Published online Nov 14, 2012. doi: 10.3748/wjg.v18.i42.6088
Revised: September 20, 2012
Accepted: September 29, 2012
Published online: November 14, 2012
AIM: To compare computed tomography enteroclysis (CTE) vs small intestine contrast ultrasonography (SICUS) for assessing small bowel lesions in Crohn's disease (CD), when using surgical pathology as gold standard.
METHODS: From January 2007 to July 2008, 15 eligible patients undergoing elective resection of the distal ileum and coecum (or right colon) were prospectively enrolled. All patients were under follow-up. The study population included 6 males and 9 females, with a median age of 44 years (range: 18-80 years). Inclusion criteria: (1) certain diagnosis of small bowel requiring elective ileo-colonic resection; (2) age between 18-80 years; (3) elective surgery in our Surgical Unit; and (4) written informed consent. SICUS and CTE were performed ≤ 3 mo before surgery, followed by surgical pathology. The following small bowel lesions were blindly reported by one sonologist, radiologist, surgeon and histolopathologist: disease site, extent, strictures, abscesses, fistulae, small bowel dilation. Comparison between findings at SICUS, CTE, surgical specimens and histological examination was made by assessing the specificity, sensitivity and accuracy of each technique, when using surgical findings as gold standard.
RESULTS: Among the 15 patients enrolled, CTE was not feasible in 2 patients, due to urgent surgery in one patients and to low compliance in the second patient, refusing to perform CTE due to the discomfort related to the naso-jejunal tube. The analysis for comparing CTE vs SICUS findings was therefore performed in 13 out of the 15 CD patients enrolled. Differently from CTE, SICUS was feasible in all the 15 patients enrolled. No complications were observed when using SICUS or CTE. Surgical pathology findings in the tested population included: small bowel stricture in 13 patients, small bowel dilation above ileal stricture in 10 patients, abdominal abscesses in 2 patients, enteric fistulae in 5 patients, lymphnodes enlargement (> 1 cm) in 7 patients and mesenteric enlargement in 9 patients. In order to compare findings by using SICUS, CTE, histology and surgery, characteristics of the small bowel lesions observed in CD each patient were blindly reported in the same form by one gastroenterologist-sonologist, radiologist, surgeon and anatomopathologist. At surgery, lesions related to CD were detected in the distal ileum in all 13 patients, also visualized by both SICUS and CTE in all 13 patients. Ileal lesions > 10 cm length were detected at surgery in all the 13 CD patients, confirmed by SICUS and CTE in the same 12 out of the 13 patients. When using surgical findings as a gold standard, SICUS and CTE showed the exactly same sensitivity, specificity and accuracy for detecting the presence of small bowel fistulae (accuracy 77% for both) and abscesses (accuracy 85% for both). In the tested CD population, SICUS and CTE were also quite comparable in terms of accuracy for detecting the presence of small bowel strictures (92% vs 100%), small bowel fistulae (77% for both) and small bowel dilation (85% vs 82%).
CONCLUSION: In our study population, CTE and the non-invasive and radiation-free SICUS showed a comparable high accuracy for assessing small bowel lesions in CD.
-
Citation: Onali S, Calabrese E, Petruzziello C, Zorzi F, Sica G, Fiori R, Ascolani M, Lolli E, Condino G, Palmieri G, Simonetti G, Pallone F, Biancone L. Small intestine contrast ultrasonography
vs computed tomography enteroclysis for assessing ileal Crohn's disease. World J Gastroenterol 2012; 18(42): 6088-6095 - URL: https://www.wjgnet.com/1007-9327/full/v18/i42/6088.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i42.6088
Accurate assessment of the lesions is mandatory for a proper pre-operative evaluation in Crohn’s disease (CD). Diagnostic imaging of the small bowel traditionally included the small bowel follow through (SBFT) or small bowel enteroclysis[1]. A comparable accuracy for assessing small bowel lesions in CD has been shown in referral centres[2]. More recently, magnetic resonance enterography (MRE) and computed tomography enterography or enteroclysis (CTE) showed to accurately assess the presence, site and extent of small bowel lesions in CD, including stenosis, bowel dilation above stenosis and accurate measurement of the lumen diameter[3-6]. These techniques also provide detailed extraluminal findings, including the bowel wall thickness (BWT), fistulas, abscesses and phlegmons not detected by barium studies[7-9]. For these reasons, MRE and CTE currently represent the standard techniques for assessing small bowel lesions in CD[10]. The major limit of CTE is represented by the high radiation exposure for the patient[5-11]. However, CTE has a greater availability and is less time-consuming than MRE[10]. Therefore, as CTE and MRE show a comparable sensitivity for assessing small bowel lesions in CD, their use is also related to the local feasibility and availability of an experienced radiologist[10].
Transabdominal ultrasonography also has been proposed for detecting small bowel lesions in patients with suspected or known CD, showing a sensitivity and specificity of 67%-84% and 81%-95%, respectively[12-14]. The use of oral contrast significantly increases the sensitivity of ultrasonography for assessing small bowel lesions in CD (by more than 95%)[10,15-19]. In particular, small intestine contrast ultrasonography (SICUS) performed by an experienced sonographer may visualize both established CD lesions (i.e., stenosis with possible pre-stenotic dilation) and minor changes of the small bowel[10,15-20]. In experienced hands, SICUS may detect lesions in suspected small bowel diseases with a high (> 95%) sensitivity and specificity, when compared with SBFT and enema[10,15-19]. The use of SICUS has also been proposed in the follow-up of CD patients after ileo-colonic resection, in order to avoid radiation exposure or the more invasive ileocolonoscopy[19].
To our knowledge, only one retrospective study compared CTE and surgical pathology findings in patients with small bowel CD[21]. A detailed information of the small bowel lesions is mandatory before elective surgery in CD[10]. Moreover, surgical indication in subgroup of patients with small bowel CD may also be related to characteristics of the lesions, including abscesses, marked lumen narrowing and/or strictures with prestenotic dilation. On the basis of these observations, in a prospective longitudinal study, we aimed to compare the sensitivity, specificity and accuracy of SICUS vs CTE for assessing the presence of small bowel lesions in patients with CD undergoing elective ileo-colonic resection, when using surgical pathology findings as a gold standard.
From January 2007 to July 2008, 18 eligible patients undergoing elective resection of the distal ileum and coecum (or right colon) with ileo-colonic anastomosis were enrolled. Among these 18 patients, there were 15 patients with ileal CD (8 males, median age 44 years, range: 19-73 years) and, as a control group, 3 patients (2 males, mean age 69 years, range: 60-77 years), requiring ileal resection due to small bowel duplication, carcinoid or ischemic enteritis. All patients were under regular follow-up in our unit.
Inclusion criteria included: (1) Patients with a certain diagnosis of small bowel diseases including CD or other non-inflammatory bowel disease (IBD) related conditions, requiring elective ileo-colonic resection; (2) age between 18-80 years; (3) elective surgery in our Referral Surgical Unit; and (4) written informed consent.
Exclusion criteria included: (1) Low compliance to perform both SICUS and CTE, including the introduction of a naso-gastric tube; (2) patients requiring urgent surgery; (3) obesity (body mass index > 30) not allowing a proper assessment by SICUS; and (4) allergy to contrast agents. In patients with CD, the diagnosis was made according to standard clinical, endoscopic and radiological criteria[10]. Clinical characteristics of each of the 16 patients studied are summarized in Table 1.
| Disease | Sex | Age(yr) | Surgical indication | Lesions extent (cm) | CD pattern |
| CD | M | 39 | Sub-obstructions | 30 | Fibrostricturing |
| CD | F | 19 | Abscess | 20 | Fistulizing |
| CD | F | 49 | Sub-obstructions | 30 | Fibrostricturing |
| CD | M | 38 | Abscess | 21 | Fibrostricturing |
| CD | F | 73 | Sub-obstructions | 40 | Fibrostricturing |
| CD | F | 33 | Sub-obstructions | 25 | Fibrostricturing |
| CD | F | 57 | Sub-obstructions | 30 | Fibrostricturing |
| CD | M | 31 | Abscess | 15 | Fistulizing |
| CD | F | 49 | Sub-obstructions | 35 | Fibrostricturing |
| CD | M | 41 | Sub-obstructions | 20 | Fibrostricturing |
| CD | M | 45 | Sub-obstructions | 15 | Fibrostricturing |
| CD | M | 30 | Sub-obstructions | 40 | Fibrostricturing |
| CD | M | 30 | Sub-obstructions | 35 | Fibrostricturing |
| Small bowel duplication | M | 60 | Sub-obstructions | 20 | NA |
| Ischemic enteritis | M | 69 | Abdominal pain | 10 | NA |
| Small bowel carcinoid | F | 77 | Diarrhoea, weight loss | 35 | NA |
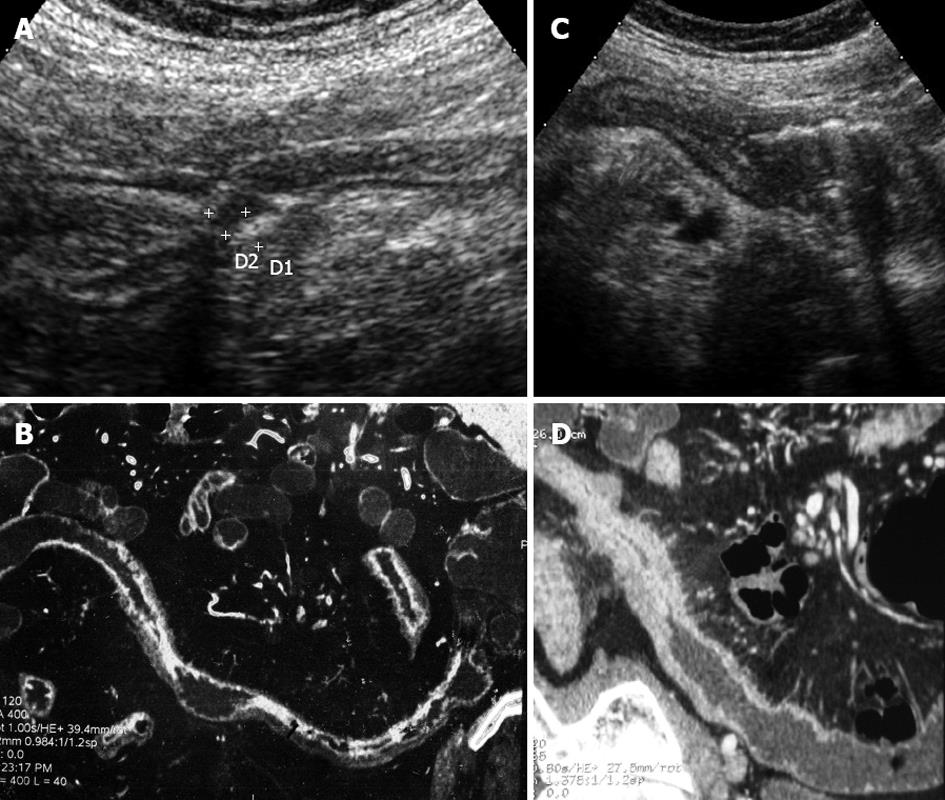
From January 2007 to July 2008, all patients fulfilling the inclusion criteria and requiring elective ileo-colonic resection in our Unit due to small bowel CD were prospectively enrolled. In all patients, ileal lesions were assessed by using both SICUS and CTE within 3 mo before surgery, followed by surgical pathology findings used as a gold standard. Histological assessment of the surgical specimen was performed. In order to compare findings by using SICUS, CTE, histology and surgery, characteristics of the small bowel lesions were blindly reported in the same form by one gastroenterologist-sonologist (Calabrese E), radiologist (Fiori R), surgeon (Simonetti G) and anatomopathologist (Palmieri G). The following parameters detailing the characteristics of the small bowel lesions were blindly reported by each specialist: site of the lesions (ileum, ileum-colon, colon, others), extent of the lesions (< 10 cm vs > 10 cm), strictures (yes/no, number), fistulae (yes/no, number), abscesses (yes/no, number), bowel dilation above strictures (yes/no), lymphnodes enlargement > 1 cm (yes/no, number), mesenteric enlargement (yes/no) (Figure 1).
CTE was performed by one experienced radiologist unaware of SICUS findings, from the Department of Diagnostic Imaging from our university, as previously described[22]. Colonic cleaning was performed the day before CTE by using polyethylen glycole (PEG) 4000 solution. A 20G needle was placed in the antecubital vein and an 8-F naso-jejunal catheter with a Teflon-covered guide wire was positioned under fluoroscopic guidance (Guerbetm Guerbet GmbH D65838, Sulzbach/Ts) and the distal tip was located in the distal duodenum. The patient was then taken into CT room and contrast material (1500 mL of PEG) was administered manually with 60-mL syringes, with a continuous injection rate of 150 mL/min followed by a flow rate of 200 mL/min until the maximum tolerance of the patient. Before the examination, a smooth muscle relaxant (N butyl-scopolamine) was administered. CTE was performed by a 64-slice multidetector (LightSpeed VCT, General Electric Medical System, Milwaukee, WI, United States). After PEG infusion, CT scan was performed before and after the administration of i.v., iodinated contrast material. The contrast-enhanced study was acquired 70 s after the administration of contrast material (Ultravist 370, Schering AG, Berlin, Germany) with a “double-bolus” technique (a first bolus of 60 cc at a flow rate of 1.5 mL/s and a second bolus of 80 cc at a flow rate of 2.0 mL/s).
SICUS was performed as previously described[15,18,19]. In particular, SICUS was performed after the ingestion of 375 mL (range: 250-500 mL) of oral contrast solution consisting of PEG (Promefarm, Milano, Italy), by using a convex transducer (frequency 3.5-5 MHz) and then with a high frequency linear-array transducer (5-12 MHz) (Hitachi, EUB 6500, Japan). All procedures were performed by the same expert EC (> 2000 examinations).
The following findings were considered compatible with CD[16,18,19]: (1) increased BWT (> 3 mm); (2) “stiff loop”, identified by the presence of small bowel loop, with increased BWT not distended by contrast solution; (3) small bowel dilation, defined as a lumen diameter > 2.5 cm; (4) bowel stricture defined as lumen diameter < 1 cm, measured at the level of maximally distended loop, independently of the presence of pre-stenotic dilation; (5) fistulae defined as hypoechoic tract with or without hyperechoic content; (6) mesenteric enlargement and/or masses; (7) lymphnodes enlargement (> 1 cm); and (8) abscesses identified as roundish anechoic lesions, with an irregular wall, often presenting internal echoes and posterior echo enhancement.
At time of intestinal resection, one single GS filled up the above reported form in order to assess the small bowel lesions. Findings at surgery were considered as the gold standard for assessing the small bowel lesions described by SICUS and CTE. The surgical specimen was fixed in formalin for histological examination.
The surgical specimen was examined by the one single GP unaware of previous findings at SICUS, CTE and surgery. At this purpose, routine hematoxylin and eosin staining was performed and the GP filled up the same form used by the sonographist, radiologist and surgeon.
All results were expressed as median and range. Comparison between findings at SICUS, CTE, surgical specimens and histological examination was made by assessing the specificity, sensitivity and accuracy of each technique, when using surgical findings as a gold standard.
From January 2007 to July 2008, 15 CD patients undergoing elective ileo-colonic resection and fulfilling the inclusion criteria were prospectively enrolled. Among these 15 patients, 2 CD patients performed SICUS but were not able to perform CTE, as one patient required “urgent surgery”, and the second patient refused to perform CTE due to the discomfort related to the naso-jejunal tube. Therefore, among the initial 15 patients eligible for the study, only 13 patients were studied by both SICUS and CTE and were therefore considered for the analysis. No side effects were reported after SICUS and CTE procedures.
Among the 13 CD patients considered in the analysis, surgical pathology findings included: small bowel stricture in 13, small bowel dilation above stricture in 10, abdominal abscesses in 2, fistulae in 5 (associated with abscess in 2), lymphnodes enlargement (> 1 cm) in 7 and mesenteric enlargement in 9 patients (Table 2).
| Characteristics | Surgery | SICUS | CTE | Histology |
| CD site | ||||
| Ileum | 8/13 | 10/131 | 10/13 | 8/13 |
| Ileum-colon | 5/13 | 3/13 | 3/13 | 5/13 |
| CD extent (cm) | ||||
| < 10 | 0/13 | 12/13 | 12/13 | 9/13 |
| ≥ 10 | 13/13 | 1/13 | 1/13 | 4/13 |
| Strictures | ||||
| Yes | 13/13 | 12/13 | 13/13 | 13/13 |
| No | 0/13 | 1/13 | 0/13 | 0/13 |
| Dilation | ||||
| Yes | 10/13 | 10/13 | 11/13 | 5/13 |
| No | 0/13 | 0/13 | 2/13 | 8/13 |
| Fistulae | ||||
| Yes | 5/13 | 6/13 | 4/13 | 6/13 |
| No | 8/13 | 7/13 | 9/13 | 7/13 |
| Abscesses | ||||
| Yes | 3/13 | 5/13 | 3/13 | 4/13 |
| No | 11/13 | 8/13 | 10/13 | 9/13 |
Site of the lesions: At surgery, lesions were detected in the distal ileum in all 13 patients, and also in the right colon in 5. Both SICUS and CTE also visualized ileal lesions in all 13 patients, while concomitant lesions in the right colon were detected in 3 out of the 5 patients by both SICUS and CTE (including the same patients in 2 cases) (Table 2). Histological findings were comparable to surgery in all CD patients.
Extent of the small bowel lesions: In CD group (Table 2), histology detected ileal lesions of > 10 cm length in only 9 patients.
Small bowel strictures: Ileal strictures were detected at surgery in all 13 CD patients. Comparable findings were detected by using CTE and histology, while no strictures were detected in one CD patient by using SICUS (Table 2).
Bowel dilation above strictures: Dilation above ileal strictures was detected by both surgery and SICUS in 10/13 CD patients, by CTE in 11/13 patients and by histology in 5/13 patients (Table 2). However, discrepant findings vs surgery were observed by using SICUS in 4/13 CD (dilation not detected in 2; dilation detected only by SICUS in 2), by using CTE in 5/13 CD (dilation not detected in 2; dilation detected only by CTE in 3) and by histology in 5/13 patients (dilation not detected in 5, discrepant findings vs surgery but comparable with SICUS in 2 and with CTE in 1) (Table 2). In the same 2 CD patients, both SICUS and CTE concordantly reported dilation above strictures not detected at surgery. Findings at CTE and SICUS were comparable in only 8/13 patients, as dilation was detected only by SICUS in 2 (confirmed at surgery) and only by CTE in 3 CD patients (confirmed at surgery in 2).
Fistulae: The presence of enteric fistulae were detected in 5 out of the 13 CD patients at surgery, in 6 patients when using SICUS, in 4 patients by using CTE, while histology reported the presence of fistulae in 6 CD patients (Table 2). Findings different from surgery were detected by SICUS in 3/13 patients (fistulae detected by SICUS and not at surgery in 2 patients; fistulae detected at surgery and not by SICUS in 1 patient) by CTE in 4/13 patients (fistulae detected only by CTE in 2; detected only at surgery in 2); and by histology in 3/13 patients (fistulae detected by histology and not at surgery in 2, and detected at surgery and not by histology in 1). In 3 patients, SICUS and CTE concordantly reported enteric fistulae not confirmed at surgery (detected histologically in 2). When comparing SICUS vs CTE, the presence of fistulae was concordantly detected in 9/13 patients, while fistulae were detected only by SICUS in 1 CD patient.
Abscesses: Abdominal abscesses were detected at surgery in 3/13 CD patients (surgically drained in 1), by using SICUS in 5, by CTE in 3 and by histology in 4 patients (Table 2). Findings different from surgery were reported by SICUS in 2 patients (abscess detected only by SICUS in both), by CTE in 2 patients (abscess detected only by CTE in 1, only at surgery in 1), and by histology in 3 patients (abscess detected only by histology in 2 and only at surgery in 1 patient performing surgical drainage). In one patient, abdominal abscess was detected by both SICUS and CTE but not by surgical pathology and histology. When comparing SICUS and CTE, the presence of abscesses was concordantly detected in 11 out of the 13 patients, while in 2 patients SICUS only reported the presence of an intestinal abscess (confirmed at surgery in one of them).
When using surgical findings as a gold standard, sensitivity, specificity and accuracy of SICUS and CTE for assessing the presence of stenosis, dilation above stenosis and fistulae are reported in Table 3. As indicated, the two techniques showed the same sensitivity, specificity and accuracy for detecting the presence of small bowel fistulae (accuracy 77% for both) and abscesses (accuracy 85% for both). SICUS and CTE were also quite comparable for detecting the presence of small bowel strictures, fistulae and abscesses. Nevertheless, there was a not significant trend for a higher sensitivity and accuracy of CTE vs SICUS for assessing small bowel strictures (accuracy 100% vs 92%; the observed 0% specificity related to the absence of true negative findings), while SICUS showed a not significantly higher accuracy vs CTE for detecting small bowel dilation (85% vs 82%).
| Parameter | SICUS | CTE | ||||
| Sens. | Spec. | Accuracy | Sens. | Spec. | Accuracy | |
| Strictures | 92 | 0 | 92 | 100 | 0 | 100 |
| (TN 0; TP 12; FN 1; FP 0) | (TN 0; TP 13; FN 0; FP0) | |||||
| Dilation | 100 | 50 | 85 | 78 | 0 | 82 |
| (TN2; TP 9; FN 0; FP2) | (TN 0; TP 7; FN 2; FP 4) | |||||
| Fistulae | 60 | 88 | 77 | 60 | 88 | 77 |
| (TN 7; TP 3; FN 2; FP 1) | (TN 7; TP 3; FN 2; FP 1) | |||||
| Abscesses | 100 | 80 | 85 | 67 | 100 | 85 |
| (TN 8; TP 3; FN 0; FP 2) | (TN 9; TP 2; FN 1; FP 1) | |||||
Appropriate surgical treatment of CD involves an accurate knowledge of the characteristics of the lesions, including the site, extent and possible presence of complications (strictures, dilation above strictures, fistulae, abscesses). The development of a marked bowel dilation above stricture or abscesses may represent indication for surgery[10]. Colonoscopy represents the gold standard technique for assessing colonic lesions, while small bowel lesions were previously assessed by SBFT or small bowel enteroclysis[1,2]. More recently, CTE or MRE represent the gold standard techniques at this purpose[10]. These techniques indeed provide not only an accurate assessment of the presence, site and extent of the lesions, but they also allow the visualization of extraluminal findings related to the disease (i.e., increased BWT, fistulae, abscesses, mesenteric enlargement)[3-9]. The preferential use of CTE vs MRE is related to the feasibility and easy access to these techniques in each IBD referral centre. At this purpose, both appropriate radiologic instruments and an experienced radiologist with specific competence in the field are required[10]. MRE shows the advantage of a radiation-free procedure.
SICUS also has also been recently suggested as a non-invasive technique able to assess, in experienced hands, the presence of small bowel lesions in CD, including the BWT, strictures, bowel dilation, fistulae and abscesses[16,18,21]. Indication for surgery in CD may also be related to the characteristics of the small bowel lesions (i.e., marked dilation above strictures, abscesses). Whether CTE and SICUS provide a comparable definition of the small bowel lesions in CD is currently unknown. On the basis of these observations, in the present study we aimed to compare these 2 techniques in terms of assessment of the small bowel lesions in patients with CD undergoing elective ileo-colonic resection. The use of small bowel capsule endoscopy has also been shown to accurately visualize small bowel lesions in CD[23-25]. However, the use of small bowel capsule endoscopy (SBCE) is limited by the impact risk in patients with intestinal stenosis[23-25]. In our study, according to the inclusion criteria, all CD patients were undergoing elective ileo-colonic resection. Therefore, all the enrolled CD patients were by definition at high risk of SBCE impact, related to severe lesions requiring surgical resection. For this reason, this useful technique able to visualize the entire small bowel was not feasible in the present study aimed to compare findings using CTE vs SICUS. A comparative estimate of the costs of the current techniques able to assess small bowel lesions, including not only CTE and SICUS, but also MRE and SBCE, could be of great interest. However, these cost may greatly differ in different hospitals, thus limiting the usefulness of this estimate. Nevertheless, among techniques tested in the present study, it appears conceivable to consider CTE more expensive than SICUS.
Limitations of the study include the limited number of tested patients (n = 15), related to difficulties to perform 2 consecutive small bowel examinations in patients with active CD undergoing surgical resection. Additional limitation include the absence of a control group, as the purpose of the study was to compare the accuracy of SICUS vs CTE for assessing small bowel lesions in patients with a certain diagnosis of CD. Results from our limited series suggest that SICUS and CTE are quite comparable techniques at this purpose. However, while the accuracy of these two procedures for assessing the presence of strictures was quite comparable, SICUS showed a slightly higher accuracy for detecting the presence of dilation above strictures. In our series, CTE and SICUS were absolutely comparable for assessing the presence of fistulae and abscesses. SICUS is not feasible in obese patients, due to inaccurate findings and may be less accurate than CTE for visualizing lesions in the deeper layer of the abdominal cavity[12]. Nevertheless, it seems relevant to note that CTE could not be performed in 2 out of the 17 enrolled CD patients (11.7%) already studied by SICUS. These 2 patients were therefore excluded from the analysis, as CTE could not be performed due to low compliance in one patient refusing the naso-jejunal tube and to need of urgent surgery in the second patient. These observations therefore support that CTE may not be performed in a relatively high proportion of patients undergoing ileo-colonic resection for CD.
Nevertheless, differently form SICUS, CTE is an invasive procedure associated with a high radiation exposure for the patient[11]. This issue assumes particular relevance when considering that small bowel assessment before surgery for CD is most often required in young patients already performing other diagnostic radiological procedures and treated with immunomodulatory drugs[26-29]. These observations, together with findings from our study therefore suggest that in referral IBD centres with a feasible experienced ultrasonographer, SICUS may represent the procedure of choice when compared with CTE, for assessing small bowel lesions in patients undergoing elective ileo-colonic resection for CD.
Magnetic resonance enterography (MRE) and computed tomography enterography or enteroclysis (CTE) accurately assess small bowel lesions in Crohn's disease (CD), representing the standard techniques at this purpose. The major limit of CTE is represented by the high radiation exposure for the patient. Recently, small intestine contrast ultrasonography (SICUS) performed by an experienced sonographer has been shown to visualize CD lesions of the small bowel. These findings suggest that SICUS may be used for assessing CD lesions, although comparison with CTE when using surgical pathology as standard is unknown.
Proper follow up of CD patients includes the assessment of the lesions in order to choice appropriate treatment strategies and the presence of complications. In this study, the authors compared the sensitivity, specificity and accuracy of SICUS vs CTE for assessing the presence of small bowel lesions in patients with CD undergoing elective ileo-colonic resection, when using surgical pathology findings as a gold standard.
Small bowel lesions in CD may be accurately detected by CTE or MRE. However, the use of CTE is associated with a high radiation exposure, while MRE shows a low availability. Moreover, the need of intestinal preparation, insertion of the naso-gastric tube may limit the use of both techniques. The authors performed a prospective longitudinal study in patients undergoing elective surgery, aimed to assess the accuracy of SICUS vs CTE for assessing small bowel lesions in CD, when using surgical pathology as gold standard.
This study provides the first evidence that SICUS and CTE show a comparable high accuracy for assessing small bowel lesions in CD. These results suggest that the radiation-free, non-invasive SICUS performed by an experienced sonographer may be used for assessing small bowel lesions in patients with CD.
CTE and MRE may not be performed in patients with low compliance. Results from this study support that, differently from CTE, SICUS may be performed in all CD patients undergoing elective surgery. As SICUS and CTE showed a comparable high accuracy for assessing small bowel lesions in CD, the non-invasive SICUS should be used at this purpose in referral centres provided of an experienced and available sonologist.
Peer reviewers: Dr. Alberto Tommasini, MD, Professor, Laboratory of Immunopathology, Institute for Maternal and Child Health, IRCCS Burlo Garofolo, Via dell’Istria 65/1, 34137 Trieste, Italy; Limas Kupcinskas, Professor, Department of Gastroenterology, Kaunas University of Medicine, Mickeviciaus 9, LT44307 Kaunas, Lithuania; Yu-Yuan Li, Professor, Department of Gastroenterology, First Municipal People’s Hospital of Guangzhou, 1 Panfu Road, Guangzhou 510180, Guangdong Province, China
S- Editor Gou SX L- Editor A E- Editor Xiong L
| 1. | Goldberg HI, Caruthers SB, Nelson JA, Singleton JW. Radiographic findings of the National Cooperative Crohn's Disease Study. Gastroenterology. 1979;77:925-937. [PubMed] [Cited in This Article: ] |
| 2. | Bernstein CN, Boult IF, Greenberg HM, van der Putten W, Duffy G, Grahame GR. A prospective randomized comparison between small bowel enteroclysis and small bowel follow-through in Crohn's disease. Gastroenterology. 1997;113:390-398. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 83] [Cited by in F6Publishing: 87] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 3. | Koh DM, Miao Y, Chinn RJ, Amin Z, Zeegen R, Westaby D, Healy JC. MR imaging evaluation of the activity of Crohn's disease. AJR Am J Roentgenol. 2001;177:1325-1332. [PubMed] [Cited in This Article: ] |
| 4. | Wold PB, Fletcher JG, Johnson CD, Sandborn WJ. Assessment of small bowel Crohn disease: noninvasive peroral CT enterography compared with other imaging methods and endoscopy--feasibility study. Radiology. 2003;229:275-281. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 255] [Cited by in F6Publishing: 263] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 5. | Doerfler OC, Ruppert-Kohlmayr AJ, Reittner P, Hinterleitner T, Petritsch W, Szolar DH. Helical CT of the small bowel with an alternative oral contrast material in patients with Crohn disease. Abdom Imaging. 2003;28:313-318. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 40] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 6. | Hassan C, Cerro P, Zullo A, Spina C, Morini S. Computed tomography enteroclysis in comparison with ileoscopy in patients with Crohn's disease. Int J Colorectal Dis. 2003;18:121-125. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 55] [Cited by in F6Publishing: 57] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 7. | Rimola J, Rodriguez S, García-Bosch O, Ordás I, Ayala E, Aceituno M, Pellisé M, Ayuso C, Ricart E, Donoso L. Magnetic resonance for assessment of disease activity and severity in ileocolonic Crohn's disease. Gut. 2009;58:1113-1120. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 508] [Cited by in F6Publishing: 478] [Article Influence: 31.9] [Reference Citation Analysis (0)] |
| 8. | Albert JG, Martiny F, Krummenerl A, Stock K, Lesske J, Göbel CM, Lotterer E, Nietsch HH, Behrmann C, Fleig WE. Diagnosis of small bowel Crohn's disease: a prospective comparison of capsule endoscopy with magnetic resonance imaging and fluoroscopic enteroclysis. Gut. 2005;54:1721-1727. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 225] [Cited by in F6Publishing: 188] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 9. | Sailer J, Peloschek P, Schober E, Schima W, Reinisch W, Vogelsang H, Wunderbaldinger P, Turetschek K. Diagnostic value of CT enteroclysis compared with conventional enteroclysis in patients with Crohn's disease. AJR Am J Roentgenol. 2005;185:1575-1581. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 56] [Cited by in F6Publishing: 61] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 10. | Van Assche G, Dignass A, Panes J, Beaugerie L, Karagiannis J, Allez M, Ochsenkühn T, Orchard T, Rogler G, Louis E. The second European evidence-based Consensus on the diagnosis and management of Crohn's disease: Definitions and diagnosis. J Crohns Colitis. 2010;4:7-27. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 818] [Cited by in F6Publishing: 776] [Article Influence: 55.4] [Reference Citation Analysis (0)] |
| 11. | Brenner DJ, Hall EJ. Computed tomography--an increasing source of radiation exposure. N Engl J Med. 2007;357:2277-2284. [PubMed] [Cited in This Article: ] |
| 12. | Fraquelli M, Colli A, Casazza G, Paggi S, Colucci A, Massironi S, Duca P, Conte D. Role of US in detection of Crohn disease: meta-analysis. Radiology. 2005;236:95-101. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 225] [Cited by in F6Publishing: 196] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 13. | Sonnenberg A, Erckenbrecht J, Peter P, Niederau C. Detection of Crohn's disease by ultrasound. Gastroenterology. 1982;83:430-434. [PubMed] [Cited in This Article: ] |
| 14. | Limberg B, Osswald B. Diagnosis and differential diagnosis of ulcerative colitis and Crohn's disease by hydrocolonic sonography. Am J Gastroenterol. 1994;89:1051-1057. [PubMed] [Cited in This Article: ] |
| 15. | Parente F, Greco S, Molteni M, Anderloni A, Sampietro GM, Danelli PG, Bianco R, Gallus S, Bianchi Porro G. Oral contrast enhanced bowel ultrasonography in the assessment of small intestine Crohn's disease. A prospective comparison with conventional ultrasound, x ray studies, and ileocolonoscopy. Gut. 2004;53:1652-1657. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 150] [Cited by in F6Publishing: 145] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 16. | Calabrese E, La Seta F, Buccellato A, Virdone R, Pallotta N, Corazziari E, Cottone M. Crohn's disease: a comparative prospective study of transabdominal ultrasonography, small intestine contrast ultrasonography, and small bowel enema. Inflamm Bowel Dis. 2005;11:139-145. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 95] [Cited by in F6Publishing: 91] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 17. | Pallotta N, Tomei E, Viscido A, Calabrese E, Marcheggiano A, Caprilli R, Corazziari E. Small intestine contrast ultrasonography: an alternative to radiology in the assessment of small bowel disease. Inflamm Bowel Dis. 2005;11:146-153. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 85] [Cited by in F6Publishing: 72] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 18. | Biancone L, Calabrese E, Petruzziello C, Onali S, Caruso A, Palmieri G, Sica GS, Pallone F. Wireless capsule endoscopy and small intestine contrast ultrasonography in recurrence of Crohn's disease. Inflamm Bowel Dis. 2007;13:1256-1265. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 89] [Cited by in F6Publishing: 71] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 19. | Calabrese E, Petruzziello C, Onali S, Condino G, Zorzi F, Pallone F, Biancone L. Severity of postoperative recurrence in Crohn's disease: correlation between endoscopic and sonographic findings. Inflamm Bowel Dis. 2009;15:1635-1642. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 99] [Cited by in F6Publishing: 79] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 20. | Calabrese E, Zorzi F, Zuzzi S, Ooka S, Onali S, Petruzziello C, Lasinio GJ, Biancone L, Rossi C, Pallone F. Development of a numerical index quantitating small bowel damage as detected by ultrasonography in Crohn's disease. J Crohns Colitis. 2012;6:852-860. [PubMed] [Cited in This Article: ] |
| 21. | Chiorean MV, Sandrasegaran K, Saxena R, Maglinte DD, Nakeeb A, Johnson CS. Correlation of CT enteroclysis with surgical pathology in Crohn's disease. Am J Gastroenterol. 2007;102:2541-2550. [PubMed] [DOI] [Cited in This Article: ] |
| 22. | Fiori R, Viarani S, Petrella MC, Vanni S, Simonetti G. Intestinal duplication in an adult patient diagnosed by multidetector computed tomography enteroclysis: report of a case. Abdom Imaging. 2009;34:726-730. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 23. | Pallotta N, Giovannone M, Pezzotti P, Gigliozzi A, Barberani F, Piacentino D, Hassan NA, Vincoli G, Tosoni M, Covotta A. Ultrasonographic detection and assessment of the severity of Crohn's disease recurrence after ileal resection. BMC Gastroenterol. 2010;10:69. [PubMed] [Cited in This Article: ] |
| 24. | Petruzziello C, Onali S, Calabrese E, Zorzi F, Ascolani M, Condino G, Lolli E, Naccarato P, Pallone F, Biancone L. Wireless capsule endoscopy and proximal small bowel lesions in Crohn's disease. World J Gastroenterol. 2010;16:3299-3304. [PubMed] [Cited in This Article: ] |
| 25. | Dionisio PM, Gurudu SR, Leighton JA, Leontiadis GI, Fleischer DE, Hara AK, Heigh RI, Shiff AD, Sharma VK. Capsule endoscopy has a significantly higher diagnostic yield in patients with suspected and established small-bowel Crohn's disease: a meta-analysis. Am J Gastroenterol. 2010;105:1240-128; quiz 1249. [PubMed] [Cited in This Article: ] |
| 26. | Desmond AN, O'Regan K, Curran C, McWilliams S, Fitzgerald T, Maher MM, Shanahan F. Crohn's disease: factors associated with exposure to high levels of diagnostic radiation. Gut. 2008;57:1524-1529. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 279] [Cited by in F6Publishing: 256] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 27. | Guimarães LS, Fidler JL, Fletcher JG, Bruining DH, Huprich JE, Siddiki H, Sandborn WJ, Loftus EV, Pardi DS, McCollough CH. Assessment of appropriateness of indications for CT enterography in younger patients. Inflamm Bowel Dis. 2010;16:226-232. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 35] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 28. | Zorzi F, Zuzzi S, Onali S, Calabrese E, Condino G, Petruzziello C, Ascolani M, Pallone F, Biancone L. Efficacy and safety of infliximab and adalimumab in Crohn's disease: a single centre study. Aliment Pharmacol Ther. 2012;35:1397-1407. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 45] [Cited by in F6Publishing: 33] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 29. | Dignass A, Van Assche G, Lindsay JO, Lémann M, Söderholm J, Colombel JF, Danese S, D'Hoore A, Gassull M, Gomollón F. The second European evidence-based Consensus on the diagnosis and management of Crohn's disease: Current management. J Crohns Colitis. 2010;4:28-62. [PubMed] [Cited in This Article: ] |