized mechanism to be responsible of the higher tumor accumulation of this drug[55].
A few potential molecular mechanisms underlying the synergistic effect of the combination of nab-paclitaxel and gemcitabine have also been identified. Evidence suggests that Nab-paclitaxel targets tumor stroma, which represents a substantial barrier to the perfusion and diffusion of gemcitabine[56,57]. The synergistic effect also seems to be related to the inactivation by nab-paclitaxel of cytidine deaminase: a gemcitabine catabolizing enzyme, which increases, as a consequence, intratumoral gemcitabine levels[58].
The efficacy and safety data of the combination of nab-paclitaxel and gemcitabine were tested in a phase I-II study, enrolling a total of 67 patients. The median PFS for all patients was 7.1 mo with a median OS of 10.3 mo. Hematologic grade 3 toxicities were quite common, comprising 67% of neutropenia and 23% of thrombocytopenia Interestingly, the response rate was 46%. Furthermore, in the 36 patients evaluable for SPARC, high SPARC expression correlated with significantly longer OS[59].
After this promising phase I-II trial, the phase III trial enrolled 861 patients, which were randomized to receive the combination of nab-paclitaxel and gemcitabine or gemcitabine monotherapy. The median OS was 8.5 mo vs 6.7 mo, respectively, favouring the combination of nab-paclitaxel and gemcitabine (P < 0.001). The PFS was significantly longer for the combination of nab-paclitaxel and gemcitabine (5.5 mo vs 3.7 mo, P < 0.001)[60]. A list of prognostic factors is reported in the Table 1.
To investigate a potential predictive/prognostic role of SPARC expression, tissue was collected in this study. Using an immunohistochemical assay, 86% concordance was reported compared to the assay employed in the phase I/II trial. SPARC was measured in the tumor stroma (256 patients), tumor epithelia (301 patients) and plasma (343 patients). Stromal SPARC was deemed as high in 71 patients and low in 185 patients and was not associated with OS, both in the univariate and in the multivariate analysis. Similarly, epithelia and plasma SPARC were not associated with outcome. Therefore, SPARC failed as a predictive biomarker and as a potential selection criteria for treatment with nab-paclitaxel[61].
Two recent studies revealed that depletion of stromal cells can lead to a more biologically aggressive form of PDAC with poorly differentiated histology, increased vascularity and proliferation. In contrary depletion of carcinoma-associated fibroblasts (CAFs) induces immunosuppression and is associated to epithelial to mesenchymal transition[62]. These data suggest that stromal factors can differentially influence PDAC growth and further studies on the potential prognostic and/or predictive role of components of both the tumor and its microenvironment are warranted.
Other potential biomarkers have been explored among key determinants of paclitaxel activity (Figure 1A). In particular, the role of tubulin in resistence to taxane therapy has been widely investigated. Class III beta-tubulin (TUBB3) seems to be involved in taxane-based chemo-resistance and linked to taxane resistance in NSCLC. In addition, in stage III and IV NSCLC, receiving taxanes or other chemotherapy agents, beta-tubulin has been assessed by immunohistochemistry on tumor samples. Low tumor levels of class III B-tubulin isotype had a better response rate, longer PFS and OS, and this variable was not found to be predictive in patients receiving regimens without taxanes[63]. The role of tubulin expression was also investigated in gastric cancer: 146 gastric cancer patients receiving taxane-based chemotherapy showed a significantly shorter median PFS if TUBB3 expression was high, compared to low TUBB3 expression; in multivariate analysis TUBB3 expression was related to a shorter PFS[64].
Cytochrome P450 CYP2C8 is the main enzyme in the metabolic inactivation of paclitaxel. In vitro studies showed induction of this enzyme in cells with acquired resistance to paclitaxel[65] and that recombinant CYP2C8*3 is less efficient in paclitaxel metabolism than the CYP2C8*1 allele. However, this polymorphism was not statistically significantly correlated to OS in 119 patients treated for ovarian cancer with paclitaxel/carboplatin[66].
Pancreatic cancer is a tumor characterized by a dense stromal component. The stroma comprises many components, both cellular and acellular: pancreatic stellate cells, immune cells, fibroblast, myofibroblast, blood vessels and extracellular matrix. All these heterogeneous components within the tumor microenvironment, seem to be involved in cancer proliferation, metastasis and resistance to therapy[67]. For instance, the formation of the extracellular matrix, made up of proteoglycans, hyaluronic acid and collagen, has several consequences on blood vessels distribution inside the tumoral lesion[68]. The excessive accumulation of hyaluronic acid increases the interstitial fluid pressure compressing the blood vessels, consequently causing reduced drug delivery and chemoresistance[57]. Against this background, drugs targeting the stromal compartment are therefore under extensive investigation, as well as drugs targeting several key pathways emerging from the deep molecular profiling provided by the most recent genetic analyses. A list of the phase III trials with new experimental compounds performed in pancreatic cancer is presented in the Table 2.
| Ref. | Treatment arms | Patients | Results |
| Kindler et al[69] J Clin Oncol 2010 | Gemcitabine + bevacizumab vs gemcitabine + placebo | 302 | OS: 5.8 mo vs 5.9 mo (P = 0.95) |
| PFS: 3.8 mo vs 2.9 mo (P = 0.07) | |||
| 300 | RR: 13% vs 10% (P = NR) | ||
| Van Cutsem et al[70] J Clin Oncol 2009 | Erlotinib + gemcitabine + bevacizumab vs erlotinib + gemcitabine + placebo | 306 | OS: 7.1 mo vs 6.0 mo (P = 0.2087) |
| PFS: 4.6 mo vs 3.6 mo (P = 0.0002) | |||
| 301 | RR: 13.5% vs 8.6% (P = 0.0574) | ||
| Rougier et al[71] Eur J Cancer 2013 | Gemcitabine + aflibercept vs gemcitabine + placebo | 271 | OS: 6.5 mo vs 7.8 mo (P = 0.2034) |
| PFS: 3.7 mo vs 3.7 mo (P = 0.8645) | |||
| 275 | RR: NR | ||
| Kindler et al[73] Lancet Oncol 2011 | Gemcitabine + axitinib vs gemcitabine + placebo | 316 | OS: 8.5 mo vs 8.3 mo (P = 0.5436) |
| PFS: 4.4 mo vs 4.4 mo (P = 0.5203) | |||
| 316 | RR: 5% vs 2% (P = 0.0180) | ||
| Gonçalves et al[74] Ann Oncol 2012 | Gemcitabine + sorafenib vs gemcitabine + placebo | 52 | OS: 8.0 mo vs 9.2 mo (P = 0.231) |
| PFS: 3.8 mo vs 5.7 mo (P = 0.902) | |||
| 52 | RR: 23% vs 19% (P = NR) | ||
| Philip et al[94] J Clin Oncol 2010 | Gemcitabine + cetuximab vs gemcitabine | 372 | OS: 6.3 mo vs 5.9 mo (P = 0.19) |
| PFS: 3.4 mo vs 3.0 mo (P = 0.18) | |||
| 371 | RR: 14% vs 12% (P = 0.59) |
Although vascular pattern seems to be basically altered in pancreatic cancer and this type of tumor seems to be able to survive despite a relatively low blood flow, the vascular endothelial growth factor (VEGF) pathway has been targeted in several studies.
The anti-VEGF antibody bevacizumab was used in pancreatic cancer in combination with gemcitabine in two phase III studies. In a first study bevacizumab was combined with gemcitabine in a phase III placebo controlled study, without obtaining any advantage both in PFS and OS[69]. Given the improved OS registered with the combination of gemcitabine and erlotinib, bevacizumab was also tested in combination with this doublet: 301 patients received the gemcitabine, erlotinib and placebo combination and 306 patients received the combination containing bevacizumab. A statistically significant increase in PFS emerged, but improvement of the primary endpoint (OS) was not met[70]. Despite these failures, a phase III study tested the combination of gemcitabine with aflibercept, which is a recombinant fusion protein consisting of VEGF-binding portions from the extracellular domains of human VEGF receptors (VEGFR) 1 and 2. Unfortunately this trial was ended prematurely for futility after an interim analysis of OS[71].
Other clinical trials evaluated small molecules, such as axitinib. Axitinib is an oral inhibitor of VEGFR-1, 2 and 3. This was tested in a randomized phase II trial in combination with gemcitabine vs gemcitabine monotherapy. A longer but not statistically significant OS was detected with the combination therapy of gemcitabine and axitinib (6.9 mo vs 5.6 mo)[72]. Subsequently, a phase III trial was started comparing gemcitabine plus axitinib or placebo. No difference was observed in the OS of the patients treated within these two arms (8.5 mo vs 8.3 mo) and concluded that axitinib was deemed not effective in pancreatic cancer[73].
The multi-target kinase inhibitor sorafenib acts by inhibiting both VEGFR-2 and VEGFR-3, and PDGFR and RAF kinase. This results in an antiangiogenic action as well as in the disruption of the KRAS-BRAF-MEK-ERK pathway. Given the high prevalence of KRAS mutations in pancreatic cancer the use of this compound has a strong rationale. Despite these premises no advantage in PFS or OS emerged when combining sorafenib with gemcitabine in the phase III BAYPAN study[74]. These disappointing results could be explained by upregulation of pathways that may circumvent BRAF inhibition, particularly in KRAS-mutated tumors, as demonstrated in preclinical melanoma models[75].
Notably, all these trials demonstrated negative results in using anti-VEGF pathway compounds, suggesting that pancreatic cancer is independent from conventional angiogenesis. However, all these studies used an unselected population, without identifying a predictive biomarker of response, also because no validated biomarkers of antiangiogenic therapies are available for routine clinical use. Research on biomarkers that can guide for successful anti-angiogenesis treatments represents an important challenge not only for pancreatic cancer.
With the emergence of the pancreatic cancer microenvironment as an essential ingredient of this malignancy, therapies targeting its dense stromal reaction have begun to be designed and applied in the clinic.
Remarkably, nab-paclitaxel was designed as a cytotoxic agent directed to SPARC, and so targeting a stroma component. Data about the stromal disruption after nab-paclitaxel are promising: in 16 patients with resectable pancreatic cancer who underwent two cycles of nab-paclitaxel and gemcitabine the tumor response was evaluated by PET scan and CA19.9 levels, while the effect on tumor stroma was evaluated by Endoscopic Ultrasound Elastography (EUS) and on the histology specimen after resection. The results were compared with untreated patients or patients treated with conventional therapy. A significant decrease in tumor stiffness was detected by EUS, and the analysis of the tumor stroma in resected specimens showed disorganized collagen and low density of CAFs[76].
An interesting target among stroma components is hyaluronic acid, which can be targeted by PEGylated Recombinant Human Hyaluronidase (PEGPH20). This agent has been tested in combination with gemcitabine in a phase Ib study enrolling 28 patients: the PFS and OS for the entire population were respectively 5.0 and 6.6 mo. In a subgroup of patients (n = 17), the tissue hyaluronan (HA) levels at baseline were evaluated. Interestingly, PFS and OS were 7.2 and 13.0 mo for "high"-HA expressing patients[77]. A randomized phase IB/II study evaluating the addition of PEGPH20 to modified FOLFIRINOX vs modified FOLFIRINOX alone is currently recruiting patients[78]. The interim results of another randomized phase II study in metastatic pancreatic cancer patients treated with the combination of gemcitabine and nab-paclitaxel with PEGPH20 or the standard doublet alone, already showed that patients with high HA levels had significantly better ORR and PFS when treated with the triplet-drug combination than with nab-paclitaxel and gemcitabine alone. This evidence supports future studies to investigate HA as a predictive factor of response[79].
Despite these promising results, stromal depletion strategies should be used with caution[80]. Deletion of Sonic Hedgehog (Shh) can decrease the stromal component in PDAC, but might also contribute to a more aggressive tumor behavior. By deleting Shh in a mouse model, the reduced stromal component was indeed coupled to increased aggressiveness and vascularity of the tumor. Additionally, a VEGFR inhibitor selectively improved survival in Shh-deficient tumors, suggesting that some component of the stroma can limit the tumor growth by suppressing angiogenesis[81]. These data might explain the negative results obtained with the Shh inhibitor, IPI926, which has been investigated in phase I and phase II trials. The first study, that tested IPI926 in combination with FOLFIRINOX was prematurely ended, despite a good response rate of 67%, due to a separate phase II study in combination with gemcitabine that demonstrated a detrimental effect of the combination[82].
Another potential target is the connective tissue growth factor (CTGF), that is usually overexpressed in the stroma surrounding pancreatic cancer[80]. The use of the monoclonal antibody FG-3019 targeting the CTGF increased the response to gemcitabine in murine models of pancreatic cancer[83]. In the clinical setting, FG-3019 has been combined to gemcitabine and erlotinib in 75 locally advanced and metastatic pancreatic cancer patients. The combination was well tolerated and the OS for the whole study population was 9.4 mo, with 3% of complete response and 52% of partial response rate[84]. Therefore, a phase I/II trial of gemcitabine plus nab-paclitaxel with or without FG-3019 as neoadjuvant chemotherapy in locally advanced, unresectable pancreatic cancer is currently ongoing[85]. Remarkably, the baseline plasma CTGF correlated inversely with OS, warranting further investigation. A randomized phase II trial of FG-3019 combined with gemcitabine plus nab-paclitaxel vs chemotherapy alone in patients with marginally inoperable pancreatic cancer is currently recruiting patients[86]. Finally, a phase I trial on the χ-secretase inhibitor MK-0752, that blocks the NOTCH pathway, administered in combination with gemcitabine, in patients with with Stage IV pancreatic ductal adenocarcinoma showed the feasibility of this combination and the initial data on clinical activity prompted further investigations, especially in patients who initially respond to and tolerate gemcitabine well, but develop resistant disease[87].
Co-expression of EGFR and HER-2 receptor has been related to invasion and worse clinical outcome in pancreatic cancer[88]. Furthermore, strong HER-3 expression seems to be related to short survival[89]. A report that investigated the co-expression of HER-2 (by immunohistochemistry and FISH) in EGFR positive pancreatic cancer, suggested that HER-2 is an important cooperating member of the EGFR pathway since overexpression of HER-2 was detected in 17% of the whole population and 24% of EGFR-overexpressing tumors. Conversely none of EGFR negative tumors had a overexpressed or amplified HER-2[88]. The subsequent trial on the combination of the monoclonal anti-HER-2/neu receptor trastuzumab with gemcitabine showed HER-2 overexpression in about 16% of the samples. In agreement with previous favourable results in breast cancer[90], the patients were selected according to the immunohistochemistry expression of HER-2 (2+ and 3+). However, partial response was reported in only 6% of patients, and the median OS was 7 mo[91]. Trastuzumab was also tested in combination with capecitabine in a phase II trial. This study reported HER-2+ and 3+ overexpression or gene amplification in 11% of patients, but only 64% of patients with HER-2 and 3+ expression showed gene amplification. The effect on the PFS and OS were not satisfactory, so further evaluation of this targeted therapy was not suggested by the authors[92]. In addition, a phase II study evaluating the combination of the dual HER2/neu and EGFR tyrosine kinase lapatinib and gemcitabine in an unselected population, was closed due to a futility analysis[93].
Disappointing results were also observed in a large phase III trial comprising patients with metastatic or locally advanced pancreatic cancer who were randomly assigned to receive gemcitabine and cetuximab or gemcitabine monotherapy. No difference was detected for OS, response rate or PFS between the two groups. The population was not selected according to a biomarker, but EGFR expression was evaluated on 595 patients and detected in 90%: the EGFR positive patients showed no clinical benefit either[94].
Despite this failure, a two-stage study of PEGPH20 and cetuximab in patients with pancreatic adenocarcinoma prior to surgical resection is currently ongoing[95]. Moreover, a randomized phase II trial is currently recruiting patients undergoing treatment with gemcitabine monotherapy and gemcitabine plus afatinib, which is an oral EGFR1 and HER-2/HER-4 inhibitor. Of note, a translational project is included in the study in order to select patients who can benefit from the combination treatment[96].
The most known driver mutation in the progression of pancreatic cancer is mutated KRAS, which is present in up 85% of the patients. New molecules and therapeutic strategies to effectively inhibit KRAS are under investigation, but up to now no agent has successfully targeted KRAS or KRAS downstream pathways, such as mitogen-activated protein kinase kinase (MEK or MAPK/ERK kinase) or mTOR.
For instance, the MEK1/2 inhibitor CI-1040 has been evaluated in a phase II study including 15 pancreatic cancer patients. This drug demonstrated insufficient antitumor activity to warrant further evaluation[97]. Selumetinib has been evaluated in a phase II study comparing this MEK inhibitor in monotherapy vs capecitabine in the second-line setting, after a gemcitabine-based regimen. This trial showed a good safety profile, but no difference in OS emerged between the two arms[98]. MEK inhibitors have also been also investigated in combination with chemotherapy: the combination of trametinib and gemcitabine vs placebo and gemcitabine in the first-line setting. This trial did not show any significant difference in outcome and no difference was observed also in KRAS mutation-positive patients[99]. Similarly, the combination of pimasertib and gemcitabine did not result in any advantage in the clinical outcome vs gemcitabine and placebo[100]. A recent preclinical study showed that pimasertib reduced ribonucleotide reductase subunit 1 protein, which is a target of gemcitabine[101]. However, this protein was not evaluated in patients’ specimens, while KRAS mutational status did not influence the results. Conversely, in a randomized phase II trial evaluating refametinib and gemcitabine combination vs placebo, a trend toward a significantly longer OS, PFS and better ORR was observed in the subgroup of patients with KRAS wild type profile[102].
Feedback mechanisms triggered by MEK inhibitors can activate the EGFR and PI3K oncogenic pathways. This prompted the investigation of specific combination strategies[103], but the combination of EGFR and MEK inhibitors showed modest antitumor activity in previously treated pancreatic cancer patients. In particular, a phase II study combining erlotinib and selumetinib showed no objective response, a PFS of 1.9 mo and an OS of 7.3 mo. Interestingly, patients with an epithelial phenotype (i.e., with high level of E-cadherin expression) seemed to be more sensitive to the treatment, suggesting that further translational studies could identify subgroups of patients more likely to benefit from this treatment[104]. However, these combinatorial approaches can be limited by increased toxicity. Indeed, a phase I study of trametinib combined with mTOR inhibitor everolimus showed promising partial response and stable disease rates, of 7 and in 31% of cases, respectively, in the 21 pancreatic cancer patients enrolled in the trial. Unfortunately, the occurrence of severe treatment-related adverse events did not allow identifying a dose for a following phase II trial[105].
The overexpression of the tyrosine kinase receptor c-Met and its ligand, HGF, have been associated with cellular proliferation and survival in different tumor types[106]. In pancreatic cancer c-Met expression has been correlated to TNM stage, poor tumor differentiation, increased abnormal angiogenesis and shorter OS [107].
This receptor has been identified as a marker of pancreatic cancer stem cells (CSCs), which play a pivotal role in metastatic behaviour, and intrinsic chemoresistance[108]. Moreover, c-Met has been associated to the mesenchymal support network and EMT-like changes that characterize the cells with acquired resistance to gemcitabine[109]. The HGF-c-Met pathway has also been identified as a possible mediator of the neoangiogenic effects of cancer-associated human pancreatic stellate cells[110]. Furthermore HGF increases the production of VEGF by stromal cells and interacts with VEGF to support endothelial cells proliferation[111].
Recent preclinical studies showed the ability of the c-Met inhibitor crizotinib to specifically target CSC-like subpopulations and synergistically interact with gemcitabine, while cabozantinib slowed tumor growth and reduced the population of CSCs increasing the efficacy of gemcitabine even in high-resistant cells[112,113]. However, a more recent study on the inhibition of HGF using the neutralizing antibody AMG102 showed that this therapeutic strategy was more effective than gemcitabine in inhibiting tumor metastasis, but this effect was lost when combined with chemotherapy. These data suggest that gemcitabine selects a subpopulation of cells with CSCs and EMT features[114].
Several clinical trials on the combination of cabozantinib and gemcitabine are currently ongoing in advanced cancers, including pancreatic cancer (NCT01744652, NCT01548144, NCT01531361, NCT01999972, NCT01663272) and the results of a recently completed randomized phase II trial of tivantinib vs gemcitabine in patients with advanced pancreatic cancer are awaited[115].
A recent study showed that targeting the Janus-activated kinase-2 (JAK2) signalling pathway in pancreatic cancer inhibits the proliferation of pancreatic cancer cells. JAK2 can indeed activate the transcriptional factor signal transducer and activator of transcription 3 (STAT3), which is leading one of the signalling mechanisms involved in pancreatic carcinogenesis; as well as to angiogenesis, cell proliferation and metastasis in various malignancies[116]. Furthermore, JAK-STAT pathway is a mediator of multiple inflammatory responses both in the tumor and in the host tissues, involved in the cachexia response[117].
The potent JAK-1 and JAK-2 inhibitor ruxolitinib was tested in a randomized phase II study in patients who underwent failure to a gemcitabine-containing first-line treatment, who were randomized to receive ruxolitinib in combination with capecitabine vs capecitabine and placebo. In the whole population of 127 patients no difference in OS or PFS was detected between the two arms, but in a pre-specified subgroup analysis it was shown that patients with higher levels of C-reactive protein (> 13 mg/L) had an HR for OS of 0.47 while the HR for OS in patients with levels lower or equal to 13 mg/L was 0.89. Remarkably, additional post-hoc analyses which categorized patients according to mGPS (Glasgow Prognostic Score) status (based on C-reactive protein and albumin levels), showed a meaningful separation in OS between the ruxolitinib and capecitabine groups with increasing mGPS[118].
Based on these results, two phase III studies are ongoing to investigate the activity of ruxolitinib and capecitabine after failure of a first-line treatment, in patients with metastatic pancreatic cancer and an mGPS status of 1 or 2[119,120].
Since pancreatic cancer is such a dismal disease, any biomarker that can help to better stratify patients might have crucial clinical applications. Moreover, considering that the therapeutic options that have been made recently available for metastatic pancreatic cancer patients provide almost identical disease control and similar survival, novel biomarkers are required to aid treatment decisions.
High impact bench-to-bedside research on hundreds of patient samples improved prognostic capabilities in several tumor types, such as breast cancer[121]. Similar studies are more difficult to perform in pancreatic cancer, which is less common disease, characterized by dense stromal reaction and very small amounts of tumor tissue available.
The discovery of miRNAs has unraveled new mechanisms for regulation of gene expression and has provided new directions for the quest of cancer biomarkers[122]. MiRNAs are potentially ideal biomarkers, as they are stable molecules, tumor and tissue specific, and can be detected with different techniques in a very small amount of tissue.
The pivotal regulatory role of each miRNA in controlling expression of multiple gene transcripts offers a unique opportunity of identifying critical miRNAs as informative biomarkers for detection, diagnosis and prognosis of tumors that result from deregulation of multiple genes. Expression profiling data have created diagnostic and prognostic signatures for a variety of tumor types[123]. Furthermore, selected miRNAs may influence response to chemotherapy[124].
Although the PDAC miRNome has been extensively profiled[125], it remains unclear which differentially expressed miRNAs are most important in the clinical outcome. In particular, only a few studies evaluated the role of candidate miRNAs to predict the sensitivity/resistance to the drugs of the FOLFIRINOX and gemcitabine/nab-paclitaxel regimens.
The epithelial and stromal expression of miR-21 was assessed by in situ hybridization (ISH) in 229 patients from a phase III randomized trial comparing 5-FU to gemcitabine before and after 5-FU-based chemoradiation therapy (RTOG 9704). Remarkably, higher levels of miR-21 expression in CAFs correlated with shorter OS in the patients treated with 5-FU, but not gemcitabine[126]. These data are in contrast with a previous study assessing miR-21 expression by PCR in two independent cohorts of patients, treated with various gemcitabine or 5-FU containing adjuvant regimens, suggesting that miR-21 expression can affect outcome of both gemcitabine and 5-FU-based treatment[127]. Similarly, PCR data on laser-microdissected specimens demonstrated a correlation between a high expression of miR-21 with worse outcome after gemcitabine treatment in both radically-resected and metastatic patients, as well as in a cohort of pancreatic cancer arising from intraductal papillary mucinous neoplasms of the pancreas[128,129]. These results might be explained by several effects of miR-21 overexpression on preclinical models of pancreatic cancer, including inhibition of apoptosis and induction of cell proliferation and invasion, as well as chemoresistance to both gemcitabine and 5-FU[128,130]. More recently, other two miRNAs (miR-23a, and miR-27a) were added to miR-21 to identify a combination of miRNA that acted as cooperative repressors of a network of tumor suppressor genes[131]. In 91 PDAC samples from gemcitabine-treated radically resected patients, high levels of this triple miRNA combination were associated with shorter OS. Thus, the role of miR-21 as prognostic or predictive biomarker for 5-FU and/or gemcitabine is still under debate and data from a study on larger cohorts of patients, using validated methods, are urgently awaited.
Other potential biomarkers related to miRNA effects in patients treated with 5-FU as well as to the other drugs of the FOLFIRINOX regimens have been investigated in metastatic patients affected by different tumor types, but not in pancreas. In particular, a pharmacogenetic study on 18 polymorphisms in miRNA-containing genomic regions (primary and precursor miRNA) and in genes related to miRNA biogenesis in 61 patients with metastatic colorectal cancer treated with 5-FU and irinotecan. The polymorphism rs7372209 in pri-miR26a-1 was associated with a higher response and longer OS, while the polymorphism rs1834306, located in the pri-miR-100 gene, correlated with a longer PFS[132]. A more extensive study profiled 742 miRNAs in laser-capture microdissected samples from 26 patients receiving 5-FU or capecitabine combined with oxaliplatin for metastatic colorectal cancer. This study suggested that overexpression of miR-625-3p, miR-181b and miR-27b was associated with lower response rate. In a validation cohort of 94 patients treated with capecitabine and oxaliplatin, high expression of miR-625-3p was confirmed to be associated with poor response rate[133]. However, different results emerged from a study evaluating 754 miRNAs in a screening (n = 212) and validation (n = 121) cohort of metastatic colorectal cancer patients treated with the first line combination of capecitabine, oxaliplatin and the VEGF inhibitor bevacizumab[134]. Higher miR-664-3p expression and lower miR-455-5p expression were predictive of longer OS, while higher expression of miR-196b-5p and miR-592 predicted improved OS regardless of bevacizumab treatment in a control cohort of 127 patients.
No data are yet available on miRNA affecting nab-paclitaxel, but several miRNAs have been associated to resistance to paclitaxel, which is currently used for treatment of various cancers. A study in 82 patients with metastatic or recurrent gastric cancer receiving first-line chemotherapy with fluoropyrimidine combined with paclitaxel or oxaliplatin showed that patients with miRNA27a overexpression had a significantly shorter OS[135]. More recently, the Nanostring miRNA array was used to evaluate tumor tissues from 115 of 823 patients enrolled in the Intergroup trial E2603, which randomized metastatic melanoma patients to carboplatin and paclitaxel with or without sorafenib[136]. High levels of miR-659-3p expression were correlated to responsive compared to stable disease, supporting future studies on this potential predictive biomarker in different tumor types.
Several preclinical studies suggest the role of many other miRNAs in the activity of the chemotherapeutics drugs used for the first-line treatment of metastatic pancreatic cancer, as illustrated in the Table 3. However, as with previous studies on gene profiling, most miRNAs correlated to chemoresistance are not overlapping and no conclusive evidence has yet been obtained about their clinical use. These controversial data might be explai00pned by the different samples (frozen vs paraffin-embedded, micro- vs non-microdissected), experimental platforms (quantitative PCR vs miRNA array or ISH), stage, and regimens, as well as small cohort size, and lack of adequate statistical analyses. Trials in larger cohorts, with new, standardized analytical methodologies, including next-generation sequencing, are warranted.
| Drug | miRNA | Expression/polymorphism | Tumor type | Ref. |
| 5-FU | miR-21 | Overexpression | Pancreatic cancer | Donahue et al[126], J Surg Oncol 2014 |
| 5-FU and irinotecan | pri-miR26a-1 | rs7372209 polymorphism | Colorectal cancer | Boni et al[132], Pharmacogenomics J 2011 |
| 5-FU and oxaliplatin | miR-106a, miR-484, miR-130b | Overexpression | Colorectal cancer | Kjersem et al[143], Mol Oncol 2014 |
| 5-FU, paclitaxel and oxaliplatin | miR-27a | Overexpression | Gastric cancer | Huang et al[135], J Cell Biochem 2014 |
| 5-FU, capecitabine and oxaliplatin | miR-625-3p, miR-181b, miR-27b | Overexpression | Colorectal cancer | Rasmussen et al[133], Mol Oncol 2013 |
| Irinotecan and cetuximab | miR-345 | Overexpression | Colorectal cancer | Schou et al[144], PLoS One 2014 |
| Oxaliplatin | miR-203 | Overexpression | Colorectal cancer | Zhou et al[145], Mol Oncol 2014 |
| Carboplatin and paclitaxel ± sorafenib | miR-659-3p | Downregulation | Melanoma | Villaruz et al[136], Clin Epigenetics 2015 |
| Paclitaxel | miR-200c | Downregulation | Ovarian and endometrial cancer | Cochrane et al[146], Mol Cancer Ther 2009 |
| Paclitaxel | miR-145 | Downregulation | Ovarian cancer | Zhu et al[147], Int J Cancer 2014 |
| Paclitaxel | miR-17-5p | Downregulation | Lung cancer | Aggarwal et al[148], Planta Med 2008 |
| Gemcitabine | miR-21 | Overexpression | Pancreatic cancer | Hwang et al[127], PLoS One 2010 |
| Giovannetti et al[128], Cancer Res 2010 | ||||
| Caponi et al[129], Ann Oncol 2013 | ||||
| Gemcitabine | miR-21, miR-23a, miR-27a | Overexpression | Pancreatic cancer | Frampton et al[131], Gastroenterology 2014 |
Several progresses have been made in the chemotherapeutic treatment of metastatic pancreatic cancer in these last few years, but these improvements are still mostly incremental, without major impact on the grim prognosis of these patients.
Despite the substantially improved knowledge about basic pancreatic cancer biology and the recruitment of hundreds of patients in many clinical trials, novel targeted therapies for angiogenic targets and tyrosine kinase have shown poor results. However, most of these trials did not evaluate predictive markers, which are essential to guide patient selection with biological agents. Moreover, most translational studies on candidate biomarkers, such as hENT1, TS and SPARC, showed controversial results. The major limitations of these studies should be overcome by prospective clinical trials, using standardized analytical methodologies, in which a direct comparison is performed between patient treatments selected on the basis of standard criteria vs treatment selection suggested by tumor characteristics.
Other limitations arise from the intra-tumor heterogeneity and other complex epigenetic factors, such as miRNA, which might foster tumor adaptation and therapeutic failure. Therefore, studies on miRNA may clarify the role of several signaling pathways in drug resistance and identify stronger biomarkers or new potential targets.
Moreover, to evaluate the heterogeneity and possible evolution of cancer cells the future clinical trials should include multiple and repeated biopsies of the single tumor, and/or novel liquid biopsies. Most recent studies have showed promising results for liquid biopsy-based molecular diagnostics in patients with several types of cancer, including pancreatic cancer[137,138]. In particular, by investigating circulating metabolites in plasma from 4 cohorts of pancreatic cancer patients and matching controls, elevated plasma levels of branched-chain amino acids (BCAAs) have been associated with a greater than two-fold increased risk of pancreatic carcinogenesis. Remarkably, plasma BCAAs were elevated in mice with early-stage pancreatic cancers driven by mutant Kras expression but not in mice with KRAS-driven tumors in other tissues, suggesting that increased whole-body protein breakdown is a specific event that accompanies early stage development of pancreatic cancer[138].
Early detection of a druggable biomarker in the natural history of the single patient can indeed be crucial, considering the rapidly progressing disease and the sudden deterioration of general conditions that commonly characterize the subset of pancreatic cancer patients. The individualized molecular pancreatic cancer trial is a good example of a trial aimed at improving outcome of patients with recurrence or metastases pancreatic cancer using molecular analysis on tumor specimens to guide treatment decision. This trial was designed as a randomized phase II trial in 2010, before the “FOLFIRINOX/nab-paclitaxel-gemcitabine era”. Therefore, the patients were randomized to receive chemotherapy with gemcitabine or personalized treatment depending on the genetic biomarker expressed: patients with amplification of HER-2, absence of KRAS mutation or patients with mutation in DNA damage repair genes (BRCA1 and 2-ATM-PALB2) were eligible for personalized therapy. This trial showed the feasibility of collecting and analyzing samples for candidate molecular targets in real-time and prompt future translational studies with similar design[139,140].
Many ongoing trials are evaluating the combination of new agents within both “FOLFIRINOX-based” and “nab-paclitaxel-based” therapies, as extensively reviewed by Vaccaro and collaborators[141]. An interesting approach is the combination with immunotherapy, and a recent study phase Ib study showed promising results for FOLFIRINOX in combination with a CCR2 inhibitor PF-04136309, which will be further investigated in a phase II randomized trial. The rationale of this study is based on the fact that the CCL2-CCR2 chemokine axis is involved in recruiting tumor-associated macrophages and in the construction of the immunosuppressive microenvironment of pancreatic cancer[142]. Hopefully, within these trials, as well as in other ongoing and future clinical protocols, the availability of new technologies for appropriate parallel translational studies will identify solid predictive biomarkers that in turn can be used to select the most appropriate pharmacological agent for personalization of the treatment (i.e., precision medicine). For this goal both the careful collection of tissue samples, and the coordinated multidisciplinary work of surgeons, radiologists, gastroenterologists, oncologists and scientists, will be crucial to evaluate the best experimental therapeutic options for each given patient, and should therefore enter as soon as possible in the clinical practice.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Italy
Peer-review report classification
Grade A (Excellent): A, A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Chen Q, Lonardo E, Neri V S- Editor: Yu J L- Editor: A E- Editor: Ma S
| 1. | Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA Cancer J Clin. 2016;66:7-30. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12135] [Cited by in F6Publishing: 12698] [Article Influence: 1587.3] [Reference Citation Analysis (2)] |
| 2. | Stromnes IM, Schmitt TM, Hulbert A, Brockenbrough JS, Nguyen HN, Cuevas C, Dotson AM, Tan X, Hotes JL, Greenberg PD. T Cells Engineered against a Native Antigen Can Surmount Immunologic and Physical Barriers to Treat Pancreatic Ductal Adenocarcinoma. Cancer Cell. 2015;28:638-652. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 134] [Cited by in F6Publishing: 132] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 3. | Beatty GL, Torigian DA, Chiorean EG, Saboury B, Brothers A, Alavi A, Troxel AB, Sun W, Teitelbaum UR, Vonderheide RH. A phase I study of an agonist CD40 monoclonal antibody (CP-870,893) in combination with gemcitabine in patients with advanced pancreatic ductal adenocarcinoma. Clin Cancer Res. 2013;19:6286-6295. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 306] [Cited by in F6Publishing: 334] [Article Influence: 30.4] [Reference Citation Analysis (0)] |
| 4. | Laheru D, Lutz E, Burke J, Biedrzycki B, Solt S, Onners B, Tartakovsky I, Nemunaitis J, Le D, Sugar E. Allogeneic granulocyte macrophage colony-stimulating factor-secreting tumor immunotherapy alone or in sequence with cyclophosphamide for metastatic pancreatic cancer: a pilot study of safety, feasibility, and immune activation. Clin Cancer Res. 2008;14:1455-1463. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 250] [Cited by in F6Publishing: 252] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 5. | Le DT, Wang-Gillam A, Picozzi V, Greten TF, Crocenzi T, Springett G, Morse M, Zeh H, Cohen D, Fine RL. Safety and survival with GVAX pancreas prime and Listeria Monocytogenes-expressing mesothelin (CRS-207) boost vaccines for metastatic pancreatic cancer. J Clin Oncol. 2015;33:1325-1333. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 386] [Cited by in F6Publishing: 409] [Article Influence: 45.4] [Reference Citation Analysis (0)] |
| 6. | Burris HA, Moore MJ, Andersen J, Green MR, Rothenberg ML, Modiano MR, Cripps MC, Portenoy RK, Storniolo AM, Tarassoff P. Improvements in survival and clinical benefit with gemcitabine as first-line therapy for patients with advanced pancreas cancer: a randomized trial. J Clin Oncol. 1997;15:2403-2413. [PubMed] [Cited in This Article: ] |
| 7. | Cunningham D, Chau I, Stocken DD, Valle JW, Smith D, Steward W, Harper PG, Dunn J, Tudur-Smith C, West J. Phase III randomized comparison of gemcitabine versus gemcitabine plus capecitabine in patients with advanced pancreatic cancer. J Clin Oncol. 2009;27:5513-5518. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 534] [Cited by in F6Publishing: 550] [Article Influence: 36.7] [Reference Citation Analysis (0)] |
| 8. | Heinemann V, Quietzsch D, Gieseler F, Gonnermann M, Schönekäs H, Rost A, Neuhaus H, Haag C, Clemens M, Heinrich B. Randomized phase III trial of gemcitabine plus cisplatin compared with gemcitabine alone in advanced pancreatic cancer. J Clin Oncol. 2006;24:3946-3952. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 464] [Cited by in F6Publishing: 482] [Article Influence: 26.8] [Reference Citation Analysis (0)] |
| 9. | Sun C, Ansari D, Andersson R, Wu DQ. Does gemcitabine-based combination therapy improve the prognosis of unresectable pancreatic cancer? World J Gastroenterol. 2012;18:4944-4958. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 56] [Cited by in F6Publishing: 53] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 10. | Moore MJ, Goldstein D, Hamm J, Figer A, Hecht JR, Gallinger S, Au HJ, Murawa P, Walde D, Wolff RA. Erlotinib plus gemcitabine compared with gemcitabine alone in patients with advanced pancreatic cancer: a phase III trial of the National Cancer Institute of Canada Clinical Trials Group. J Clin Oncol. 2007;25:1960-1966. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2755] [Cited by in F6Publishing: 2667] [Article Influence: 156.9] [Reference Citation Analysis (0)] |
| 11. | Van Cutsem E, Li CP, Nowara E, Aprile G, Moore M, Federowicz I, Van Laethem JL, Hsu C, Tham CK, Stemmer SM. Dose escalation to rash for erlotinib plus gemcitabine for metastatic pancreatic cancer: the phase II RACHEL study. Br J Cancer. 2014;111:2067-2075. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 37] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 12. | Geis-Gerstorfer J, Eckhardt M, Lin W, Weber H. [Finishing of cast titanium for crowns and bridges]. Dtsch Zahnarztl Z. 1989;44:882-884. [PubMed] [Cited in This Article: ] |
| 13. | Elnaggar M, Giovannetti E, Peters GJ. Molecular targets of gemcitabine action: rationale for development of novel drugs and drug combinations. Curr Pharm Des. 2012;18:2811-2829. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 40] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 14. | van Bree C, Castro Kreder N, Loves WJ, Franken NA, Peters GJ, Haveman J. Sensitivity to ionizing radiation and chemotherapeutic agents in gemcitabine-resistant human tumor cell lines. Int J Radiat Oncol Biol Phys. 2002;54:237-244. [PubMed] [Cited in This Article: ] |
| 15. | Ohhashi S, Ohuchida K, Mizumoto K, Fujita H, Egami T, Yu J, Toma H, Sadatomi S, Nagai E, Tanaka M. Down-regulation of deoxycytidine kinase enhances acquired resistance to gemcitabine in pancreatic cancer. Anticancer Res. 2008;28:2205-2212. [PubMed] [Cited in This Article: ] |
| 16. | Kroep JR, Loves WJ, van der Wilt CL, Alvarez E, Talianidis I, Boven E, Braakhuis BJ, van Groeningen CJ, Pinedo HM, Peters GJ. Pretreatment deoxycytidine kinase levels predict in vivo gemcitabine sensitivity. Mol Cancer Ther. 2002;1:371-376. [PubMed] [Cited in This Article: ] |
| 17. | Al-Madhoun AS, van der Wilt CL, Loves WJ, Padron JM, Eriksson S, Talianidis I, Peters GJ. Detection of an alternatively spliced form of deoxycytidine kinase mRNA in the 2’-2’-difluorodeoxycytidine (gemcitabine)-resistant human ovarian cancer cell line AG6000. Biochem Pharmacol. 2004;68:601-609. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 18. | Sebastiani V, Ricci F, Rubio-Viqueira B, Kulesza P, Yeo CJ, Hidalgo M, Klein A, Laheru D, Iacobuzio-Donahue CA. Immunohistochemical and genetic evaluation of deoxycytidine kinase in pancreatic cancer: relationship to molecular mechanisms of gemcitabine resistance and survival. Clin Cancer Res. 2006;12:2492-2497. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 115] [Cited by in F6Publishing: 125] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 19. | Abbruzzese JL, Grunewald R, Weeks EA, Gravel D, Adams T, Nowak B, Mineishi S, Tarassoff P, Satterlee W, Raber MN. A phase I clinical, plasma, and cellular pharmacology study of gemcitabine. J Clin Oncol. 1991;9:491-498. [PubMed] [Cited in This Article: ] |
| 20. | Grunewald R, Abbruzzese JL, Tarassoff P, Plunkett W. Saturation of 2’,2’-difluorodeoxycytidine 5’-triphosphate accumulation by mononuclear cells during a phase I trial of gemcitabine. Cancer Chemother Pharmacol. 1991;27:258-262. [PubMed] [Cited in This Article: ] |
| 21. | Pollera CF, Ceribelli A, Crecco M, Oliva C, Calabresi F. Prolonged infusion gemcitabine: a clinical phase I study at low- (300 mg/m2) and high-dose (875 mg/m2) levels. Invest New Drugs. 1997;15:115-121. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 48] [Cited by in F6Publishing: 51] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 22. | Grunewald R, Kantarjian H, Du M, Faucher K, Tarassoff P, Plunkett W. Gemcitabine in leukemia: a phase I clinical, plasma, and cellular pharmacology study. J Clin Oncol. 1992;10:406-413. [PubMed] [Cited in This Article: ] |
| 23. | Tempero M, Plunkett W, Ruiz Van Haperen V, Hainsworth J, Hochster H, Lenzi R, Abbruzzese J. Randomized phase II comparison of dose-intense gemcitabine: thirty-minute infusion and fixed dose rate infusion in patients with pancreatic adenocarcinoma. J Clin Oncol. 2003;21:3402-3408. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 388] [Cited by in F6Publishing: 410] [Article Influence: 19.5] [Reference Citation Analysis (0)] |
| 24. | Poplin E, Feng Y, Berlin J, Rothenberg ML, Hochster H, Mitchell E, Alberts S, O’Dwyer P, Haller D, Catalano P. Phase III, randomized study of gemcitabine and oxaliplatin versus gemcitabine (fixed-dose rate infusion) compared with gemcitabine (30-minute infusion) in patients with pancreatic carcinoma E6201: a trial of the Eastern Cooperative Oncology Group. J Clin Oncol. 2009;27:3778-3785. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 295] [Cited by in F6Publishing: 308] [Article Influence: 20.5] [Reference Citation Analysis (0)] |
| 25. | Spratlin J, Sangha R, Glubrecht D, Dabbagh L, Young JD, Dumontet C, Cass C, Lai R, Mackey JR. The absence of human equilibrative nucleoside transporter 1 is associated with reduced survival in patients with gemcitabine-treated pancreas adenocarcinoma. Clin Cancer Res. 2004;10:6956-6961. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 289] [Cited by in F6Publishing: 302] [Article Influence: 15.9] [Reference Citation Analysis (0)] |
| 26. | Giovannetti E, Del Tacca M, Mey V, Funel N, Nannizzi S, Ricci S, Orlandini C, Boggi U, Campani D, Del Chiaro M. Transcription analysis of human equilibrative nucleoside transporter-1 predicts survival in pancreas cancer patients treated with gemcitabine. Cancer Res. 2006;66:3928-3935. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 259] [Cited by in F6Publishing: 273] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 27. | Farrell JJ, Elsaleh H, Garcia M, Lai R, Ammar A, Regine WF, Abrams R, Benson AB, Macdonald J, Cass CE. Human equilibrative nucleoside transporter 1 levels predict response to gemcitabine in patients with pancreatic cancer. Gastroenterology. 2009;136:187-195. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 320] [Cited by in F6Publishing: 350] [Article Influence: 23.3] [Reference Citation Analysis (0)] |
| 28. | Greenhalf W, Ghaneh P, Neoptolemos JP, Palmer DH, Cox TF, Lamb RF, Garner E, Campbell F, Mackey JR, Costello E. Pancreatic cancer hENT1 expression and survival from gemcitabine in patients from the ESPAC-3 trial. J Natl Cancer Inst. 2014;106:djt347. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 199] [Cited by in F6Publishing: 198] [Article Influence: 19.8] [Reference Citation Analysis (0)] |
| 29. | Poplin E, Wasan H, Rolfe L, Raponi M, Ikdahl T, Bondarenko I, Davidenko I, Bondar V, Garin A, Boeck S. Randomized, multicenter, phase II study of CO-101 versus gemcitabine in patients with metastatic pancreatic ductal adenocarcinoma: including a prospective evaluation of the role of hENT1 in gemcitabine or CO-101 sensitivity. J Clin Oncol. 2013;31:4453-4461. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 117] [Cited by in F6Publishing: 132] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 30. | Sinn M, Riess H, Sinn BV, Stieler JM, Pelzer U, Striefler JK, Oettle H, Bahra M, Denkert C, Bläker H. Human equilibrative nucleoside transporter 1 expression analysed by the clone SP 120 rabbit antibody is not predictive in patients with pancreatic cancer treated with adjuvant gemcitabine - Results from the CONKO-001 trial. Eur J Cancer. 2015;51:1546-1554. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 29] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 31. | Wei CH, Gorgan TR, Elashoff DA, Hines OJ, Farrell JJ, Donahue TR. A meta-analysis of gemcitabine biomarkers in patients with pancreaticobiliary cancers. Pancreas. 2013;42:1303-1310. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 32] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 32. | Ychou M, Conroy T, Seitz JF, Gourgou S, Hua A, Mery-Mignard D, Kramar A. An open phase I study assessing the feasibility of the triple combination: oxaliplatin plus irinotecan plus leucovorin/ 5-fluorouracil every 2 weeks in patients with advanced solid tumors. Ann Oncol. 2003;14:481-489. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 70] [Cited by in F6Publishing: 74] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 33. | Conroy T, Paillot B, François E, Bugat R, Jacob JH, Stein U, Nasca S, Metges JP, Rixe O, Michel P. Irinotecan plus oxaliplatin and leucovorin-modulated fluorouracil in advanced pancreatic cancer--a Groupe Tumeurs Digestives of the Federation Nationale des Centres de Lutte Contre le Cancer study. J Clin Oncol. 2005;23:1228-1236. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 162] [Cited by in F6Publishing: 174] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 34. | Conroy T, Desseigne F, Ychou M, Bouché O, Guimbaud R, Bécouarn Y, Adenis A, Raoul JL, Gourgou-Bourgade S, de la Fouchardière C. FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. N Engl J Med. 2011;364:1817-1825. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4838] [Cited by in F6Publishing: 5099] [Article Influence: 392.2] [Reference Citation Analysis (1)] |
| 35. | Conroy T, Gavoille C, Samalin E, Ychou M, Ducreux M. The role of the FOLFIRINOX regimen for advanced pancreatic cancer. Curr Oncol Rep. 2013;15:182-189. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 64] [Cited by in F6Publishing: 63] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 36. | Mahaseth H, Brutcher E, Kauh J, Hawk N, Kim S, Chen Z, Kooby DA, Maithel SK, Landry J, El-Rayes BF. Modified FOLFIRINOX regimen with improved safety and maintained efficacy in pancreatic adenocarcinoma. Pancreas. 2013;42:1311-1315. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 145] [Cited by in F6Publishing: 148] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 37. | Lowery MA, Yu KH, Adel NG, Apollo AJ, Boyar MS, Caron P, Ilson D, Segal NH, Janjigian YY, Reidy DL. Activity of front-line FOLFIRINOX (FFX) in stage III/IV pancreatic adenocarcinoma (PC) at Memorial Sloan-Kettering Cancer Center (MSKCC). J Clin Oncol. 2012;30:4057. [Cited in This Article: ] |
| 38. | Falcone A, Masi G, Allegrini G, Danesi R, Pfanner E, Brunetti IM, Di Paolo A, Cupini S, Del Tacca M, Conte P. Biweekly chemotherapy with oxaliplatin, irinotecan, infusional Fluorouracil, and leucovorin: a pilot study in patients with metastatic colorectal cancer. J Clin Oncol. 2002;20:4006-4014. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 119] [Cited by in F6Publishing: 127] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 39. | Masi G, Allegrini G, Cupini S, Marcucci L, Cerri E, Brunetti I, Fontana E, Ricci S, Andreuccetti M, Falcone A. First-line treatment of metastatic colorectal cancer with irinotecan, oxaliplatin and 5-fluorouracil/leucovorin (FOLFOXIRI): results of a phase II study with a simplified biweekly schedule. Ann Oncol. 2004;15:1766-1772. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 81] [Cited by in F6Publishing: 88] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 40. | Falcone A, Ricci S, Brunetti I, Pfanner E, Allegrini G, Barbara C, Crinò L, Benedetti G, Evangelista W, Fanchini L. Phase III trial of infusional fluorouracil, leucovorin, oxaliplatin, and irinotecan (FOLFOXIRI) compared with infusional fluorouracil, leucovorin, and irinotecan (FOLFIRI) as first-line treatment for metastatic colorectal cancer: the Gruppo Oncologico Nord Ovest. J Clin Oncol. 2007;25:1670-1676. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 830] [Cited by in F6Publishing: 838] [Article Influence: 49.3] [Reference Citation Analysis (0)] |
| 41. | Vivaldi C, Caparello C, Musettini G, Pasquini G, Catanese S, Fornaro L, Lencioni M, Falcone A, Vasile E. First-line treatment with FOLFOXIRI for advanced pancreatic cancer in clinical practice: Patients’ outcome and analysis of prognostic factors. Int J Cancer. 2016;139:938-945. [PubMed] [Cited in This Article: ] |
| 42. | Wang WB, Yang Y, Zhao YP, Zhang TP, Liao Q, Shu H. Recent studies of 5-fluorouracil resistance in pancreatic cancer. World J Gastroenterol. 2014;20:15682-15690. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 62] [Cited by in F6Publishing: 63] [Article Influence: 6.3] [Reference Citation Analysis (1)] |
| 43. | Kurata N, Fujita H, Ohuchida K, Mizumoto K, Mahawithitwong P, Sakai H, Onimaru M, Manabe T, Ohtsuka T, Tanaka M. Predicting the chemosensitivity of pancreatic cancer cells by quantifying the expression levels of genes associated with the metabolism of gemcitabine and 5-fluorouracil. Int J Oncol. 2011;39:473-482. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 44. | Nakayama S, Takeda S, Kawase Y, Inoue S, Kaneko T, Nakao A. Clinical significance of dihydropyrimidine dehydrogenase in adjuvant 5-fluorouracil liver perfusion chemotherapy for pancreatic cancer. Ann Surg. 2004;240:840-844. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 26] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 45. | Takamura M, Nio Y, Yamasawa K, Dong M, Yamaguchi K, Itakura M. Implication of thymidylate synthase in the outcome of patients with invasive ductal carcinoma of the pancreas and efficacy of adjuvant chemotherapy using 5-fluorouracil or its derivatives. Anticancer Drugs. 2002;13:75-85. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 33] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 46. | Chaney SG, Sancar A. DNA repair: enzymatic mechanisms and relevance to drug response. J Natl Cancer Inst. 1996;88:1346-1360. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 191] [Cited by in F6Publishing: 197] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 47. | Fuereder T, Stift J, Kuehrer I, Stranzl N, Hoeflmayer D, Kornek G, Scheithauer W. Response to GEMOX plus erlotinib in pancreatic cancer is associated with ERCC1 overexpression. Eur J Clin Invest. 2014;44:958-964. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 48. | Friboulet L, Olaussen KA, Pignon JP, Shepherd FA, Tsao MS, Graziano S, Kratzke R, Douillard JY, Seymour L, Pirker R. ERCC1 isoform expression and DNA repair in non-small-cell lung cancer. N Engl J Med. 2013;368:1101-1110. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 268] [Cited by in F6Publishing: 292] [Article Influence: 26.5] [Reference Citation Analysis (0)] |
| 49. | Giovannetti E, Pacetti P, Reni M, Leon LG, Mambrini A, Vasile E, Ghidini M, Funel N, Lucchesi M, Cereda S. Association between DNA-repair polymorphisms and survival in pancreatic cancer patients treated with combination chemotherapy. Pharmacogenomics. 2011;12:1641-1652. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 35] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 50. | Avan A, Pacetti P, Reni M, Milella M, Vasile E, Mambrini A, Vaccaro V, Caponi S, Cereda S, Peters GJ. Prognostic factors in gemcitabine-cisplatin polychemotherapy regimens in pancreatic cancer: XPD-Lys751Gln polymorphism strikes back. Int J Cancer. 2013;133:1016-1022. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 23] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 51. | Takeda S, Shimazoe T, Sato K, Sugimoto Y, Tsuruo T, Kono A. Differential expression of DNA topoisomerase I gene between CPT-11 acquired- and native-resistant human pancreatic tumor cell lines: detected by RNA/PCR-based quantitation assay. Biochem Biophys Res Commun. 1992;184:618-625. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 26] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 52. | Capello M, Lee M, Wang H, Babel I, Katz MH, Fleming JB, Maitra A, Wang H, Tian W, Taguchi A. Carboxylesterase 2 as a Determinant of Response to Irinotecan and Neoadjuvant FOLFIRINOX Therapy in Pancreatic Ductal Adenocarcinoma. J Natl Cancer Inst. 2015;107:132. [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 61] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 53. | Grunnet M, Calatayud D, Schultz NA, Hasselby JP, Mau-Sørensen M, Brünner N, Stenvang J. TOP1 gene copy numbers are increased in cancers of the bile duct and pancreas. Scand J Gastroenterol. 2015;50:485-494. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 54. | Yardley DA. nab-Paclitaxel mechanisms of action and delivery. J Control Release. 2013;170:365-372. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 232] [Cited by in F6Publishing: 297] [Article Influence: 27.0] [Reference Citation Analysis (0)] |
| 55. | Desai N, Trieu V, Damascelli B, Soon-Shiong P. SPARC Expression Correlates with Tumor Response to Albumin-Bound Paclitaxel in Head and Neck Cancer Patients. Transl Oncol. 2009;2:59-64. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 272] [Cited by in F6Publishing: 285] [Article Influence: 21.9] [Reference Citation Analysis (0)] |
| 56. | Olive KP, Jacobetz MA, Davidson CJ, Gopinathan A, McIntyre D, Honess D, Madhu B, Goldgraben MA, Caldwell ME, Allard D. Inhibition of Hedgehog signaling enhances delivery of chemotherapy in a mouse model of pancreatic cancer. Science. 2009;324:1457-1461. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2272] [Cited by in F6Publishing: 2392] [Article Influence: 159.5] [Reference Citation Analysis (0)] |
| 57. | Provenzano PP, Cuevas C, Chang AE, Goel VK, Von Hoff DD, Hingorani SR. Enzymatic targeting of the stroma ablates physical barriers to treatment of pancreatic ductal adenocarcinoma. Cancer Cell. 2012;21:418-429. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1408] [Cited by in F6Publishing: 1468] [Article Influence: 122.3] [Reference Citation Analysis (0)] |
| 58. | Frese KK, Neesse A, Cook N, Bapiro TE, Lolkema MP, Jodrell DI, Tuveson DA. nab-Paclitaxel potentiates gemcitabine activity by reducing cytidine deaminase levels in a mouse model of pancreatic cancer. Cancer Discov. 2012;2:260-269. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 312] [Cited by in F6Publishing: 328] [Article Influence: 27.3] [Reference Citation Analysis (0)] |
| 59. | Von Hoff DD, Ramanathan RK, Borad MJ, Laheru DA, Smith LS, Wood TE, Korn RL, Desai N, Trieu V, Iglesias JL. Gemcitabine plus nab-paclitaxel is an active regimen in patients with advanced pancreatic cancer: a phase I/II trial. J Clin Oncol. 2011;29:4548-4554. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 755] [Cited by in F6Publishing: 835] [Article Influence: 64.2] [Reference Citation Analysis (2)] |
| 60. | Von Hoff DD, Ervin T, Arena FP, Chiorean EG, Infante J, Moore M, Seay T, Tjulandin SA, Ma WW, Saleh MN. Increased survival in pancreatic cancer with nab-paclitaxel plus gemcitabine. N Engl J Med. 2013;369:1691-1703. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4035] [Cited by in F6Publishing: 4330] [Article Influence: 393.6] [Reference Citation Analysis (0)] |
| 61. | Hidalgo M, Plaza C, Musteanu M, Illei P, Brachmann CB, Heise C, Pierce D, Lopez-Casas PP, Menendez C, Tabernero J. SPARC Expression Did Not Predict Efficacy of nab-Paclitaxel plus Gemcitabine or Gemcitabine Alone for Metastatic Pancreatic Cancer in an Exploratory Analysis of the Phase III MPACT Trial. Clin Cancer Res. 2015;21:4811-4818. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 97] [Cited by in F6Publishing: 106] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 62. | Gore J, Korc M. Pancreatic cancer stroma: friend or foe? Cancer Cell. 2014;25:711-712. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 143] [Cited by in F6Publishing: 149] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 63. | Sève P, Mackey J, Isaac S, Trédan O, Souquet PJ, Pérol M, Lai R, Voloch A, Dumontet C. Class III beta-tubulin expression in tumor cells predicts response and outcome in patients with non-small cell lung cancer receiving paclitaxel. Mol Cancer Ther. 2005;4:2001-2007. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 186] [Cited by in F6Publishing: 198] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 64. | Hwang JE, Hong JY, Kim K, Kim SH, Choi WY, Kim MJ, Jung SH, Shim HJ, Bae WK, Hwang EC. Class III β-tubulin is a predictive marker for taxane-based chemotherapy in recurrent and metastatic gastric cancer. BMC Cancer. 2013;13:431. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 40] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 65. | García-Martín E, Pizarro RM, Martínez C, Gutierrez-Martín Y, Pérez G, Jover R, Agúndez JA. Acquired resistance to the anticancer drug paclitaxel is associated with induction of cytochrome P450 2C8. Pharmacogenomics. 2006;7:575-585. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 32] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 66. | Bergmann TK, Gréen H, Brasch-Andersen C, Mirza MR, Herrstedt J, Hølund B, du Bois A, Damkier P, Vach W, Brosen K. Retrospective study of the impact of pharmacogenetic variants on paclitaxel toxicity and survival in patients with ovarian cancer. Eur J Clin Pharmacol. 2011;67:693-700. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 58] [Cited by in F6Publishing: 62] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 67. | Feig C, Gopinathan A, Neesse A, Chan DS, Cook N, Tuveson DA. The pancreas cancer microenvironment. Clin Cancer Res. 2012;18:4266-4276. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 841] [Cited by in F6Publishing: 942] [Article Influence: 85.6] [Reference Citation Analysis (0)] |
| 68. | Mahadevan D, Von Hoff DD. Tumor-stroma interactions in pancreatic ductal adenocarcinoma. Mol Cancer Ther. 2007;6:1186-1197. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 429] [Cited by in F6Publishing: 441] [Article Influence: 25.9] [Reference Citation Analysis (0)] |
| 69. | Kindler HL, Niedzwiecki D, Hollis D, Sutherland S, Schrag D, Hurwitz H, Innocenti F, Mulcahy MF, O’Reilly E, Wozniak TF. Gemcitabine plus bevacizumab compared with gemcitabine plus placebo in patients with advanced pancreatic cancer: phase III trial of the Cancer and Leukemia Group B (CALGB 80303). J Clin Oncol. 2010;28:3617-3622. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 596] [Cited by in F6Publishing: 645] [Article Influence: 46.1] [Reference Citation Analysis (0)] |
| 70. | Van Cutsem E, Vervenne WL, Bennouna J, Humblet Y, Gill S, Van Laethem JL, Verslype C, Scheithauer W, Shang A, Cosaert J. Phase III trial of bevacizumab in combination with gemcitabine and erlotinib in patients with metastatic pancreatic cancer. J Clin Oncol. 2009;27:2231-2237. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 469] [Cited by in F6Publishing: 478] [Article Influence: 31.9] [Reference Citation Analysis (0)] |
| 71. | Rougier P, Riess H, Manges R, Karasek P, Humblet Y, Barone C, Santoro A, Assadourian S, Hatteville L, Philip PA. Randomised, placebo-controlled, double-blind, parallel-group phase III study evaluating aflibercept in patients receiving first-line treatment with gemcitabine for metastatic pancreatic cancer. Eur J Cancer. 2013;49:2633-2642. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 120] [Cited by in F6Publishing: 142] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 72. | Spano JP, Chodkiewicz C, Maurel J, Wong R, Wasan H, Barone C, Létourneau R, Bajetta E, Pithavala Y, Bycott P. Efficacy of gemcitabine plus axitinib compared with gemcitabine alone in patients with advanced pancreatic cancer: an open-label randomised phase II study. Lancet. 2008;371:2101-2108. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 194] [Cited by in F6Publishing: 207] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 73. | Kindler HL, Ioka T, Richel DJ, Bennouna J, Létourneau R, Okusaka T, Funakoshi A, Furuse J, Park YS, Ohkawa S. Axitinib plus gemcitabine versus placebo plus gemcitabine in patients with advanced pancreatic adenocarcinoma: a double-blind randomised phase 3 study. Lancet Oncol. 2011;12:256-262. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 291] [Cited by in F6Publishing: 299] [Article Influence: 23.0] [Reference Citation Analysis (0)] |
| 74. | Gonçalves A, Gilabert M, François E, Dahan L, Perrier H, Lamy R, Re D, Largillier R, Gasmi M, Tchiknavorian X. BAYPAN study: a double-blind phase III randomized trial comparing gemcitabine plus sorafenib and gemcitabine plus placebo in patients with advanced pancreatic cancer. Ann Oncol. 2012;23:2799-2805. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 165] [Cited by in F6Publishing: 157] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 75. | Hatzivassiliou G, Song K, Yen I, Brandhuber BJ, Anderson DJ, Alvarado R, Ludlam MJ, Stokoe D, Gloor SL, Vigers G. RAF inhibitors prime wild-type RAF to activate the MAPK pathway and enhance growth. Nature. 2010;464:431-435. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1208] [Cited by in F6Publishing: 1256] [Article Influence: 89.7] [Reference Citation Analysis (0)] |
| 76. | Alvarez R, Musteanu M, Garcia-Garcia E, Lopez-Casas PP, Megias D, Guerra C, Muñoz M, Quijano Y, Cubillo A, Rodriguez-Pascual J. Stromal disrupting effects of nab-paclitaxel in pancreatic cancer. Br J Cancer. 2013;109:926-933. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 195] [Cited by in F6Publishing: 252] [Article Influence: 22.9] [Reference Citation Analysis (0)] |
| 77. | Hingorani SR, Harris WP, Beck JT, Berdov BA, Wagner SA, Pshevlotsky EM, Tjulandin S, Gladkov O, Holcombe RF, Jiang P. A phase Ib study of gemcitabine plus PEGPH20 (pegylated recombinant human hyaluronidase) in patients with stage IV previously untreated pancreatic cancer. J Clin Oncol. 2013;31:4010. [Cited in This Article: ] |
| 78. | S1313, Combination Chemotherapy With or Without PEGPH20 in Treating Patients With Newly Diagnosed Metastatic Pancreatic Cancer. Available from: https://clinicaltrials.gov/ct2/show/NCT01959139. [Cited in This Article: ] |
| 79. | Hingorani S, Harris W, Hendifar A, Bullock A, Wu W, Huang Y, Jiang P. High Response Rate and PFS with PEGPH20 Added to Nab-Paclitaxel/Gemcitabine in Stage IV Previously Untreated Pancreatic Cancer Patients with High-HA Tumors: Interim Results of a Randomized Phase 2 Study. J Clin Oncol. 2015;33:4006. [Cited in This Article: ] |
| 80. | Koay EJ, Amer AM, Baio FE, Ondari AO, Fleming JB. Toward stratification of patients with pancreatic cancer: Past lessons from traditional approaches and future applications with physical biomarkers. Cancer Lett. 2016; Epub ahead of print. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 81. | Rhim AD, Oberstein PE, Thomas DH, Mirek ET, Palermo CF, Sastra SA, Dekleva EN, Saunders T, Becerra CP, Tattersall IW. Stromal elements act to restrain, rather than support, pancreatic ductal adenocarcinoma. Cancer Cell. 2014;25:735-747. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1359] [Cited by in F6Publishing: 1469] [Article Influence: 146.9] [Reference Citation Analysis (0)] |
| 82. | Ko AH, LoConte N, Tempero MA, Walker EJ, Kate Kelley R, Lewis S, Chang WC, Kantoff E, Vannier MW, Catenacci DV. A Phase I Study of FOLFIRINOX Plus IPI-926, a Hedgehog Pathway Inhibitor, for Advanced Pancreatic Adenocarcinoma. Pancreas. 2016;45:370-375. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 159] [Cited by in F6Publishing: 140] [Article Influence: 17.5] [Reference Citation Analysis (0)] |
| 83. | Neesse A, Frese KK, Bapiro TE, Nakagawa T, Sternlicht MD, Seeley TW, Pilarsky C, Jodrell DI, Spong SM, Tuveson DA. CTGF antagonism with mAb FG-3019 enhances chemotherapy response without increasing drug delivery in murine ductal pancreas cancer. Proc Natl Acad Sci USA. 2013;110:12325-12330. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 189] [Cited by in F6Publishing: 214] [Article Influence: 19.5] [Reference Citation Analysis (0)] |
| 84. | Picozzi VJ, Pipas JM, Koong A, Giaccia A, Bahary N, Krishnamurthi SS, Lopez CD, O’Dwyer PJ, Modelska K, Carney M. FG-3019, a human monoclonal antibody to connective tissue growth factor (CTGF), with gemcitabine/erlotinib (G/E) in patients with locally advanced or metastatic pancreatic ductal adenocarcinoma (PDAC). J Clin Oncol. 2014;32:4138. [Cited in This Article: ] |
| 85. | A Phase 1/2 Trial of Gemcitabine Plus Nab-paclitaxel With or Without FG-3019 as Neoadjuvant Chemotherapy in Locally Advanced, Unresectable Pancreatic Cancer. Clin Identifier NCT02210559. Available from: https://clinicaltrials.gov. [Cited in This Article: ] |
| 86. | Picozzi VJ, Rocha FG, Helton S, Mody K, Asbun H, Pishvaian MJ, Jackson PG, Etheridge T, Carney M, Neff TB. Randomized, open-label trial of gemcitabine/nab-paclitaxel (G/NP) FG-3019 as neoadjuvant chemotherapy in locally advanced, unresectable pancreatic cancer (LAPC). J Clin Oncol. 2016;34:457. [Cited in This Article: ] |
| 87. | Cook N, Basu B, Smith D-M, Gopinathan A, Evans TJ, Steward WP, Hagemann T, Venugopal B, Tuveson DA, Hategan M. A phase I trial of the {gamma}-secretase inhibitor (GSI) MK-0752 in combination with gemcitabine in patients with pancreatic ductal adenocarcinoma (PDAC). J Clin Oncol. 2014;32:4116. [Cited in This Article: ] |
| 88. | Dancer J, Takei H, Ro JY, Lowery-Nordberg M. Coexpression of EGFR and HER-2 in pancreatic ductal adenocarcinoma: a comparative study using immunohistochemistry correlated with gene amplification by fluorescencent in situ hybridization. Oncol Rep. 2007;18:151-155. [PubMed] [Cited in This Article: ] |
| 89. | Bittoni A, Mandolesi A, Andrikou K, Santoni M, Alfonsi S, Lanese A, Loretelli C, Pellei C, Piva F, Scarpelli M. HER family receptor expression and prognosis in pancreatic cancer. Int J Biol Markers. 2015;30:e327-e332. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 90. | Figueroa-Magalhães MC, Jelovac D, Connolly RM, Wolff AC. Treatment of HER2-positive breast cancer. Breast. 2014;23:128-136. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 136] [Cited by in F6Publishing: 158] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 91. | Safran H, Iannitti D, Ramanathan R, Schwartz JD, Steinhoff M, Nauman C, Hesketh P, Rathore R, Wolff R, Tantravahi U. Herceptin and gemcitabine for metastatic pancreatic cancers that overexpress HER-2/neu. Cancer Invest. 2004;22:706-712. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 92. | Harder J, Ihorst G, Heinemann V, Hofheinz R, Moehler M, Buechler P, Kloeppel G, Röcken C, Bitzer M, Boeck S. Multicentre phase II trial of trastuzumab and capecitabine in patients with HER2 overexpressing metastatic pancreatic cancer. Br J Cancer. 2012;106:1033-1038. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 117] [Cited by in F6Publishing: 130] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 93. | Safran H, Miner T, Bahary N, Whiting S, Lopez CD, Sun W, Charpentier K, Shipley J, Anderson E, McNulty B. Lapatinib and gemcitabine for metastatic pancreatic cancer. A phase II study. Am J Clin Oncol. 2011;34:50-52. [PubMed] [Cited in This Article: ] |
| 94. | Philip PA, Benedetti J, Corless CL, Wong R, O’Reilly EM, Flynn PJ, Rowland KM, Atkins JN, Mirtsching BC, Rivkin SE. Phase III study comparing gemcitabine plus cetuximab versus gemcitabine in patients with advanced pancreatic adenocarcinoma: Southwest Oncology Group-directed intergroup trial S0205. J Clin Oncol. 2010;28:3605-3610. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 446] [Cited by in F6Publishing: 478] [Article Influence: 34.1] [Reference Citation Analysis (0)] |
| 95. | Two Stage Study Of Single Dose PEGPH20 And Cetuximab In Patients With Pancreatic Adenocarcinoma Prior To Surgical Resection. Clin Identifier NCT02241187. Available from: https://clinicaltrials.gov. [Cited in This Article: ] |
| 96. | Afatinib as Cancer Therapy for Exocrine Pancreatic Tumours (ACCEPT). Clin Identifier NCT01728818. Available from: https://clinicaltrials.gov. [Cited in This Article: ] |
| 97. | Rinehart J, Adjei AA, Lorusso PM, Waterhouse D, Hecht JR, Natale RB, Hamid O, Varterasian M, Asbury P, Kaldjian EP. Multicenter phase II study of the oral MEK inhibitor, CI-1040, in patients with advanced non-small-cell lung, breast, colon, and pancreatic cancer. J Clin Oncol. 2004;22:4456-4462. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 488] [Cited by in F6Publishing: 509] [Article Influence: 25.5] [Reference Citation Analysis (0)] |
| 98. | Bodoky G, Timcheva C, Spigel DR, La Stella PJ, Ciuleanu TE, Pover G, Tebbutt NC. A phase II open-label randomized study to assess the efficacy and safety of selumetinib (AZD6244 [ARRY-142886]) versus capecitabine in patients with advanced or metastatic pancreatic cancer who have failed first-line gemcitabine therapy. Invest New Drugs. 2012;30:1216-1223. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 149] [Cited by in F6Publishing: 149] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 99. | Infante JR, Somer BG, Park JO, Li CP, Scheulen ME, Kasubhai SM, Oh DY, Liu Y, Redhu S, Steplewski K. A randomised, double-blind, placebo-controlled trial of trametinib, an oral MEK inhibitor, in combination with gemcitabine for patients with untreated metastatic adenocarcinoma of the pancreas. Eur J Cancer. 2014;50:2072-2081. [PubMed] [Cited in This Article: ] |
| 100. | Van Cutsem E, Hidalgo M, Bazin I, Canon J-L, Poddubskaya E, Manojlovic N, Milella M, Radenkovic D, Verslype C, Guo W. Phase II randomized trial of MEK inhibitor pimasertib or placebo combined with gemcitabine in the first-line treatment of metastatic pancreatic cancer. J Clin Oncol. 2015;33:344. [Cited in This Article: ] |
| 101. | Vena F, Li Causi E, Rodriguez-Justo M, Goodstal S, Hagemann T, Hartley JA, Hochhauser D. The MEK1/2 Inhibitor Pimasertib Enhances Gemcitabine Efficacy in Pancreatic Cancer Models by Altering Ribonucleotide Reductase Subunit-1 (RRM1). Clin Cancer Res. 2015;21:5563-5577. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 49] [Cited by in F6Publishing: 46] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 102. | Van Laethem JL, Jassem J, Heinemann V, Weekes CD, Bridgewater JA, Cascinu S, Melichar B, Peeters M, Ross PJ, Saramak P. Phase II study of refametinib (BAY 86-9766), an allosteric dual MEK 1/2 inhibitor, and gemcitabine in patients with unresectable, locally advanced, or metastatic pancreatic cancer. J Clin Oncol. 2014;32:4025. [Cited in This Article: ] |
| 103. | Zhao Y, Adjei AA. The clinical development of MEK inhibitors. Nat Rev Clin Oncol. 2014;11:385-400. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 274] [Cited by in F6Publishing: 292] [Article Influence: 29.2] [Reference Citation Analysis (0)] |
| 104. | Ko AH, Bekaii-Saab T, Van Ziffle J, Mirzoeva OM, Joseph NM, Talasaz A, Kuhn P, Tempero MA, Collisson EA, Kelley RK. A Multicenter, Open-Label Phase II Clinical Trial of Combined MEK plus EGFR Inhibition for Chemotherapy-Refractory Advanced Pancreatic Adenocarcinoma. Clin Cancer Res. 2016;22:61-68. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 79] [Cited by in F6Publishing: 88] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 105. | Tolcher AW, Bendell JC, Papadopoulos KP, Burris HA, Patnaik A, Jones SF, Rasco D, Cox DS, Durante M, Bellew KM. A phase IB trial of the oral MEK inhibitor trametinib (GSK1120212) in combination with everolimus in patients with advanced solid tumors. Ann Oncol. 2015;26:58-64. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 103] [Cited by in F6Publishing: 96] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 106. | Garajová I, Giovannetti E, Biasco G, Peters GJ. c-Met as a Target for Personalized Therapy. Transl Oncogenomics. 2015;7:13-31. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 3] [Reference Citation Analysis (0)] |
| 107. | Neuzillet C, Couvelard A, Tijeras-Raballand A, de Mestier L, de Gramont A, Bédossa P, Paradis V, Sauvanet A, Bachet JB, Ruszniewski P. High c-Met expression in stage I-II pancreatic adenocarcinoma: proposal for an immunostaining scoring method and correlation with poor prognosis. Histopathology. 2015;67:664-676. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 108. | Li C, Wu JJ, Hynes M, Dosch J, Sarkar B, Welling TH, Pasca di Magliano M, Simeone DM. c-Met is a marker of pancreatic cancer stem cells and therapeutic target. Gastroenterology. 2011;141:2218-2227.e5. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 255] [Cited by in F6Publishing: 283] [Article Influence: 21.8] [Reference Citation Analysis (0)] |
| 109. | Shah AN, Summy JM, Zhang J, Park SI, Parikh NU, Gallick GE. Development and characterization of gemcitabine-resistant pancreatic tumor cells. Ann Surg Oncol. 2007;14:3629-3637. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 315] [Cited by in F6Publishing: 352] [Article Influence: 20.7] [Reference Citation Analysis (0)] |
| 110. | Patel MB, Pothula SP, Xu Z, Lee AK, Goldstein D, Pirola RC, Apte MV, Wilson JS. The role of the hepatocyte growth factor/c-MET pathway in pancreatic stellate cell-endothelial cell interactions: antiangiogenic implications in pancreatic cancer. Carcinogenesis. 2014;35:1891-1900. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 58] [Cited by in F6Publishing: 62] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 111. | Xin X, Yang S, Ingle G, Zlot C, Rangell L, Kowalski J, Schwall R, Ferrara N, Gerritsen ME. Hepatocyte growth factor enhances vascular endothelial growth factor-induced angiogenesis in vitro and in vivo. Am J Pathol. 2001;158:1111-1120. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 286] [Cited by in F6Publishing: 280] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 112. | Avan A, Caretti V, Funel N, Galvani E, Maftouh M, Honeywell RJ, Lagerweij T, Van Tellingen O, Campani D, Fuchs D. Crizotinib inhibits metabolic inactivation of gemcitabine in c-Met-driven pancreatic carcinoma. Cancer Res. 2013;73:6745-6756. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 61] [Cited by in F6Publishing: 66] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 113. | Hage C, Rausch V, Giese N, Giese T, Schönsiegel F, Labsch S, Nwaeburu C, Mattern J, Gladkich J, Herr I. The novel c-Met inhibitor cabozantinib overcomes gemcitabine resistance and stem cell signaling in pancreatic cancer. Cell Death Dis. 2013;4:e627. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 88] [Cited by in F6Publishing: 92] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 114. | Pothula SP, Xu Z, Goldstein D, Biankin AV, Pirola RC, Wilson JS, Apte MV. Hepatocyte growth factor inhibition: a novel therapeutic approach in pancreatic cancer. Br J Cancer. 2016;114:269-280. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 75] [Cited by in F6Publishing: 69] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 115. | A Randomized Phase 2 Study of ARQ 197 Vs Gemcitabine in Treatment- Naïve Patients With Unresectable Locally Advanced or Metastatic Pancreatic Adenocarcinoma. Clin Identifier NCT005582. Available from: https://clinicaltrials.gov. [Cited in This Article: ] |
| 116. | Nagaraju GP, Mezina A, Shaib WL, Landry J, El-Rayes BF. Targeting the Janus-activated kinase-2-STAT3 signalling pathway in pancreatic cancer using the HSP90 inhibitor ganetespib. Eur J Cancer. 2016;52:109-119. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 29] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 117. | Yu H, Pardoll D, Jove R. STATs in cancer inflammation and immunity: a leading role for STAT3. Nat Rev Cancer. 2009;9:798-809. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2935] [Cited by in F6Publishing: 3111] [Article Influence: 207.4] [Reference Citation Analysis (0)] |
| 118. | Hurwitz HI, Uppal N, Wagner SA, Bendell JC, Beck JT, Wade SM, Nemunaitis JJ, Stella PJ, Pipas JM, Wainberg ZA. Randomized, Double-Blind, Phase II Study of Ruxolitinib or Placebo in Combination With Capecitabine in Patients With Metastatic Pancreatic Cancer for Whom Therapy With Gemcitabine Has Failed. J Clin Oncol. 2015;33:4039-4047. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 172] [Cited by in F6Publishing: 206] [Article Influence: 22.9] [Reference Citation Analysis (0)] |
| 119. | A Study of Ruxolitinib in Pancreatic Cancer Patients. Clin Identifier NCT02119663. Available from: https://clinicaltrials.gov. [Cited in This Article: ] |
| 120. | Study of Ruxolitinib in Pancreatic Cancer Patients (Janus 1). Clin Identifier NCT02117479. Available from: https://clinicaltrials.gov. [Cited in This Article: ] |
| 121. | van de Vijver MJ, He YD, van’t Veer LJ, Dai H, Hart AA, Voskuil DW, Schreiber GJ, Peterse JL, Roberts C, Marton MJ. A gene-expression signature as a predictor of survival in breast cancer. N Engl J Med. 2002;347:1999-2009. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4800] [Cited by in F6Publishing: 4354] [Article Influence: 197.9] [Reference Citation Analysis (0)] |
| 122. | Esquela-Kerscher A, Slack FJ. Oncomirs - microRNAs with a role in cancer. Nat Rev Cancer. 2006;6:259-269. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5384] [Cited by in F6Publishing: 5479] [Article Influence: 304.4] [Reference Citation Analysis (0)] |
| 123. | Calin GA, Croce CM. MicroRNA signatures in human cancers. Nat Rev Cancer. 2006;6:857-866. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5705] [Cited by in F6Publishing: 5849] [Article Influence: 324.9] [Reference Citation Analysis (0)] |
| 124. | Garajová I, Le Large TY, Frampton AE, Rolfo C, Voortman J, Giovannetti E. Molecular mechanisms underlying the role of microRNAs in the chemoresistance of pancreatic cancer. Biomed Res Int. 2014;2014:678401. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 38] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 125. | Bloomston M, Frankel WL, Petrocca F, Volinia S, Alder H, Hagan JP, Liu CG, Bhatt D, Taccioli C, Croce CM. MicroRNA expression patterns to differentiate pancreatic adenocarcinoma from normal pancreas and chronic pancreatitis. JAMA. 2007;297:1901-1908. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 873] [Cited by in F6Publishing: 952] [Article Influence: 56.0] [Reference Citation Analysis (0)] |
| 126. | Donahue TR, Nguyen AH, Moughan J, Li L, Tatishchev S, Toste P, Farrell JJ. Stromal microRNA-21 levels predict response to 5-fluorouracil in patients with pancreatic cancer. J Surg Oncol. 2014;110:952-959. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 36] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 127. | Hwang JH, Voortman J, Giovannetti E, Steinberg SM, Leon LG, Kim YT, Funel N, Park JK, Kim MA, Kang GH. Identification of microRNA-21 as a biomarker for chemoresistance and clinical outcome following adjuvant therapy in resectable pancreatic cancer. PLoS One. 2010;5:e10630. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 219] [Cited by in F6Publishing: 228] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 128. | Giovannetti E, Funel N, Peters GJ, Del Chiaro M, Erozenci LA, Vasile E, Leon LG, Pollina LE, Groen A, Falcone A. MicroRNA-21 in pancreatic cancer: correlation with clinical outcome and pharmacologic aspects underlying its role in the modulation of gemcitabine activity. Cancer Res. 2010;70:4528-4538. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 337] [Cited by in F6Publishing: 347] [Article Influence: 24.8] [Reference Citation Analysis (0)] |
| 129. | Caponi S, Funel N, Frampton AE, Mosca F, Santarpia L, Van der Velde AG, Jiao LR, De Lio N, Falcone A, Kazemier G. The good, the bad and the ugly: a tale of miR-101, miR-21 and miR-155 in pancreatic intraductal papillary mucinous neoplasms. Ann Oncol. 2013;24:734-741. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 65] [Cited by in F6Publishing: 73] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 130. | Wei X, Wang W, Wang L, Zhang Y, Zhang X, Chen M, Wang F, Yu J, Ma Y, Sun G. MicroRNA-21 induces 5-fluorouracil resistance in human pancreatic cancer cells by regulating PTEN and PDCD4. Cancer Med. 2016;5:693-702. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 71] [Cited by in F6Publishing: 80] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 131. | Frampton AE, Castellano L, Colombo T, Giovannetti E, Krell J, Jacob J, Pellegrino L, Roca-Alonso L, Funel N, Gall TM. MicroRNAs cooperatively inhibit a network of tumor suppressor genes to promote pancreatic tumor growth and progression. Gastroenterology. 2014;146:268-277.e18. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 126] [Cited by in F6Publishing: 129] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 132. | Boni V, Zarate R, Villa JC, Bandrés E, Gomez MA, Maiello E, Garcia-Foncillas J, Aranda E. Role of primary miRNA polymorphic variants in metastatic colon cancer patients treated with 5-fluorouracil and irinotecan. Pharmacogenomics J. 2011;11:429-436. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 74] [Cited by in F6Publishing: 90] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 133. | Rasmussen MH, Jensen NF, Tarpgaard LS, Qvortrup C, Rømer MU, Stenvang J, Hansen TP, Christensen LL, Lindebjerg J, Hansen F. High expression of microRNA-625-3p is associated with poor response to first-line oxaliplatin based treatment of metastatic colorectal cancer. Mol Oncol. 2013;7:637-646. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 66] [Cited by in F6Publishing: 76] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 134. | Boisen MK, Dehlendorff C, Linnemann D, Nielsen BS, Larsen JS, Osterlind K, Nielsen SE, Tarpgaard LS, Qvortrup C, Pfeiffer P. Tissue microRNAs as predictors of outcome in patients with metastatic colorectal cancer treated with first line Capecitabine and Oxaliplatin with or without Bevacizumab. PLoS One. 2014;9:e109430. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 37] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 135. | Huang D, Wang H, Liu R, Li H, Ge S, Bai M, Deng T, Yao G, Ba Y. miRNA27a is a biomarker for predicting chemosensitivity and prognosis in metastatic or recurrent gastric cancer. J Cell Biochem. 2014;115:549-556. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 51] [Cited by in F6Publishing: 59] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 136. | Villaruz LC, Huang G, Romkes M, Kirkwood JM, Buch SC, Nukui T, Flaherty KT, Lee SJ, Wilson MA, Nathanson KL. MicroRNA expression profiling predicts clinical outcome of carboplatin/paclitaxel-based therapy in metastatic melanoma treated on the ECOG-ACRIN trial E2603. Clin Epigenetics. 2015;7:58. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 137. | Best MG, Sol N, Kooi I, Tannous J, Westerman BA, Rustenburg F, Schellen P, Verschueren H, Post E, Koster J. RNA-Seq of Tumor-Educated Platelets Enables Blood-Based Pan-Cancer, Multiclass, and Molecular Pathway Cancer Diagnostics. Cancer Cell. 2015;28:666-676. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 569] [Cited by in F6Publishing: 548] [Article Influence: 60.9] [Reference Citation Analysis (0)] |
| 138. | Mayers JR, Wu C, Clish CB, Kraft P, Torrence ME, Fiske BP, Yuan C, Bao Y, Townsend MK, Tworoger SS. Elevation of circulating branched-chain amino acids is an early event in human pancreatic adenocarcinoma development. Nat Med. 2014;20:1193-1198. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 405] [Cited by in F6Publishing: 444] [Article Influence: 44.4] [Reference Citation Analysis (0)] |
| 139. | Chantrill LA, Nagrial AM, Watson C, Johns AL, Martyn-Smith M, Simpson S, Mead S, Jones MD, Samra JS, Gill AJ. Precision Medicine for Advanced Pancreas Cancer: The Individualized Molecular Pancreatic Cancer Therapy (IMPaCT) Trial. Clin Cancer Res. 2015;21:2029-2037. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 180] [Cited by in F6Publishing: 179] [Article Influence: 19.9] [Reference Citation Analysis (0)] |
| 140. | Sjoquist KM, Chin VT, Chantrill LA, O’Connor C, Hemmings C, Chang DK, Chou A, Pajic M, Johns AL, Nagrial AM. Personalising pancreas cancer treatment: When tissue is the issue. World J Gastroenterol. 2014;20:7849-7863. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 20] [Cited by in F6Publishing: 20] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 141. | Vaccaro V, Sperduti I, Vari S, Bria E, Melisi D, Garufi C, Nuzzo C, Scarpa A, Tortora G, Cognetti F. Metastatic pancreatic cancer: Is there a light at the end of the tunnel? World J Gastroenterol. 2015;21:4788-4801. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 51] [Cited by in F6Publishing: 53] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 142. | Nywening TM, Wang-Gillam A, Sanford DE, Belt BA, Panni RZ, Cusworth BM, Toriola AT, Nieman RK, Worley LA, Yano M. Targeting tumour-associated macrophages with CCR2 inhibition in combination with FOLFIRINOX in patients with borderline resectable and locally advanced pancreatic cancer: a single-centre, open-label, dose-finding, non-randomised, phase 1b trial. Lancet Oncol. 2016;17:651-662. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 425] [Cited by in F6Publishing: 499] [Article Influence: 62.4] [Reference Citation Analysis (0)] |
| 143. | Kjersem JB, Ikdahl T, Lingjaerde OC, Guren T, Tveit KM, Kure EH. Plasma microRNAs predicting clinical outcome in metastatic colorectal cancer patients receiving first-line oxaliplatin-based treatment. Mol Oncol. 2014;8:59-67. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 114] [Cited by in F6Publishing: 120] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 144. | Schou JV, Rossi S, Jensen BV, Nielsen DL, Pfeiffer P, Høgdall E, Yilmaz M, Tejpar S, Delorenzi M, Kruhøffer M. miR-345 in metastatic colorectal cancer: a non-invasive biomarker for clinical outcome in non-KRAS mutant patients treated with 3rd line cetuximab and irinotecan. PLoS One. 2014;9:e99886. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 54] [Cited by in F6Publishing: 59] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 145. | Zhou Y, Wan G, Spizzo R, Ivan C, Mathur R, Hu X, Ye X, Lu J, Fan F, Xia L. miR-203 induces oxaliplatin resistance in colorectal cancer cells by negatively regulating ATM kinase. Mol Oncol. 2014;8:83-92. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 127] [Cited by in F6Publishing: 144] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 146. | Cochrane DR, Spoelstra NS, Howe EN, Nordeen SK, Richer JK. MicroRNA-200c mitigates invasiveness and restores sensitivity to microtubule-targeting chemotherapeutic agents. Mol Cancer Ther. 2009;8:1055-1066. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 218] [Cited by in F6Publishing: 243] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 147. | Zhu X, Li Y, Xie C, Yin X, Liu Y, Cao Y, Fang Y, Lin X, Xu Y, Xu W. miR-145 sensitizes ovarian cancer cells to paclitaxel by targeting Sp1 and Cdk6. Int J Cancer. 2014;135:1286-1296. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 83] [Cited by in F6Publishing: 94] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 148. | Aggarwal BB, Kunnumakkara AB, Harikumar KB, Tharakan ST, Sung B, Anand P. Potential of spice-derived phytochemicals for cancer prevention. Planta Med. 2008;74:1560-1569. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 167] [Cited by in F6Publishing: 138] [Article Influence: 8.6] [Reference Citation Analysis (0)] |