Published online Apr 21, 2013. doi: 10.3748/wjg.v19.i15.2441
Revised: March 1, 2013
Accepted: March 15, 2013
Published online: April 21, 2013
At present, radical resection remains the only effective treatment for patients with hilar cholangiocarcinoma. The surgical approach for R0 resection of hilar cholangiocarcinoma is complex and diverse, but for the biliary reconstruction after resection, almost all surgeons use Roux-en-Y hepaticojejunostomy. A viable alternative to Roux-en-Y reconstruction after radical resection of hilar cholangiocarcinoma has not yet been proposed. We report a case of performing duct-to-duct biliary reconstruction after radical resection of Bismuth IIIa hilar cholangiocarcinoma. End-to-end anastomosis between the left hepatic duct and the distal common bile duct was used for the biliary reconstruction, and a single-layer continuous suture was performed along the bile duct using 5-0 prolene. The patient was discharged favorably without biliary fistula 2 wk later. Evidence for tumor recurrence was not found after an 18 mo follow-up. Performing bile duct end-to-end anastomosis in hilar cholangiocarcinoma can simplify the complex digestive tract reconstruction process.
Core tip: Roux-en-Y anastomosis is the standard of care for biliary reconstruction after radical resection of hilar cholangiocarcinoma. However, a direct duct-to-duct biliary reconstruction preserves the normal sphincter mechanism and endoscopic access to the biliary tree for diagnostic and therapeutic purposes. Duct-to-duct biliary reconstruction is widely used in liver transplantation and hepatic resection. The objective of this study was to determine the feasibility of duct-to-duct biliary reconstruction in the setting of Bismuth IIIa hilar cholangiocarcinoma with limited biliary confluence involvement.
- Citation: Wu WG, Gu J, Dong P, Lu JH, Li ML, Wu XS, Yang JH, Zhang L, Ding QC, Weng H, Ding Q, Liu YB. Duct-to-duct biliary reconstruction after radical resection of Bismuth IIIa hilar cholangiocarcinoma. World J Gastroenterol 2013; 19(15): 2441-2444
- URL: https://www.wjgnet.com/1007-9327/full/v19/i15/2441.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i15.2441
Surgical outcomes for treating hilar cholangiocarcinoma have gradually improved due to advances in surgical procedures and the accumulation of anatomic knowledge concerning the hepatic hilum[1-5]. As cancer-free margins are considered to be particularly important for curative resection of hilar cholangiocarcinoma[6], bile ducts should be dissected longitudinally as far from the tumor as possible to ensure curative resection[7]. For biliary reconstruction after resection, almost all surgeons use Roux-en-Y hepaticojejunostomy[1-7]. Following curative resection of a tumor, if there is still sufficient tissue available for remodeling the normal biliary structure, should hepatic duct and common bile duct one stage anastomosis be considered? We report a case of performing duct-to-duct biliary one stage reconstruction for biliary reconstruction after radical resection of Bismuth IIIa hilar cholangiocarcinoma. Evidence for tumor recurrence was not found after an 18 mo follow-up.
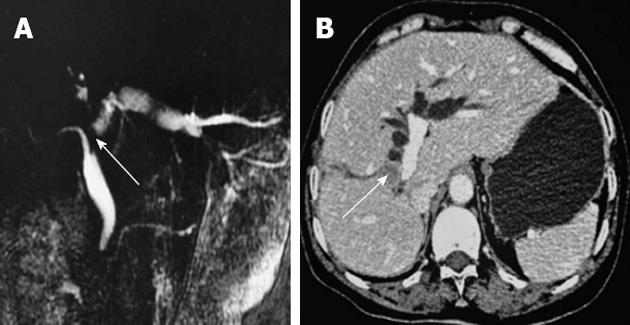
The patient, a 58-year old female, was admitted to the hospital on February 15, 2011 because of “paroxysmal right upper quadrant pain for one week”. Admission examination: body skin and sclera are slightly yellow; the whole abdomen is soft, with no tenderness, no rebound tenderness and no mass; and no other symptoms are noted. Liver function: Glutamic-pyvuvic-transaminase 213 U/L, Glutamic-oxaiacetic-transaminase 177 U/L, alkaline phosphatase 1171 U/L, gamma-glutamyltransferase 1262 U/L, total bilirubin 21.3 μmol/L, direct bilirubin 8.8 μmol/L. Tumor markers: carbohydrate antigen 19-9 336.10 U/mL, carbohydrate antigen-50 38.46 U/mL, alpha fetoprotein 1.88 ng/mL. Magnetic resonance cholangiopancreatograph (MRCP)/abdominal enhanced computed tomography (CT): hepatic portal soft tissue signal intensity, approximately 1.6 cm in diameter, and the common bile duct proximal locally shows truncated change. The extrahepatic bile duct widened, and the left hepatic intrahepatic bile duct dilatation staggered. Hepatic cirrhosis was noted. A diagnosis of hilar cholangiocarcinoma (Bismuth IIIa type) was made (Figure 1).
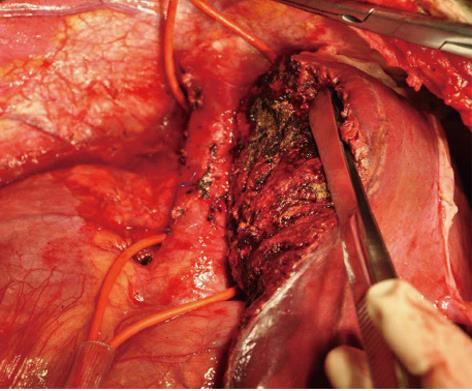
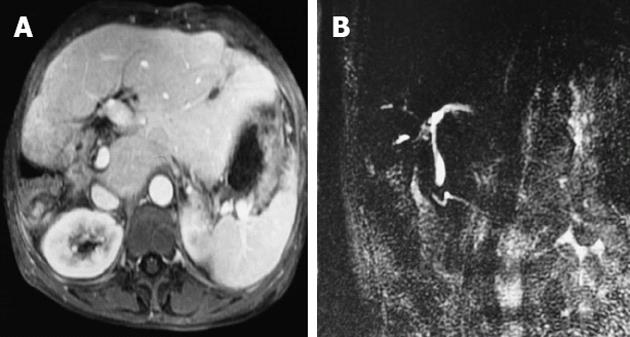
The patient underwent right hemihepatectomy with caudate process lobectomy on February 18 and systematic lymphadenectomy of the nodes (Figure 2). The lymph node groups resected en bloc included the anterior pancreaticoduodenal lymph nodes (lymph node station 17 in the Japanese system), the posterior pancreaticoduodenal lymph nodes (station 13), nodes in the hepatoduodenal ligament (stations 12a, 12b and 12c), nodes along the common hepatic artery (station 8a), and the superior pyloric node (station 5). Intraoperative frozen pathological examination indicated duct cell carcinoma in the right hepatic duct and common bile duct. Negative margins were found on the left hepatic duct and common bile duct (Figure 3). After removal of the right lobe and the caudate process, the left hepatic duct and distal common bile duct end-to-end anastomoses were used for the biliary reconstruction and a biliary stent was placed in the bile duct. The specific method of the bile duct reconstruction was as follows: (1) ensure blood supply of the left hepatic duct and common bile duct resection margin; (2) mobilization of the left liver was performed from the left side followed by the Kocher maneuver to release the duodenal descending portion to reduce anastomosis tension; and (3) single-layer continuous suture was performed for bile duct reconstruction with 5-0 prolene (Figure 4). Ten days after the operation, liver function had generally returned to normal. The patient was discharged favorably without biliary fistula 2 wk later. Postoperative pathology indicated hilar bile duct adenocarcinoma grade II involving the right hepatic duct. A 2 cm diameter tumor was found with invasion to the fibrous muscular layer and outer connective tissue. The common bile duct and the left hepatic duct resection margin was negative. The tumor-free margin of the left duct was approximately 5 mm in the final postoperative pathological assessment. No regional lymph node metastasis was observed in a total of 19 dissected nodes. Consequently, the tumor was staged according to the American Joint Commission on Cancer staging as T2N0M0. No evidence of tumor recurrence was found using MRCP scans 18 mo post-operation (Figure 5).
Surgical radical resection currently remains the only effective method that increases long-term survival for treating patients with hilar cholangiocarcinoma[8]. The hilar cholangiocarcinoma surgical approach is complex and diverse; however, for biliary reconstruction after resection, almost all surgeons use the biliary-enteric Roux-en-Y anastomosis method. The Roux-en-Y hepaticojejunostomy is primarily preferred for the following reasons: (1) it is imperative to remove as much of the bile duct as possible to ensure that the bile duct resection margin is negative; (2) removal of the common bile duct simplifies the hepatoduodenal ligament lymphadenectomy, reduces the difficulty of lymphadenectomy and generally improves its quality; and (3) the lower tension of Roux-en-Y hepaticojejunostomy reduces the occurrence of postoperative biliary fistula. However, performing duct-to-duct biliary reconstruction in hilar cholangiocarcinoma can simplify the complex digestive tract reconstruction process required in the traditional Roux-en-Y hepaticojejunostomy because it requires less radical alteration to normal gastrointestinal physiology, reduces some postoperative complications, and can simplify the treatment of complications. The faster anastomotic procedure in duct-to-duct may be another advantage over Roux-en-Y hepaticojejunostomy.
Studies suggest that the invasion longitude of hilar cholangiocarcinoma along the bile duct varies significantly, with distances ranging from a few millimeters to several centimeters[9], with variations related to bile duct cancer type, degree of differentiation, and other factors. A positive bile duct resection margin not only correlates with higher local recurrence rate after surgery but is also an independent risk factor for poor prognosis of hilar cholangiocarcinoma; furthermore, its role is similar to a positive lymph node[10]. Unfortunately, preoperative procedures such as CT or MRCP, and even intraoperative exploration, cannot conclusively determine bile duct involvement. At present, intraoperative frozen pathological examination of bile duct resection margins is an important method to determine if a clean bile duct resection margin was achieved. For cases with intraoperative local excision of bile duct and a frozen pathological examination indicating a negative resection, it may be unnecessary to expand the scope of the bile duct resection and perform the routine Roux-en-Y hepaticojejunostomy. If there is still sufficient tissue available for remodeling the normal biliary structure after the tumor R0 resection, should hepatic duct and common bile duct one stage anastomosis be considered? In addition, performing the skeletonization of the hepatoduodenal ligament in carcinoma of the gallbladder or intrahepatic cholangiocarcinoma does not require the expense of the extrahepatic bile duct to reduce the difficulty of operation and improve the quality of skeletonization. The current practice of unconditional selection of the Roux-en-Y hepaticojejunostomy to reconstruct the biliary tract for hilar cholangiocarcinoma requires further reflection and research. Duct-to-duct anastomosis is currently a favorable method to reconstruct the biliary tract, even in live donor liver transplantation[11,12]. Technically easier manipulation and the preservation of physiologic bilioenteric continuity are two main advantages of duct-to-duct anastomosis over Roux-en-Y hepaticojejunostomy. Furthermore, following Roux-en-Y hepaticojejunostomy, the loss of the normal biliary tract and the digestive tract anatomical structures makes anastomotic stenosis or stone formation relatively complicated to address using minimally invasive endoscopic retrograde cholangiopancreatography and other treatments. These complications represent clinical issues that need to be considered. Therefore, we believe that in the case of intraoperative frozen pathology indicating a negative bile duct resection margin, it is unnecessary to expand the removal of bile duct. For cases with a lesser degree of bile duct resection, duct-to-duct anastomosis of the bile duct should be considered. Provided that the blood supply of the bile duct stump is adequate, performing end-to-end tension-free anastomosis is the most effective way to ensure the anastomosis is secure, which can reduce the occurrence of the postoperative biliary fistula.
In conclusion, duct-to-duct biliary reconstruction may be a better option for bile duct reconstruction after R0 resection of hilar cholangiocarcinoma when sufficient bile duct remains for remodeling the normal biliary structure. However, the precise candidates for duct-to-duct anastomosis are difficult to define and still require further investigation.
P- Reviewers Fan ST, Cho A S- Editor Gou SX L- Editor A E- Editor Li JY
| 1. | Tsao JI, Nimura Y, Kamiya J, Hayakawa N, Kondo S, Nagino M, Miyachi M, Kanai M, Uesaka K, Oda K. Management of hilar cholangiocarcinoma: comparison of an American and a Japanese experience. Ann Surg. 2000;232:166-174. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 193] [Cited by in F6Publishing: 173] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 2. | Jarnagin WR, Fong Y, DeMatteo RP, Gonen M, Burke EC, Bodniewicz BS J, Youssef BA M, Klimstra D, Blumgart LH. Staging, resectability, and outcome in 225 patients with hilar cholangiocarcinoma. Ann Surg. 2001;234:507-517; discussion 517-519. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 973] [Cited by in F6Publishing: 920] [Article Influence: 40.0] [Reference Citation Analysis (0)] |
| 3. | Seyama Y, Kubota K, Sano K, Noie T, Takayama T, Kosuge T, Makuuchi M. Long-term outcome of extended hemihepatectomy for hilar bile duct cancer with no mortality and high survival rate. Ann Surg. 2003;238:73-83. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 176] [Cited by in F6Publishing: 239] [Article Influence: 11.4] [Reference Citation Analysis (1)] |
| 4. | Kawasaki S, Imamura H, Kobayashi A, Noike T, Miwa S, Miyagawa S. Results of surgical resection for patients with hilar bile duct cancer: application of extended hepatectomy after biliary drainage and hemihepatic portal vein embolization. Ann Surg. 2003;238:84-92. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 154] [Cited by in F6Publishing: 221] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 5. | Sano T, Shimada K, Sakamoto Y, Yamamoto J, Yamasaki S, Kosuge T. One hundred two consecutive hepatobiliary resections for perihilar cholangiocarcinoma with zero mortality. Ann Surg. 2006;244:240-247. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 172] [Cited by in F6Publishing: 187] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 6. | Kondo S, Hirano S, Ambo Y, Tanaka E, Okushiba S, Morikawa T, Katoh H. Forty consecutive resections of hilar cholangiocarcinoma with no postoperative mortality and no positive ductal margins: results of a prospective study. Ann Surg. 2004;240:95-101. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 228] [Cited by in F6Publishing: 243] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 7. | Endo I, Sugita M, Masunari H, Yoshida K, Takeda K, Sekido H, Togo S, Shimada H. Retroportal hepaticojejunostomy for extended resection of hilar bile ducts. J Gastrointest Surg. 2008;12:962-965. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Hemming AW, Reed AI, Fujita S, Foley DP, Howard RJ. Surgical management of hilar cholangiocarcinoma. Ann Surg. 2005;241:693-699; discussion 699-702. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 258] [Cited by in F6Publishing: 239] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 9. | Lim JH. Cholangiocarcinoma: morphologic classification according to growth pattern and imaging findings. AJR Am J Roentgenol. 2003;181:819-827. [PubMed] [Cited in This Article: ] |
| 10. | Sasaki R, Takeda Y, Funato O, Nitta H, Kawamura H, Uesugi N, Sugai T, Wakabayashi G, Ohkohchi N. Significance of ductal margin status in patients undergoing surgical resection for extrahepatic cholangiocarcinoma. World J Surg. 2007;31:1788-1796. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 80] [Cited by in F6Publishing: 87] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 11. | Ishiko T, Egawa H, Kasahara M, Nakamura T, Oike F, Kaihara S, Kiuchi T, Uemoto S, Inomata Y, Tanaka K. Duct-to-duct biliary reconstruction in living donor liver transplantation utilizing right lobe graft. Ann Surg. 2002;236:235-240. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 4] [Reference Citation Analysis (0)] |
| 12. | Jabłońska B, Lampe P, Olakowski M, Górka Z, Lekstan A, Gruszka T. Hepaticojejunostomy vs. end-to-end biliary reconstructions in the treatment of iatrogenic bile duct injuries. J Gastrointest Surg. 2009;13:1084-1093. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 37] [Article Influence: 2.5] [Reference Citation Analysis (0)] |