Published online Aug 28, 2014. doi: 10.3748/wjg.v20.i32.11451
Revised: March 11, 2014
Accepted: April 21, 2014
Published online: August 28, 2014
The development of diagnostic imaging technology, such as multidetector computed tomography (MDCT) and magnetic resonance cholangiopancreatography (MRCP), has made it possible to obtain detailed images of the bile duct. Recent reports have indicated that a 3-dimensional (3D) reconstructed imaging system would be useful for understanding the liver anatomy before surgery. We have investigated a novel method that fuses MDCT and MRCP images. This novel system easily made it possible to detect the anatomical relationship between the vessels and bile duct in the portal hepatis. In this report, we describe a very rare case of extrahepatic cholangiocarcinoma associated with an accessory bile duct from the caudate lobe connecting with the intrapancreatic bile duct. We were unable to preoperatively detect this accessory bile duct using MDCT and MRCP. However, prior to the second operation, we were able to clearly visualise the injured accessory bile duct using our novel 3D imaging modality. In this report, we suggest that this imaging technique can be considered a novel and useful modality for understanding the anatomy of the portal hepatis, including the hilar bile duct.
Core tip: We present a case study in which 3-dimensional (3D) images were reconstructed to detect a case of extrahepatic cholangiocarcinoma associated with an accessory bile duct from the caudate lobe connecting with the intrapancreatic bile duct. We could not detect this condition preoperatively using standard imaging techniques; however, the 3D reconstruction enabled us to visualise the bile duct and treat the patient successfully.
- Citation: Miyamoto R, Oshiro Y, Hashimoto S, Kohno K, Fukunaga K, Oda T, Ohkohchi N. Three-dimensional imaging identified the accessory bile duct in a patient with cholangiocarcinoma. World J Gastroenterol 2014; 20(32): 11451-11455
- URL: https://www.wjgnet.com/1007-9327/full/v20/i32/11451.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i32.11451
In hepatobiliary and pancreatic surgery, it is important to avoid injury by taking note of any anomalies of the extrahepatic bile duct. According to previous reports, the accessory bile duct is of particular importance because it occurs relatively frequently[1-5]. It is well known that there is significant variation in the caudate lobe bile duct[6-8]. Recently, Ryu[8] were able to visualise the variation in the caudate lobe bile duct using 3-dimensional (3D) imaging techniques.
Recent advances in diagnostic imaging technology, such as endoscopic retrograde cholangiopancreatography (ERCP) and magnetic resonance cholangiopancreatography (MRCP), have enabled us to obtain detailed information of the bile duct before surgery. However, when the common bile duct is dilated, a thin ectopic bile duct may be hidden behind it[9,10]. Moreover, with the use of MRCP alone, it is impossible to know the relative positions of the bile duct with vascular components, such as the hepatic artery and portal vein, and the parenchymal organs, such as the pancreas and liver.
Many institutes in Japan have recently begun to construct 3D images from multidetector computed tomography (MDCT) datasets for patients who undergo hepatic resection in order to share the images with the surgical staff[11-14]. We have reconstructed 3D images of the liver using the Synapse Vincent medical imaging system (Fujifilm Medical, Tokyo). Furthermore, we have developed a novel 3D imaging system by integrating MDCT and MRCP images and have applied this 3D imaging technique to hepatobiliary and pancreatic surgery[15].
In this report, we treated a very rare case of extrahepatic cholangiocarcinoma associated with an accessory bile duct from the caudate lobe connected to the intrapancreatic bile duct. The first preoperative imaging studies did not reveal the accessory bile duct, but the 3D studies conducted before the second operation visualised the duct and directed us to the source of the bile leak, a finding that greatly facilitated the second operation. We suggest that preoperative 3D imaging of the bile duct can provide useful guidance during surgery.
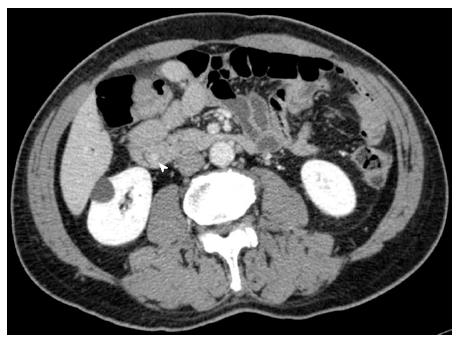
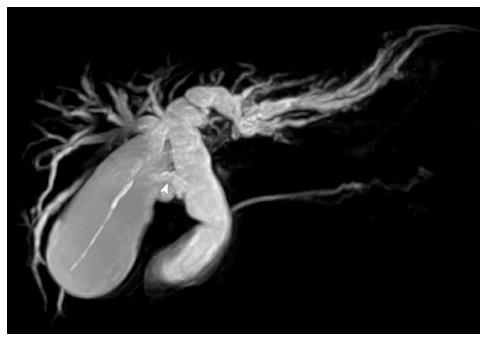
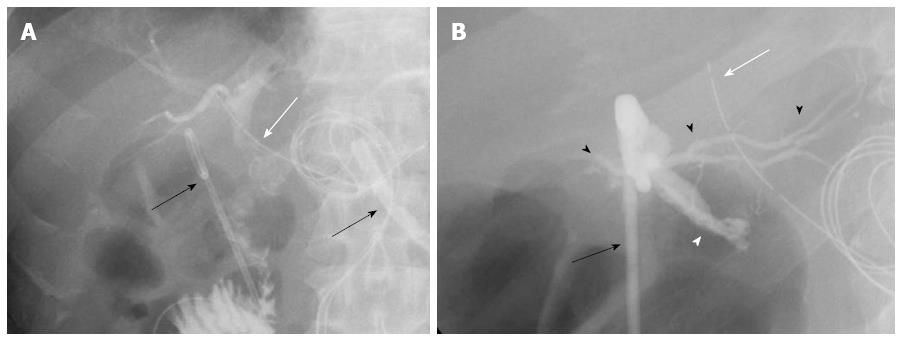
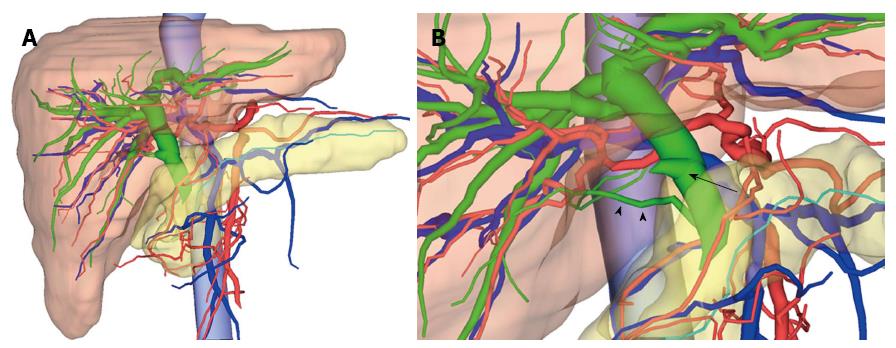
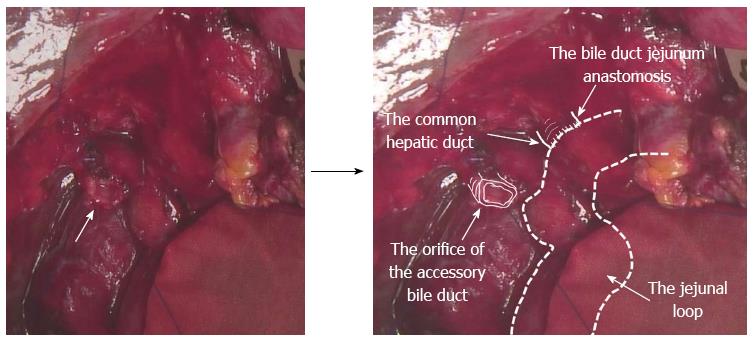
The patient was a 65-year-old male who was referred to our hospital because of jaundice. The patient was diagnosed with extrahepatic cholangiocarcinoma (cT1N0M0, Stage I) according to the Union Internationale Contre le Cancer (UICC) guidelines on the basis of a careful imaging study, including MDCT (Figure 1), MRCP (Figure 2) and ERCP. Neither our group nor the radiologists were able to preoperatively detect an accessory bile duct from the caudate lobe. The patient underwent a subtotal stomach-preserving pancreaticoduodenectomy. Because of refractory bile leakage 5 d after the operation, tubography was undertaken through the biliary drainage tube and the abdominal drainage tube. In this examination, leakage of the contrast media from the end-to-side biliojejunostomy was not observed. However, leakage was evident in images of the injured site of the bile duct (Figure 3). Furthermore, in order to clarify the injury site of the bile duct, fusion-3D images were created from preoperative MDCT and MRCP images (Figure 4). This 3D image enabled us to detect the injured accessory bile duct from the caudate lobe. Nineteen days after the first operation, the patient underwent a second operation. The intraoperative findings showed the orifice of the accessory bile duct on the surface of the liver that had been preoperatively identified on inspection of the 3D images (Figure 5). We confirmed that the bile leak was from the accessory bile duct. Abdominal drainage and an end-to-side biliojejunostomy for the injured accessory bile duct were performed. The patient had a favourable postoperative course and was discharged 16 d after the second operation. According to the UICC guidelines, the pathological classification of the tumour was pT2N1M0, Stage IIB. At the present time, the patient is currently alive without recurrence 240 d after the first operation.
Healey defined the accessory bile duct as an extrahepatic bile duct, without a bile duct connecting with the common hepatic duct within a liver[1]. Miyakawa[3] reported an accessory bile duct in 21 out of 450 (4.7%) patients. Similarly, Hisatsugu[2] reported an accessory bile duct in 616 out of 19892 (3.1%) patients undergoing bile duct surgery. They classified the accessory bile duct into seven categories based on the position on the common bile duct. In the present case, the accessory bile duct connected to the inferior common bile duct and was classified as Type IV, which comprises 3.0% of the total.
Since the study by Kumon[6] involving the use of a flexible cast, various studies have examined the caudate lobe bile duct using techniques such as radiographic evaluation. Horiguchi et al[7] examined the caudate lobe bile duct in 77 patients and reported that, in approximately 70% of cases, the bile duct from the left caudate lobe connected to the left hepatic duct. Using 3D images, Ryu[8] demonstrated that 44% of Spiegel lobe bile ducts connected to the left hepatic duct and that 90% of the caudate lobe protrusion bile ducts connected to the posterior segment bile duct. We searched Japana Centra Revuo Medicina and PubMed for reported cases of an accessory bile duct connected to the intrapancreatic bile duct and found that our case was the third to be reported[9,16] (Table 1).
| Ref. | Age | Sex | Diagnosis | Procedure |
| Ng et al[9] | 1 | F | Congenital dilation of the common bile duct | Extrahepatic bile duct resection |
| Aoki et al[16] | 72 | M | Gallbladder cancer | Extended cholecystectomy + extrahepatic bile duct resection |
| The present case | 65 | M | Extrahepatic cholangiocarcinoma | Subtotal stomach-preserving pancreaticoduodenectomy |
Hepatobiliary and pancreatic surgery requires detailed preoperative examination of the anatomy of the bile duct in order to prevent intraoperative bile duct injury. Although it is possible to obtain detailed information preoperatively because of the advances in diagnostic imaging technology such as MRCP, there is the possibility that an anomalous thin caudate lobe branch may not be detected in patients with a dilated common hepatic duct, as in our case[3,4]. We developed 3D images by integrating MDCT and MRCP images that can produce accurate preoperative anatomical images[15]. We have applied this method for the depiction of hepatic anatomy prior to hepatobiliary and pancreatic surgery. By integrating these two images, it is possible to understand the anatomical relationships between the bile duct arrangement and the vascular components, such as the hepatic artery and portal vein, and the parenchymal organs, such as the pancreas and the liver. Moreover, it became possible to share the anatomical images with the surgical staff by sharing the 3D images preoperatively.
With regard to the therapeutic method for bile duct injury, we have to consider the diameter of the bile duct and the area it covers. Longmire et al[17] reported that when the bile duct has a diameter of less than 1 mm, it can potentially be ligated if there is no infection; however, a bile duct with a diameter of 2 mm or more needs to be reconstructed. Hachisuka et al[18] also performed intraoperative bile duct imaging and evaluated the necessity of reconstruction by examining the extent of the area covered by the bile duct. In the present case, we performed a reconstruction without hesitation because it was clear that the injured site of the bile duct was the caudate lobe branch based on the 3D images. Intraoperatively, we found that the diameter was 2 mm or more.
In conclusion, we experienced a very rare case of extrahepatic cholangiocarcinoma associated with the accessory bile duct from the caudate lobe connected to the intrapancreatic bile duct, which was revealed using 3D images. A 3D imaging system such as our new modality for preoperative assessment is considered to be useful and reliable for hepatobiliary and pancreatic surgery.
In this report, authors describe a very rare case of extrahepatic cholangiocarcinoma associated with an accessory bile duct from the caudate lobe connecting with the intrapancreatic bile duct.
They were unable to preoperatively detect this accessory bile duct using multidetector computed tomography and magnetic resonance cholangiopancreatography.
However, prior to the second operation, authors were able to clearly visualise the injured accessory bile duct using our novel 3-dimensional (3D) imaging modality.
In this report, they suggest that this imaging technique can be considered a novel and useful modality for understanding the anatomy of the portal hepatis, including the hilar bile duct.
This report is well organized and documented for the significance of 3D imaging identified the accessory bile duct in a patient with cholangiocarcinoma.
P- Reviewer: Chang JH, Kim S, Sartelli M S- Editor: Gou SX L- Editor: A E- Editor: Ma S
| 1. | Healey JE, Schroy PC. Anatomy of the biliary ducts within the human liver; analysis of the prevailing pattern of branchings and the major variations of the biliary ducts. AMA Arch Surg. 1953;66:599-616. [PubMed] [Cited in This Article: ] |
| 2. | Hisatsugu T. An anomalous arrangement of the extrahepatic bile duct and surgery. Daidougakkan. 1994;27-102. [Cited in This Article: ] |
| 3. | Miyakawa T. The clinical significance of accessory bile duct: evaluation with PTC and ERCP. Jpn J Gastroenterol Surg. 1980;13:451-458. [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 4. | Moosman DA, Collier FA. Prevention of traumatic injury to the bile ducts; a study of the structures of the cystohepatic angle encountered in cholecystectomy and supraduodenal choledochostomy. Am J Surg. 1951;82:132-143. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 57] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 5. | Williams C, Williams AM. Abnormalities of the bile ducts. Ann Surg. 1955;141:598-606. [PubMed] [Cited in This Article: ] |
| 6. | Kumon M. Anatomy of the caudate lobe with special reference to portal vein and bile duct. Kanzo. 1985;26:1193-1199. [DOI] [Cited in This Article: ] [Cited by in Crossref: 106] [Cited by in F6Publishing: 108] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 7. | Horiguchi A, Miyakawa S, Miura K. Study on Radiographic Anatomy of Bile Duct of the Caudate Lobe. Fujita Gakuen Igakkaishi. 1996;20:95-98. [Cited in This Article: ] |
| 8. | Ryu T. Kanzo no Gekakaibougaku. 2nd ed. Tokyo: Igakushoin 2011; . [Cited in This Article: ] |
| 9. | Ng JW, Wong MK, Kong CK. Long accessory hepatic duct associated with congenital dilation of the common bile duct. Am J Gastroenterol. 1993;88:619-621. [PubMed] [Cited in This Article: ] |
| 10. | Narasimhan KL, Chowdhary SK, Rao KL. Management of accessory hepatic ducts in choledochal cysts. J Pediatr Surg. 2001;36:1092-1093. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Takahashi K, Sasaki R, Kondo T, Oda T, Murata S, Ohkohchi N. Preoperative 3D volumetric analysis for liver congestion applied in a patient with hilar cholangiocarcinoma. Langenbecks Arch Surg. 2010;395:761-765. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 12. | Sasaki R, Kondo T, Oda T, Murata S, Wakabayashi G, Ohkohchi N. Impact of three-dimensional analysis of multidetector row computed tomography cholangioportography in operative planning for hilar cholangiocarcinoma. Am J Surg. 2011;202:441-448. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 26] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 13. | Mise Y, Tani K, Aoki T, Sakamoto Y, Hasegawa K, Sugawara Y, Kokudo N. Virtual liver resection: computer-assisted operation planning using a three-dimensional liver representation. J Hepatobiliary Pancreat Sci. 2013;20:157-164. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 58] [Cited by in F6Publishing: 63] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 14. | Fang CH, Liu J, Fan YF, Yang J, Xiang N, Zeng N. Outcomes of hepatectomy for hepatolithiasis based on 3-dimensional reconstruction technique. J Am Coll Surg. 2013;217:280-288. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 37] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 15. | Oshiro Y, Sasaki R, Nasu K, Ohkohchi N. A novel preoperative fusion analysis using three-dimensional MDCT combined with three-dimensional MRI for patients with hilar cholangiocarcinoma. Clin Imaging. 2013;37:772-774. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 16. | Aoki H, Shinozaki S, Matsukawa H, Takakura N. A case of gallbladder cancer associated with pancreaticobiliary maljunction with long accessory hepatic duct. Tando. 2002;16:132-136. [Cited in This Article: ] |
| 17. | Longmire WP, Tompkins RK. Lesions of the segmental and lobar hepatic ducts. Ann Surg. 1975;182:478-495. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 60] [Article Influence: 1.2] [Reference Citation Analysis (0)] |