Published online Apr 7, 2014. doi: 10.3748/wjg.v20.i13.3703
Revised: December 24, 2013
Accepted: January 19, 2014
Published online: April 7, 2014
Hepatic abscess caused by foreign body penetration of the alimentary tract is rare. We report a case of gastric antrum penetration due to a toothpick complicated by liver abscess formation. A 41-year-old man was admitted to our hospital with the chief complaint of upper abdominal pain for 2 mo. Esophagogastroduodenoscopy performed at a local clinic revealed a toothpick penetrating the gastric antrum. Computed tomography (CT) of the abdomen at our hospital revealed a gastric foreign body embedded in the posterior wall of gastric antrum with regional phlegmon over the lesser sac and adhesion to the pancreatic body without notable vascular injury, and a hepatic abscess seven cm in diameter over the left liver lobe. Endoscopic removal of the foreign body was successfully performed without complication. The liver abscess was treated with parenteral antibiotics without drainage. The patient’s recovery was uneventful. Abdominal ultrasonography demonstrated complete resolution of the hepatic abscess six months after discharge. Relevant literature from the PubMed database was reviewed and the clinical presentations, diagnostic modalities, treatment strategies and outcomes of 88 reported cases were analyzed. The results showed that only 6 patients received conservative treatment with parenteral antibiotics, while the majority underwent either image-guided abscess drainage or laparotomy. Patients receiving abscess drainage via laparotomy had a significantly shorter length of hospitalization compared with those undergoing image-guided drainage. There was no significant difference in age between those who survived and those who died, however, the latter presented to hospitals in a more critical condition than the former. The overall mortality rate was 7.95%.
Core tip: Hepatic abscess caused by foreign body penetration of the alimentary tract is rare and most cases are treated surgically. We demonstrate the successful conservative treatment of a patient by combining endoscopic removal of the foreign body and broad-spectrum antibiotic coverage. A review of the literature highlighted the importance of ruling out the possibility of foreign body penetration of the alimentary tract in patients with liver abscesses and no identifiable underlying condition, particularly those refractory to conventional treatment. Appropriate diagnostic strategies, including imaging studies and surgical exploration, may be indicated for early diagnosis and timely treatment of this potentially lethal condition.
- Citation: Chong LW, Sun CK, Wu CC, Sun CK. Successful treatment of liver abscess secondary to foreign body penetration of the alimentary tract: A case report and literature review. World J Gastroenterol 2014; 20(13): 3703-3711
- URL: https://www.wjgnet.com/1007-9327/full/v20/i13/3703.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i13.3703
Accidental ingestion of foreign bodies is not uncommon and about 80%-90% of ingested foreign bodies pass through the gut uneventfully within 1 wk[1]. In fact, less than 1% of patients who ingested a foreign body developed complications such as perforation or penetration of the gastrointestinal tract[2]. The development of a hepatic abscess secondary to a foreign body penetrating the gastrointestinal tract is even more unusual. We report a case of liver abscess induced by an ingested foreign body which penetrated the gastric antrum. The abscess was successfully treated by endoscopic retrieval of the foreign body and broad-spectrum antibiotic coverage. We performed a search of relevant English literature in the PubMed database, reviewed the cases reported, and analyzed the data. Crucial information regarding this disease entity was then collected, reviewed, and summarized in this study.
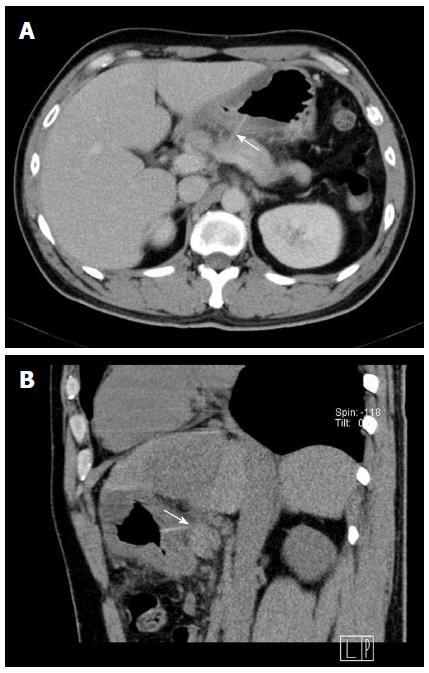
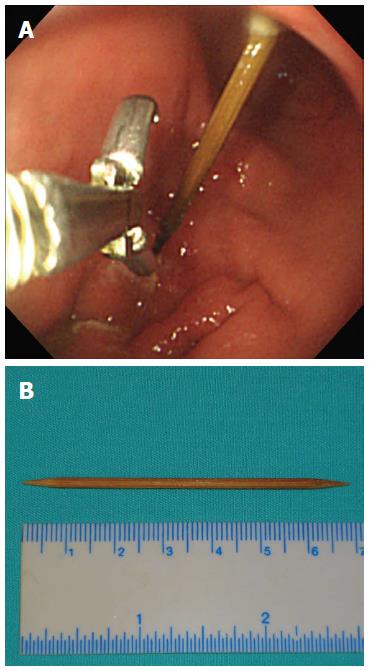
A 41-year-old man with no previous history of medical illness presented to our outpatient clinic with intermittent upper abdominal pain and acid regurgitation for two months. The patient did not experience nausea, vomiting, melena, passage of bloody stool or change in bowel habit. However, he recalled that fever occurred when the abdominal pain first started. Although he denied foreign body ingestion, esophagogastroduodenoscopy performed at a local clinic revealed a toothpick penetrating the posterior wall of the gastric antrum. He was then referred to our emergency department for further treatment. On arrival at the emergency department, his vital signs were stable with a body temperature of 36.9 °C, pulse rate of 95 breaths/min, respiratory rate of 16 breaths/min, and blood pressure of 140/71 mmHg. Physical examination was essentially normal except for mild epigastric tenderness. Laboratory studies showed a white blood cell count of 14600/mm3 with 66.4% neutrophils, a hemoglobin level of 13.4 mg/dL, and a C-reactive protein concentration of 0.535 mg/dL. Serum biochemical analyses including glucose level, renal function, liver enzymes, amylase, lipase, and alpha-fetoprotein, were all within normal limits. Blood culture yielded no bacterial growth. Chest and abdominal radiographs were unremarkable. Computed tomography (CT) of the abdomen revealed a hyperdense, linear foreign body within the gastric antrum with transgastric penetration through the posterior wall of the antrum and close contact with the pancreatic body (Figure 1). Significant edematous wall thickening of the gastric antrum and lower body with regional phlegmon over the lesser sac extending to the porta hepatis was also found. There was no apparent vascular injury. In addition, a 7-cm hypodense mass was found in the left liver lobe (Figure 2). The initial diagnosis was hepatic abscess complicating foreign body penetration of the gastric antrum. The foreign body, a 7-cm wooden toothpick, was successfully removed endoscopically using a pair of grasping forceps (FG-44NR-1, Olympus, Tokyo, Japan) (Figure 3) without notable complications. His upper abdominal pain subsided dramatically after the foreign body was removed. A parenteral proton pump inhibitor was prescribed for the small gastric ulcer resulting from removal of the foreign body. Percutaneous drainage of the liver abscess was not performed due to the absence of liquefaction. Intravenous antibiotics including ceftriaxone 2 g/d and metronidazole 500 mg every eight hours were administered. The patient was discharged after 10 d of parenteral antibiotic treatment. He remained symptom-free and treated with an oral antibiotic (levofloxacin 500 mg/d) for a further two weeks during follow-up at the outpatient clinic until C-reactive protein decreased to the normal limits. After discharge, the patient underwent serial abdominal ultrasonographic examinations every two weeks for one month and then monthly to confirm resolution of the liver abscess. Complete resolution of the hepatic abscess was noted six months after discharge.
We searched the PubMed database for relevant English literature from 1955 to 2013 using the key words “liver abscess”, “hepatic abscess”, and “foreign body”. The clinical presentations, diagnostic modalities, treatment strategies and outcomes of the reported cases were reviewed and analyzed. All statistical analyses were performed using commercially available software (SPSS, version 15.0 for Windows). Data were expressed as mean ± SD. The Student t test was used for comparison of two different sets of continuous values. Differences were considered statistically significant when P < 0.05.
The first case of hepatic abscess secondary to gastrointestinal tract perforation caused by a foreign body was reported by Lambert in 1898[3]. Since then, migrated foreign bodies, albeit uncommon, have been increasingly recognized as a potential cause of failure in the treatment of hepatic abscesses[4].
In the present study, a total of 79 journal articles were identified with 88 patients reviewed[4-82], including 64 (73%) males and 24 (27%) females. The mean age of the patients was 50.4 ± 18.6 years (ranging from 11 mo to 86 years). Although the signs and symptoms of hepatic abscesses resulting from gastrointestinal perforation by foreign bodies were often subtle and non-specific[65], abdominal pain (77.3%) and fever (58%) were the most common, followed by vomiting (19.3%) and nausea (13.6%). The frequencies of clinical manifestations in this study were consistent with those of a previous study[65]. However, weight loss, which was considered a feature of the systemic response to an ongoing infection such as abscess formation, was not apparent in the present study. Moreover, the value of a history of foreign body ingestion as a guide for diagnosis was disappointing as only 5% of patients reported a positive history[4]. In addition, our patient did not recall any episode of foreign body ingestion even after the diagnosis was made.
Of the foreign bodies reported, the frequency of occurrence in decreasing order was fish bone (33%), toothpick (27.3%), chicken bone (12.5%), and needle (9.1%), while other objects including clothespin[75], toothbrush[38,40], rosemary twig[36], pacemaker[34], rabbit bone[70], pen[59], lobster shell[77], metal wire[43], and dental plate[67] have also been sporadically documented. Similar findings were observed in a previous study[4]. The literature review in the present study demonstrated that the size of the foreign bodies ranged from as small as 1 cm (fish bone)[72] to over 19 cm (toothbrush)[38].
The review of available literature showed that the stomach was the most common site of perforation (40.9%), followed by the duodenum (20.5%) and colon (11.4%). These results are similar to those of a previous study which reported that the stomach and duodenum were the most common sites of foreign body-induced perforation[65]. With regard to the location of the hepatic abscess, the left lobe was most commonly affected (65.9%), followed by the right lobe (29.5%), and bilobar involvement (4.5%). The size of the liver abscesses ranged from 2 to 16 cm (mean, 6.82 ± 3.09 cm). In contrast to cryptogenic hepatic abscesses which often affect the right liver lobe, a predominance of left lobe involvement was noted in liver abscesses induced by foreign body penetration[4]. Furthermore, liver abscess secondary to foreign body penetration of the gastrointestinal tract should be ruled out when encountering a lesion without an identifiable underlying condition combined with treatment failure[4].
Diagnosis was made by CT in the majority of patients (53/88, 60.2%), followed by ultrasonography (21/88, 23.9%), radiographs (14/88, 15.9%), and laparotomy (13/88, 14.8%). Combined diagnostic modalities were also adopted, including the combination of ultrasonography and CT (13/88, 14.8%), radiographs and CT (3/88, 3.4%) as well as the combination of radiographs, ultrasonography and CT (6/88, 6.8%). Initial diagnosis was not established in two patients who presented to hospitals with persistent symptoms during their second visit when correct diagnoses were made[49,63]. Diagnosis was not established in seven cases until autopsy[13,20,22,26,27,71]. The frequencies of use of different diagnostic modalities are summarized in Table 1.
| Diagnostic tools | n (%) |
| Computed tomography | 53 (60.20) |
| Ultrasonography | 21 (23.90) |
| Radiographs | 14 (15.90) |
| Laparotomy | 13 (14.80) |
| Autopsy | 7 (7.95) |
| Esophagogastroduodenoscopy | 4 (4.55) |
| Colonoscopy | 3 (3.41) |
| Endoscopic ultrasonography | 1 (1.14) |
The choice of diagnostic modality depends on the nature and size of the ingested object. For instance, although plain abdominal radiography is usually the initial screening imaging study of choice for patients with a complaint of abdominal pain, the ingested foreign body is usually not identified on plain radiography unless it is radiopaque. On the other hand, a metallic object is easily detected by plain radiography, despite poor definition of the exact location. In such cases, abdominal ultrasonography may be a convenient and radiation-free screening tool for identifying the abscess and possibly the foreign body. CT, on the other hand, is the preferred imaging study for diagnosis due to its high resolution and accuracy in the identification of foreign bodies[44]. It is also useful in evaluating the depth and complication of the penetration. Indeed, the literature review in the present study showed that although there is no unanimous gold standard for the diagnosis of small-sized foreign bodies that have penetrated the alimentary tract, CT was the most commonly used diagnostic tool (60.2%). However, the accuracy of CT is limited by the lack of observer awareness. A high index of suspicion must be maintained for the correct diagnosis. It is also noteworthy that diagnosis was established only via laparotomy in up to 14.8% of all reported patients whose recovery was uneventful. Therefore, timely surgical exploration is recommended for patients with diagnostic uncertainties. Endoscopy may aid in diagnosis when it is performed at an early stage, before complete migration of the foreign body and mucosal healing[51]. In our patient, a toothpick penetrating the gastric antrum was disclosed by esophagogastroduodenoscopy as his initial presentations were upper abdominal pain and acid regurgitation. CT later revealed a 7-cm left hepatic lobe abscess.
Hepatic abscesses may result from hematogenous dissemination of pathogens via either the portal venous system from the gastrointestinal tract or the hepatic artery from sepsis, ascending cholangitis, or local spread of infection. Development of the hepatic abscess in our case was probably caused by the spread of phlegmon along the lesser sac. The clinical manifestations of hepatic abscess secondary to foreign body perforation vary and are usually subtle. In our case, classic symptoms of pyogenic hepatic abscess such as high fever and severe abdominal pain were absent. Adhesions from slow progressive inflammatory or fibrotic reactions (Figure 1) may have prevented free intra-peritoneal spillage of gastrointestinal contents and the resulting full-blown peritonitis which usually presents with high fever and severe abdominal pain. In the current study, the lack of significant differences in demographic, clinical manifestations, and pathogens between the survivors and the patients who died, except for the correct diagnosis in the former, highlighted the importance of timely diagnosis of this condition.
With regard to the identification of pathogens, a review of the relevant literature showed a single bacterial strain in the majority of cases (54.5%) with an incidence of two bacterial flora and multi-flora (i.e., three or more) being 18.2% and 12.7%, respectively. Negative culture results were noted in 14.5% of all reported cases, whereas bacterial culture was positive in only one of six (16.7%) patients in the literature with undrainable abscesses. Of all the identified pathogens, the most commonly isolated was Streptococcus species (72.3%), followed by Escherichia coli (17%) and Klebsiella pneumoniae (10.6%) (Table 2). One patient with identified candidal infection was found to have received a local steroid injection for long-standing lumbar and leg pain. An immunocompromised status due to prolonged steroid use, therefore, may have contributed to the infection. As Streptococcus species, Escherichia coli and Klebsiella pneumoniae were the most commonly identified pathogens, empirical antibiotic therapy with ampicillin/sulbactam or second-generation cephalosporins (e.g., cefoxitin) may be included in the initial treatment regimen.
| Bacterial flora | Prevalence | No. of patients |
| Streptococcus sp. | 72.30% | 34 |
| Escherichia coli | 17.00% | 8 |
| Klebsiella pneumoniae | 10.60% | 5 |
| Gram (+) cocci | 6.38% | 3 |
| Bacteroids sp. | 4.26% | 2 |
| Eikenella corrodens | 4.26% | 2 |
| Enterobacter cloacae | 4.26% | 2 |
| Mixed anaerobes | 4.26% | 2 |
| Staphylococcus aureus | 4.26% | 2 |
| Anaerobic Gram (+) cocci | 2.13% | 1 |
| Candida sp. | 2.13% | 1 |
| Enterococcus sp. | 2.13% | 1 |
| Gram (+) bacilli | 2.13% | 1 |
| Gram (-) bacilli | 2.13% | 1 |
| Proteus sp. | 2.13% | 1 |
The recommended treatment protocol for this clinical entity comprises removal of the foreign body and drainage of the hepatic abscess. In cases of hepatic abscesses related to foreign body migration, the overall rate of cure without foreign body removal is low (9.5%)[4]. Therefore, removal of the foreign body is critical for resolving the abscess and closure of the fistulous tract. Strategies for the removal of a foreign body penetrating the gastrointestinal tract include laparotomy as well as laparoscopic, endoscopic, or percutaneous interventional radiological approaches[23,31,51,62,63]. The literature review showed that the foreign bodies were removed by surgery (laparotomy or laparoscopic approach) in 62 (70.5%) patients, and by endoscopy in 10 (11.4%) patients. Other approaches included percutaneous radiological intervention[62] (n = 1, 1.1%) and ultrasound-guided fluoroscopy[29] (n = 1, 1.1%). The foreign bodies were allowed to remain in place in three (3.4%) patients[17,53,80], whereas spontaneous passage was noted in two (2.3%) cases[10,46] (Table 3). On the other hand, liver abscesses were treated by drainage via laparotomy in the majority of patients (n = 43, 48.9%), followed by image-guided drainage (n = 18, 20.5%), hepatectomy (n = 8, 9.1%), and laparoscopic drainage (n = 5, 5.7%). Six (6.8%) patients received only antibiotic treatment[17,34,51,53,69,81] (Table 4).
| Procedures | n (%) |
| Surgery | 62 (70.50) |
| Laparotomy | 54 (61.40) |
| Laparoscopy | 8 (9.10) |
| Endoscopic intervention | 10 (11.36) |
| Esophagogastroduodenoscopy | 4 (4.55) |
| Colonoscopy | 4 (4.55) |
| Sigmoidoscopy | 1 (1.14) |
| Single balloon enteroscopy | 1 (1.14) |
| Autopsy | 7 (7.95) |
| Foreign body not removed | 3 (3.41) |
| Spontaneous passage | 2 (2.27) |
| Not mentioned | 2 (2.27) |
| Percutaneous interventional radiological approach | 1 (1.14) |
| Ultrasound guided fluoroscopy | 1 (1.14) |
| Procedures | n (%) |
| Drainage via laparotomy | 43 (48.86) |
| Image guided drainage | 18 (20.45) |
| Hepatectomy | 8 (9.10) |
| Laparotomy | 6 (6.82) |
| Laparoscopy | 2 (2.27) |
| Autopsy | 7 (7.95) |
| Antibiotics alone | 6 (6.82) |
| Laparoscopic drainage | 5 (5.68) |
| Not mentioned | 1 (1.14) |
The mean length of hospitalization in the documented cases was 17.5 ± 17.3 d (ranging from 2 h to 64 d). The hospital stay was significantly shorter for patients receiving laparotomy (13.2 ± 4.6 d), compared with those undergoing abscess drainage under either CT- (47 ± 24 d) or echo-guidance (29.8 ± 22.2 d) (P < 0.05). Moreover, the hospitalization in patients receiving image-guided drainage was longer than those receiving only antibiotic treatment (11 ± 4.2 d), although the difference did not reach statistical significance (P = 0.1961). One possible explanation for this finding is that the drainage group generally had severe disease and a more complicated clinical course with larger abscesses and liquefaction compared with the antibiotics-only group. No statistically significant difference in the length of hospitalization between the open drainage and antibiotics-only groups was observed (P = 0.5489).
Although there is no established guideline regarding the choice of treatment strategy for this rare disease entity, the current study showed that abscess drainage via laparotomy in suitable candidates may shorten the length of hospital stay compared with those receiving image-guided drainage. On the other hand, the choice of conservative treatment with parenteral antibiotics may be a therapeutic option for patients with liver abscesses without evidence of liquefaction. Indeed, a liver abscess up to 7 cm was resolved after antibiotic treatment in our patient. Although the literature review in the present study showed no bacterial resistance in this clinical setting, broad-spectrum antibiotics (e.g., carbapenems) may be included in the empirical treatment regimen against drug-resistant organisms.
Most patients previously reported to have hepatic foreign bodies were treated with laparotomy which is effective, but invasive[65]. On the other hand, although endoscopy can be performed via the gastrointestinal tract, this procedure can be technically demanding[31,51]. In our case, as most of the toothpick was within the stomach and apparent intra-peritoneal free air or vascular injury was absent, endoscopic removal was the preferred treatment strategy. This was performed successfully without complication. Treatment of hepatic abscess includes drainage and antibiotic therapy. As liquefaction of the hepatic abscess was not evident in our case, conservative treatment rather than drainage was chosen. Unlike other reported cases of hepatic abscesses secondary to foreign body penetration with delayed diagnosis and complicated clinical courses[4,20,33], our patient recovered uneventfully and was discharged after 10 d of antibiotic treatment. Possible reasons for the non-complicated clinical course may be the relatively small perforation without gross intra-peritoneal spillage of gastrointestinal contents, effective antibiotic treatment against relatively less virulent bacterial flora of the upper compared with those of the lower gastrointestinal tract, and prompt removal of the foreign body before its complete migration which may have caused further damage to the surrounding structures such as the pancreatic ductal system and vasculature.
All patients with a diagnosis established during hospitalization eventually recovered regardless of the treatment strategy chosen. On the other hand, seven (four males and three females) died due to the originally undetected condition that was evident only after autopsy[13,20,22,26,27,71], giving an overall mortality rate of 7.95% (7/88). The major cause of death was septic shock. The age of the patients who died ranged from 43 to 86 years (mean 56.1 ± 15.8 years). There was no significant difference in age between the expired patients and the survivors (mean 50.4 ± 18.5 years; range 1-80 years). The overall survival rate of patients with timely diagnosis was 100% (81/81), whereas the mortality rate of those without definite diagnosis until autopsy was also 100% (7/7).
In summary, we report an unusual case of hepatic abscess caused by toothpick penetration of the gastric antrum. Although most cases of foreign body penetration of the gastrointestinal tract complicated by liver abscess are treated surgically, we demonstrated that a conservative management strategy combining endoscopic removal of the foreign body and broad-spectrum antibiotic coverage may be a feasible therapeutic option. Abscess drainage in suitable cases and identification of causative organisms are also necessary for successful conservative treatment. A review of the literature highlighted the importance of ruling out the possibility of foreign body-induced penetration of the alimentary tract in patients with liver abscesses and no identifiable underlying condition, particularly those refractory to conventional treatment. Appropriate diagnostic strategies, including imaging studies and surgical exploration, may be indicated for early diagnosis and timely treatment of this potentially lethal condition.
A 41-year-old man with no previous history of medical illness presented with intermittent upper abdominal pain for 2 mo.
Physical examination demonstrated mild epigastric tenderness on palpation.
The presence of pyogenic abscess may be assessed using abdominal sonography, whereas peptic ulcer disease and reflux esophagitis may be ruled out by esophagogastroduodenoscopy.
Not only did a hematological study show no remarkable anemia, leukocytosis or left-shift (i.e., hemoglobin concentration: 13.4 mg/dL; white blood cell count: 14600/mm3; neutrophils: 66.4%), but serum biochemical analyses also demonstrated no notable findings in C-reactive protein concentration (0.535 mg/dL), renal function, liver enzymes as well as levels of glucose, amylase, lipase, and alpha-fetoprotein.
Although chest and abdominal radiographs were unremarkable, computed tomography of the abdomen revealed a hyperdense, linear foreign body within the gastric antrum with transgastric penetration through the posterior wall of the antrum and close contact with the pancreatic body as well as a 7-cm hypodense mass in the left liver lobe.
As the patient received neither laparotomy nor drainage, no specimen was available for pathological diagnosis.
The patient was successfully treated conservatively by a combination of endoscopic foreign body removal and parenteral/oral broad-spectrum antibiotic coverage (i.e., intravenous ceftriaxone two g/d and metronidazole 500 mg every eight hours for 10 d during hospitalization; oral levofloxacin 500 mg/d for two weeks after discharge).
A review of 79 journal articles and 88 reported cases in the present study showed that most liver abscesses caused by foreign body penetration of the gastrointestinal tract were treated surgically or by image-guided drainage.
The literature review highlighted the importance of ruling out the possibility of foreign body-induced penetration of the alimentary tract in patients with liver abscesses and no identifiable underlying condition, particularly those refractory to conventional treatment and abscesses in the left liver lobe.
The strengths of the article include the comprehensiveness of review and detailed analysis of the reported cases, including demography and clinical manifestations, foreign bodies involved sites of perforation, location and size of liver abscess, tools for establishment of diagnosis, most common pathogens, treatment strategy and hospital course as well as prognosis. On the other hand, the weakness of the current study is that literature review identified only a small number of patients with undrainable abscesses who showed a high rate of negative bacterial culture so that limited insight can be gained regarding the appropriate antibiotic regimen for this patient population.
P- Reviewers: Cerwenka HR, Ferraioli G, Kirby R, Yaita K S- Editor: Zhai HH L- Editor: A E- Editor: Ma S
| 1. | McCanse DE, Kurchin A, Hinshaw JR. Gastrointestinal foreign bodies. Am J Surg. 1981;142:335-337. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 93] [Cited by in F6Publishing: 106] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 2. | Maleki M, Evans WE. Foreign-body perforation of the intestinal tract. Report of 12 cases and review of the literature. Arch Surg. 1970;101:475-477. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 133] [Cited by in F6Publishing: 146] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 3. | Lambert A. Abscess of the liver of unusual origin. NY Med J. 1898;2:177-178. [Cited in This Article: ] |
| 4. | Leggieri N, Marques-Vidal P, Cerwenka H, Denys A, Dorta G, Moutardier V, Raoult D. Migrated foreign body liver abscess: illustrative case report, systematic review, and proposed diagnostic algorithm. Medicine (Baltimore). 2010;89:85-95. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 53] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 5. | Abel RM, Fischer JE, Hendren WH. Penetration of the alimentary tract by a foreign body with migration to the liver. Arch Surg. 1971;102:227-228. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 43] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Abu-Wasel B, Eltawil KM, Keough V, Molinari M. Liver abscess caused by toothpick and treated by laparoscopic left hepatic resection: case report and literature review. BMJ Case Rep. 2012;2012. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Ariyuca S, Doğan M, Kaya A, Ay M. An unusual cause of liver abscess. Liver Int. 2009;29:1552. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 8. | Avcu S, Unal O, Ozen O, Bora A, Dülger AC. A swallowed sewing needle migrating to the liver. N Am J Med Sci. 2009;1:193-195. [PubMed] [Cited in This Article: ] |
| 9. | Berk RN, Reit RJ. Intra-abdominal chicken-bone abscess. Radiology. 1971;101:311-313. [PubMed] [Cited in This Article: ] |
| 10. | Bilimoria KY, Eagan RK, Rex DK. Colonoscopic identification of a foreign body causing an hepatic abscess. J Clin Gastroenterol. 2003;37:82-85. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 11. | Bloch DB. Venturesome toothpick. A continuing source of pyogenic hepatic abscess. JAMA. 1984;252:797-798. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 29] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 12. | Broome CJ, Peck RJ. Hepatic abscess complicating foreign body perforation of the gastric antrum: an ultrasound diagnosis. Clin Radiol. 2000;55:242-243. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 21] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 13. | Byard RW, Gilbert JD. Hepatic abscess formation and unexpected death: a delayed complication of occult intraabdominal foreign body. Am J Forensic Med Pathol. 2001;22:88-91. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 19] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Chan SC, Chen HY, Ng SH, Lee CM, Tsai CH. Hepatic abscess due to gastric perforation by ingested fish bone demonstrated by computed tomography. J Formos Med Assoc. 1999;98:145-147. [PubMed] [Cited in This Article: ] |
| 15. | Chen HK, Kuo JR, Uen YH, Sun DP. Liver abscess secondary to fish bone migration from the duodenum. ANZ J Surg. 2011;81:206. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 14] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 16. | Cheung YC, Ng SH, Tan CF, Ng KK, Wan YL. Hepatic inflammatory mass secondary to toothpick perforation of the stomach: triphasic CT appearances. Clin Imaging. 2000;24:93-95. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 25] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 17. | Chiang TH, Liu KL, Lee YC, Chiu HM, Lin JT, Wang HP. Sonographic diagnosis of a toothpick traversing the duodenum and penetrating into the liver. J Clin Ultrasound. 2006;34:237-240. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 18. | Chintamani V, Lubhana P, Durkhere R, Bhandari S. Liver abscess secondary to a broken needle migration--a case report. BMC Surg. 2003;3:8. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 44] [Cited by in F6Publishing: 52] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 19. | Clarençon F, Scatton O, Bruguière E, Silvera S, Afanou G, Soubrane O, Vignaux O, Legmann P. Recurrent liver abscess secondary to ingested fish bone migration: report of a case. Surg Today. 2008;38:572-575. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 20. | de la Vega M, Rivero JC, Ruíz L, Suárez S. A fish bone in the liver. Lancet. 2001;358:982. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 45] [Cited by in F6Publishing: 51] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 21. | Drnovsek V, Fontanez-Garcia D, Wakabayashi MN, Plavsic BM. Gastrointestinal case of the day. Pyogenic liver abscess caused by perforation by a swallowed wooden toothpick. Radiographics. 1999;19:820-822. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 28] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 22. | Dugger K, Lebby T, Brus M, Sahgal S, Leikin JB. Hepatic abscess resulting from gastric perforation of a foreign object. Am J Emerg Med. 1990;8:323-325. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 29] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 23. | Glick WA, Simo KA, Swan RZ, Sindram D, Iannitti DA, Martinie JB. Pyogenic hepatic abscess secondary to endolumenal perforation of an ingested foreign body. J Gastrointest Surg. 2012;16:885-887. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 25] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 24. | Goh BK, Yong WS, Yeo AW. Pancreatic and hepatic abscess secondary to fish bone perforation of the duodenum. Dig Dis Sci. 2005;50:1103-1106. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 31] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 25. | Gonzalez JG, Gonzalez RR, Patiño JV, Garcia AT, Alvarez CP, Pedrosa CS. CT findings in gastrointestinal perforation by ingested fish bones. J Comput Assist Tomogr. 1988;12:88-90. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 44] [Cited by in F6Publishing: 49] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 26. | Gower ND, Mond NC, Owen D. Liver abscess after perforation of liver by a fish bone. Br Med J. 1961;1:475-476. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 27. | Griffiths FE. Liver abscess due to foreign-body migration from the alimentary tract; a report of two cases. Br J Surg. 1955;42:667-668. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 10] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 28. | Gundara JS, Harrison R. An unusual zoonosis: liver abscess secondary to asymptomatic colonic foreign body. HPB Surg. 2010;2010:794271. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 29. | Horii K, Yamazaki O, Matsuyama M, Higaki I, Kawai S, Sakaue Y. Successful treatment of a hepatic abscess that formed secondary to fish bone penetration by percutaneous transhepatic removal of the foreign body: report of a case. Surg Today. 1999;29:922-926. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 49] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 30. | Houli N, MacGowan K, Hosking P. Hepatic abscess complicating foreign body perforation of the transverse colon. ANZ J Surg. 2003;73:255-259. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 31. | Hsieh MJ, Lee TC, Tseng CH, Lin TH, Liu KL, Chen SY, Wang HP. Duodenum-penetrating toothpick with liver abscess: removal with single-balloon enteroscopy. Endoscopy. 2011;43 Suppl 2 UCTN:E11-E12. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 32. | Jutte E, Cense H. Liver abscess due to sewing needle perforation. ScientificWorldJournal. 2010;10:1532-1534. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 33. | Kadowaki Y, Tamura R, Okamoto T, Mori T, Mori T. Ruptured hepatic abscess caused by fish bone penetration of the duodenal wall: report of a case. Surg Today. 2007;37:1018-1021. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 17] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 34. | Kamaruddin MS, Ramachandran MS, Turner GB, Yousaf M, McConville P, Wilson C, Clements WB. An unexpected finding during gastroscopy. Br J Hosp Med (Lond). 2006;67:154-155. [PubMed] [Cited in This Article: ] |
| 35. | Kanazawa S, Ishigaki K, Miyake T, Ishida A, Tabuchi A, Tanemoto K, Tsunoda T. A granulomatous liver abscess which developed after a toothpick penetrated the gastrointestinal tract: report of a case. Surg Today. 2003;33:312-314. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 34] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 36. | Karamarkovic AR, Djuranovic SP, Popovic NP, Bumbasirevic VD, Sijacki AD, Blazic IV. Hepatic abscess secondary to a rosemary twig migrating from the stomach into the liver. World J Gastroenterol. 2007;13:5530-5532. [PubMed] [Cited in This Article: ] |
| 37. | Kessler AT, Kourtis AP. Images in clinical medicine. Liver abscess due to Eikenella corrodens from a fishbone. N Engl J Med. 2001;345:e5. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 25] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 38. | Kim IH, Kim HC, Koh KH, Kim SH, Kim SW, Lee SO, Lee ST. Journey of a swallowed toothbrush to the colon. Korean J Intern Med. 2007;22:106-108. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 39. | Kim YM, Lee TH, Jung SH, Kim SM, Im EH, Huh KC, Choi YW, Kang YW. Hepatic abscess that formed secondary to fish bone and had a fistula with the ascending colon. Dig Dis Sci. 2007;52:3515-3518. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 40. | Kumar S, Gupta NM. Foreign bodies migrating from gut to liver. Indian J Gastroenterol. 2000;19:42. [PubMed] [Cited in This Article: ] |
| 41. | Lanthaler M, Grissmann T, Schwentner L, Nehoda H. Unusual differential diagnosis of upper abdominal pain. Diagn Ther Endosc. 2009;2009:817052. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 42. | Lawhorne TW, Schaff HV. Occult liver abscess and foreign body perforation of the bowel. Am Surg. 1979;45:659-661. [PubMed] [Cited in This Article: ] |
| 43. | Lee KF, Chu W, Wong SW, Lai PB. Hepatic abscess secondary to foreign body perforation of the stomach. Asian J Surg. 2005;28:297-300. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 20] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 44. | Liu HJ, Liang CH, Huang B, Xie SF, Wang GY. Migration of a swallowed toothpick into the liver: the value of multiplanar CT. Br J Radiol. 2009;82:e79-e81. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 45. | Liu YY, Tseng JH, Yeh CN, Fang JT, Lee HL, Jan YY. Correct diagnosis and successful treatment for pericardial effusion due to toothpick injury: a case report and literature review. World J Gastroenterol. 2007;13:4278-4281. [PubMed] [Cited in This Article: ] |
| 46. | Lowry P, Rollins NK. Pyogenic liver abscess complicating ingestion of sharp objects. Pediatr Infect Dis J. 1993;12:348-350. [PubMed] [Cited in This Article: ] |
| 47. | MacFadden DR, Penner TP, Gold WL. Persistent epigastric pain in an 80-year-old man. CMAJ. 2011;183:925-928. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 48. | Manzia TM, Sforza D, Biancone L, Tisone G. Liver abscess caused by foreign body ingestion. Dig Liver Dis. 2013;45:699. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 49. | Masoodi I, Alsayari K, Al Mohaimeed K, Ahmad S, Almtawa A, Alomair A, Alqutub A, Khan S. Fish bone migration: an unusual cause of liver abscess. BMJ Case Rep. 2012;2012. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 50. | Masunaga S, Abe M, Imura T, Asano M, Minami S, Fujisawa I. Hepatic abscess secondary to a fishbone penetrating the gastric wall: CT demonstration. Comput Med Imaging Graph. 1991;15:113-116. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 37] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 51. | Mukkada RJ, Chettupuzha AP, Francis VJ, Mathew PG, Chirayath SP, Koshy A, Augustine P. Endoscopic removal of chicken bone that caused gastric perforation and liver abscess. Indian J Gastroenterol. 2007;26:246-247. [PubMed] [Cited in This Article: ] |
| 52. | Müller-Lissner SA, Fuhrmann E. A prematurely terminated journey. Gut. 2011;60:630, 687. [PubMed] [Cited in This Article: ] |
| 53. | Ng CT, Htoo A, Tan SY. Fish bone-induced hepatic abscess: medical treatment. Singapore Med J. 2011;52:e56-e58. [PubMed] [Cited in This Article: ] |
| 54. | Nisbet M, Thomas M. Liver abscess associated with persistent Streptococcus anginosus bacteremia. Clin Infect Dis. 2005;41:352-353, 403-405. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 55. | Noel GJ, Karasic RB. Liver abscess following ingestion of a foreign body. Pediatr Infect Dis. 1984;3:342-344. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 15] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 56. | Paraskeva KD, Bury RW, Isaacs P. Streptococcus milleri liver abscesses: an unusual complication after colonoscopic removal of an impacted fish bone. Gastrointest Endosc. 2000;51:357-358. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 20] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 57. | Pedersen VM, Geerdsen JP, Bartholdy J, Kjaergaard H. Foreign body perforation of the gastrointestinal tract with formation of liver abscess. Ann Chir Gynaecol. 1986;75:245-246. [PubMed] [Cited in This Article: ] |
| 58. | Perera MT, Wijesuriya SR, Kumarage SK, Ariyaratne MH, Deen KI. Inflammatory pseudotumour of the liver caused by a migrated fish bone. Ceylon Med J. 2007;52:141-142. [PubMed] [Cited in This Article: ] |
| 59. | Perkins M, Lovell J, Gruenewald S. Life-threatening pica: liver abscess from perforating foreign body. Australas Radiol. 1999;43:349-352. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 60. | Rafizadeh F, Silver H, Fieber S. Pyogenic liver abscess secondary to a toothpick penetrating the gastrointestinal tract. J Med Soc N J. 1981;78:377-378. [PubMed] [Cited in This Article: ] |
| 61. | Reccia I, Cois A, Pisanu A, Uccheddu A. A rare cause of an unresolving liver abscess. Liver Int. 2011;31:1199. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 62. | Riani EB, Tancredi I, Sempoux C, Hubert C, Goffette P, Gigots JF. From interventional radiology to laparoscopic liver resection as complementary strategies in the treatment of hepatic abscess caused by ingested foreign bodies. Hepatogastroenterology. 2012;59:558-560. [PubMed] [Cited in This Article: ] |
| 63. | Ricci G, Campisi N, Capuano G, De Vido L, Lazzaro L, Simonatto G, Termini B, Turriziani V, Fidanza F. Liver abscess and pseudotumoral gastric lesion caused by chicken bone perforation: laparoscopic management. Case Rep Surg. 2012;2012:791857. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 64. | Rozanski M, Neuhaus V, Fahrner R, Schoeb O. Successful laparoscopic treatment of a hepatic abscess due to a chicken bone. Am Surg. 2010;76:1027-1028. [PubMed] [Cited in This Article: ] |
| 65. | Santos SA, Alberto SC, Cruz E, Pires E, Figueira T, Coimbra E, Estevez J, Oliveira M, Novais L, Deus JR. Hepatic abscess induced by foreign body: case report and literature review. World J Gastroenterol. 2007;13:1466-1470. [PubMed] [Cited in This Article: ] |
| 66. | Serwe S, Weber J, Strock P, Lens V. Liver abscess caused by an unnoticed swallowed toothpick perforating the colonic wall. Z Gastroenterol. 2007;45:1060-1062. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 67. | Shaw PJ, Freeman JG. The antemortem diagnosis of pyogenic liver abscess due to perforation of the gut by a foreign body. Postgrad Med J. 1983;59:455-456. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 21] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 68. | Starakis I, Karavias D, Marangos M, Psoni E, Bassaris H. A rooster’s revenge: hepatic abscess caused by a chicken bone. Eur J Emerg Med. 2005;12:41-42. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 69. | Stoica M, Sãftoiu A, Gheonea DI, Dumitrescu D, Surlin V. Pyogenic liver abscess caused by accidental ingestion of a wooden toothpick: role of preoperative imaging. J Gastrointestin Liver Dis. 2007;16:221-222. [PubMed] [Cited in This Article: ] |
| 70. | Tallón Aguilar L, Bernal Moreno DA, López Porras M, Marín Gómez LM, Pareja Ciuró F. Foreign bodies as infrequent cause of liver abscess. Rev Esp Enferm Dig. 2011;103:334-335. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 71. | Theodoropoulou A, Roussomoustakaki M, Michalodimitrakis MN, Kanaki C, Kouroumalis EA. Fatal hepatic abscess caused by a fish bone. Lancet. 2002;359:977. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 42] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 72. | Tomimori K, Nakasone H, Hokama A, Nakayoshi T, Sakugawa H, Kinjo F, Shiraishi M, Nishimaki T, Saito A. Liver abscess. Gastrointest Endosc. 2004;59:397-398. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 73. | Tsai JL, Than MM, Wu CJ, Sue D, Keh CT, Wang CC. Liver abscess secondary to fish bone penetration of the gastric wall: a case report. Zhonghua Yi Xue Zazhi (Taipei). 1999;62:51-54. [PubMed] [Cited in This Article: ] |
| 74. | Tsuboi K, Nakajima Y, Yamamoto S, Nagao M, Nishimura K, Yoshii M. [A case of an intrahepatic fish bone penetration--possibility of the preoperative diagnosis by CT scan (author’s transl)]. Nihon Geka Hokan. 1981;50:899-903. [PubMed] [Cited in This Article: ] |
| 75. | Tsui BC, Mossey J. Occult liver abscess following clinically unsuspected ingestion of foreign bodies. Can J Gastroenterol. 1997;11:445-448. [PubMed] [Cited in This Article: ] |
| 76. | Udawat HP, Vashishta A, Udawat H, Shah CK, Rai RR. Education and imaging: Hepatobiliary and pancreatic: liver abscess caused by an ingested foreign body. J Gastroenterol Hepatol. 2009;24:1575. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 77. | Wasserman E, Lee R, Song J, Ehrlich T. Gastric perforation with an associated subhepatic liver abscess related to an accidentally ingested lobster shell. J Clin Gastroenterol. 2008;42:553-554. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 78. | Wood MK, Harrison MR. ‘A-pin-dicitis’ and liver abscess. JAMA. 1981;246:940. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 79. | Yamaguchi N, Suzuki A. Electronic clinical challenges and images in GI. Shivering and right upper quadrant pain. Gastroenterology. 2010;138:e1-e2. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 80. | Yang CY, Kao JH, Liu KL, Chen SJ. Medical treatment of fish bone-related liver abscess. Clin Infect Dis. 2005;41:1689-1690. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 81. | Yen HH, Hsu YC. Education and Imaging: Gastrointestinal: pyogenic liver abscess associated with a penetrating fish bone. J Gastroenterol Hepatol. 2010;25:1900. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 82. | Zambrana JL, García-Gutiérrez JA, Díez F. Subphrenic abscess related to the ingestion of a toothpick. N Engl J Med. 1998;338:133-134. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 16] [Article Influence: 0.6] [Reference Citation Analysis (0)] |