Published online Oct 28, 2012. doi: 10.3748/wjg.v18.i40.5702
Revised: June 7, 2012
Accepted: August 4, 2012
Published online: October 28, 2012
AIM: To evaluate the efficacy and safety of traditional Chinese surgical treatment for anal fistulae with secondary tracks and abscess.
METHODS: Sixty patients with intersphincteric or transsphincteric anal fistulas with secondary tracks and abscess were randomly divided into study group [suture dragging combined with pad compression (SDPC)] and control group [fistulotomy (FSLT)]. In the SDPC group, the internal opening was excised and incisions at external openings were made for drainage. Silk sutures were put through every two incisions and knotted in loose state. The suture dragging process started from the first day after surgery and the pad compression process started when all sutures were removed as wound tissue became fresh and without discharge. In the FSLT group, the internal opening and all tracts were laid open and cleaned by normal saline postoperatively till all wounds healed. The time of healing, postoperative pain score (visual analogue scale), recurrence rate, patient satisfaction, incontinence evaluation and anorectal manometry before and after the treatment were examined.
RESULTS: There were no significant differences between the two groups regarding age, gender and fistulae type. The time of healing was significantly shorter (24.33 d in SDPC vs 31.57 d in FSLT, P < 0.01) and the patient satisfaction score at 1 mo postoperative follow-up was significantly higher in the SDPC group (4.07 in SDPC vs 3.37 in FSLT, P < 0.05). The mean maximal postoperative pain scores were 5.83 ± 2.5 in SDPC vs 6.37 ± 2.33 in FSLT and the recurrence rates were 3.33 in SDPC vs 0 in FSLT. None of the patients in the two groups experienced liquid and solid fecal incontinence and lifestyle alteration postoperatively. The Wexner score after treatment of intersphincter fistulae were 0.17 ± 0.41 in SDPC vs 0.40 ± 0.89 in FSLT and trans-sphincter fistulae were 0.13 ± 0.45 in SDPC vs 0.56 ± 1.35 in FSLT. The maximal squeeze pressure and resting pressure declined after treatment in both groups. The maximal anal squeeze pressures after treatment were reduced (23.17 ± 3.73 Kpa in SDPC vs 22.74 ± 4.47 Kpa in FSLT) and so did the resting pressures (12.36 ± 2.15 Kpa in SDPC vs 11.71 ± 1.87 Kpa in FSLT), but there were neither significant differences between the two groups and nor significant differences before or after treatment.
CONCLUSION: Traditional Chinese surgical treatment SDPC for anal fistulae with secondary tracks and abscess is safe, effective and less invasive.
- Citation: Wang C, Lu JG, Cao YQ, Yao YB, Guo XT, Yin HQ. Traditional Chinese surgical treatment for anal fistulae with secondary tracks and abscess. World J Gastroenterol 2012; 18(40): 5702-5708
- URL: https://www.wjgnet.com/1007-9327/full/v18/i40/5702.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i40.5702
Anal fistulae are common in human beings. Surgery remains one of the most effective therapies. The main objective of surgery for anal fistulae is to eradicate the fistula tract while maintaining anal continence[1]. Fistulotomy (FSLT) and fistulectomy are safe and effective for simple and superficial anal fistulae. When a fistula has secondary tracts or abscess, laying open procedures may have some complications such as longer healing time, larger defects, and higher risk of incontinence[2,3]. In China, many hospitals use traditional Chinese surgical therapies to treat anal fistulae. To some extent, these therapies work well[4-7]. Suture dragging combined with pad compression (SDPC) is a combined dynamic treatment which was invented by Bo-Hua Gu and has been applied to anorectal disease by Jin-Gen Lu since the 1980s[8]. The aim of this study was to evaluate the efficacy and safety of this traditional Chinese surgical treatment SDPC for anal fistulae with secondary tracks and abscess and to compare it with the surgical treatment FSLT in modern medicine.
A total of 60 consecutive patients with intersphincteric or transsphincteric anal fistulae with secondary tracks and abscess were included in the study, who were treated between January 2008 and March 2009 in the department of anorectal surgery, Longhua Hospital affiliated to Shanghai University of Traditional Chinese Medicine, Shanghai, China. This study was approved by the local ethical committee and performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki. Patients with chronic inflammatory bowel disease, dermatitis, diabetes, tumors and pregnant or lactating women were excluded. Informed consent was obtained from all participants after full explanation of the procedure. None of them were dropped out or lost to follow-up after the study.
Preoperative evaluation: Patients were randomly assigned to either the SDPC group or the FSLT group by computer-generated random number. Each group has 30 patients. Clinical evaluation was based on both digital examinations and assessments with perianal and endoanal ultrasonography by an experienced sonographer. All patients were identified to have either intersphincteric or transsphincter anal fistulae with secondary tracts or abscesses. Incontinence evaluation (Wexner score, 0-20) and anorectal manometry (Medtronic Synectics, Sweden) were performed with an 8 channel water-perfused catheter before surgery. Maximal anal squeeze and anal resting pressures were recorded.
Postoperative pain was evaluated using a visual analogue scale (0-10), incontinence evaluation and anorectal manometry were performed when wounds were completely epithelized.
Operative technique: All procedures were carried out by one of two surgeons with significant experience in SDPC and FSLT. Surgeon was told of the intervention one day before surgery. Both groups were operated upon under spinal anaesthesia and in lithotomy or left lateral position. One dose of metronidazole (Shanghai Huazhong Pharmaceutical, Ltd., Shanghai, China) was used intravenously during the operation.
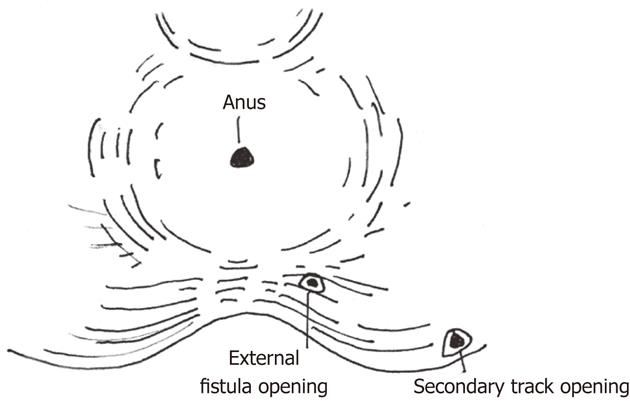
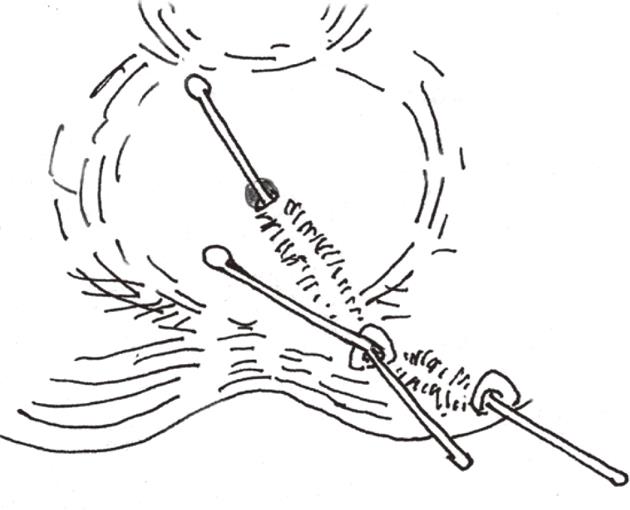
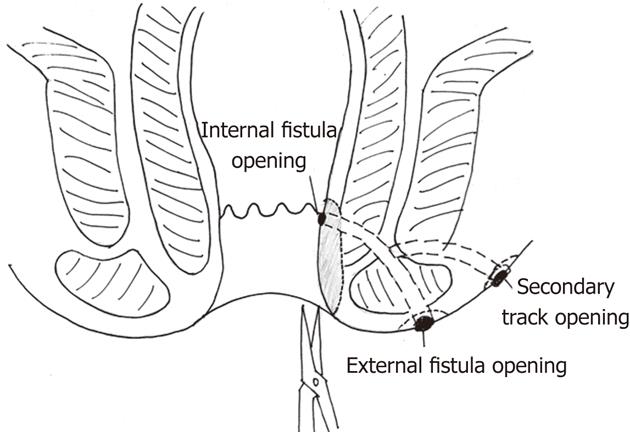
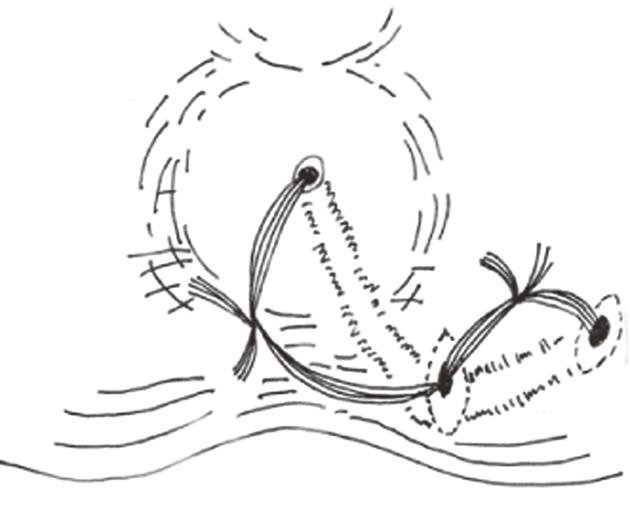
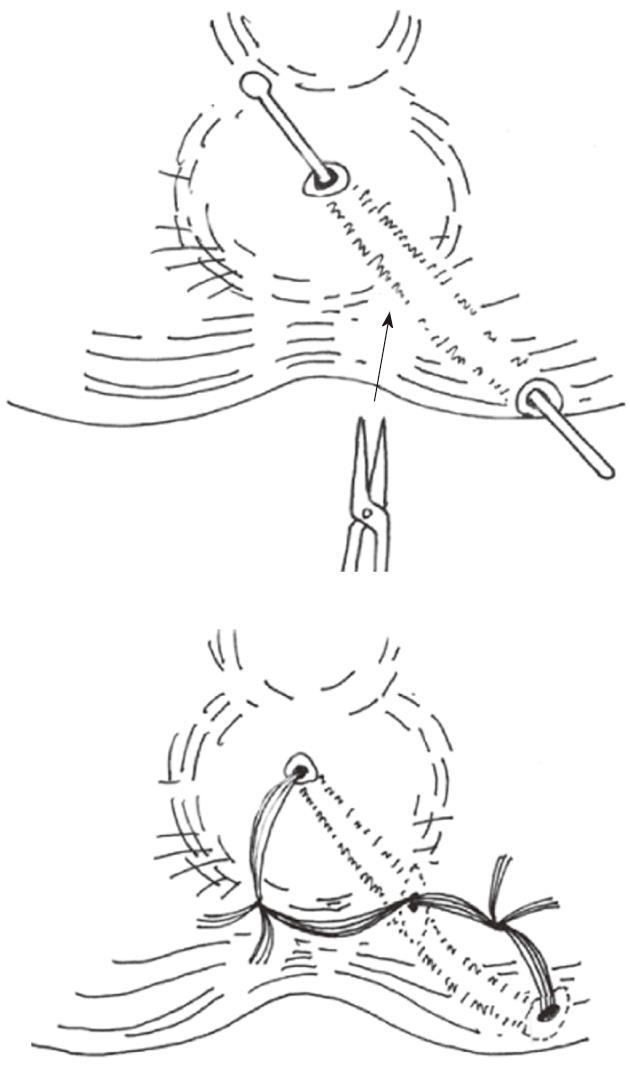
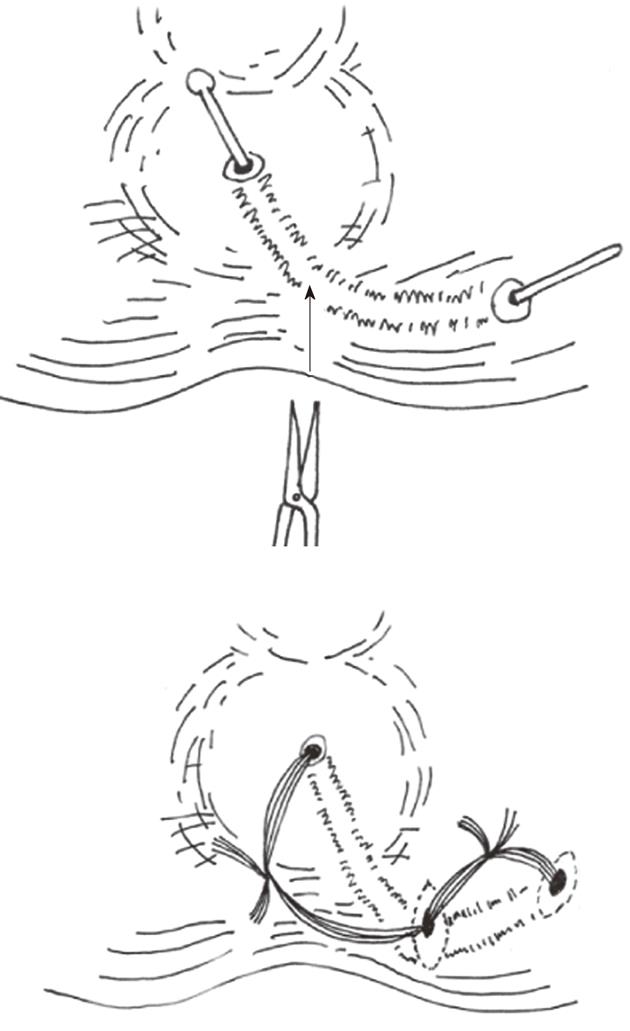
In the SDPC group, internal opening and secondary tracts or abscess were identified by a ball-shape head sliver fistula probe (Figures 1 and 2). The internal opening and inflammatory tissue around were excised with scissors. Mucosa and internal sphincter below the internal opening were laid open and the incision was extended to anal verge for drainage. All secondary tracts and abscesses of intersphincteric fistulae or transsphincteric fistulae were curetted carefully to remove epithelialized and necrotic tissues. Incisions at external openings were made about 1 cm × 0.5 cm for drainage (Figure 3). Then ten silk sutures (4-0, 25 cm length, Shanghai Jinhuan Medical, Ltd., Shanghai, China) were put through every two incisions and knotted in loose state (Figure 4). For complete drainage, one incision was done in the middle of curved (Figure 5) or longer than 5 cm fistulous tract (Figure 6).
In the FSLT group, the internal opening and all tracts were identified with the same ball-shape head sliver fistula probe. The internal opening, extended fistula tracts, abscess and external openings were laid open thoroughly with scissors and curetted carefully. All wounds were left open for drainage.
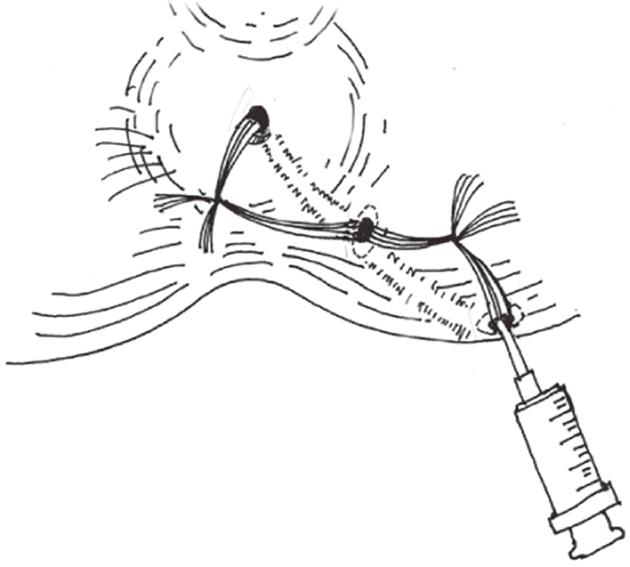
Postoperative care: Metronidazole was administered intravenously for three days postoperatively in both groups. In the SDPC group, dressings were changed by doctors twice a day at 8 am and 4 pm, respectively. The suture dragging process was started from the first day after surgery during dressing change. Wounds and fistulous track cavities were irrigated with normal saline (Figure 7). Part of the silk sutures inside the fistula tract were dragged out and cleansed with normal saline, then turned back into the tract cavity. Usually the fistulous cavity became smaller at 10 d after surgery while the granulation tissue grew, then five sutures were cut and taken away. The residual sutures were removed one by one every 1-2 d afterwards depending on the space of the cavity. When all sutures were removed as wound tissue became fresh and without discharge, the pad compression process was initiated. One dose of lopramide hydrochloride (Xian-Janssen Pharmaceutical, Ltd., Xi’an, China) was given to the patients at the same time. A thick cotton pad was wrapped over the fistulous cavity and fixed with tape. Patients were asked to sit on a flat chair for 30 min, and relax for 10 min. The total time for pad compression was 6 h a day till the cavity healed.
In the FSLT group, dressings were changed by doctors twice a day at 8 am and 4 pm from the first day after surgery. Normal saline was used to clean the wounds until all wounds were completely epithelized. Patients in both groups were discharged when wounds healed. Success was defined by the absence of bleeding, pain, discharge, and subjective symptomatic relief.
Patients were followed up at outpatient clinic at 1 mo after the wounds were completely healed and by telephone at 12 mo after surgery. Patient's satisfaction was assessed in the outpatient clinic at the first follow-up using scores from -5 to +5 (with -5 being dissatisfied and +5 being very satisfied).
Statistical analysis was performed using SPSS for Windows Version 11.5 (SPSS Inc., Chicago, IL, United States). Descriptive statistics for demographic data were employed. Quantitative data were expressed as the mean ± SD, while χ2 test was used for categorical data analysis. The two groups were compared with one-sided t test for analysis. P < 0.05 was considered significant.
The demographic data and outcomes in the two groups are shown in Table 1.
| SDPC (n = 30) | FIST (s = 30) | P value | |
| Age (yr) | 44.25 ± 14.31 | 41.17 ± 17.58 | 0.744 |
| Gender (male/female) | 22/8 | 19/11 | 0.405 |
| Fistulae type | |||
| Intersphincteric | 6 | 5 | 0.739 |
| Trans-sphincteric | 24 | 25 | |
| Secondary tracts | 21 | 23 | 0.559 |
| Secondary abscess | 9 | 7 | |
| Time of healing (d) | 24.33 ± 4.44 | 31.57 ± 5.30 | < 0.001 |
| Postoperative pain scores | 5.83 ± 2.50 | 6.37 ± 2.33 | 0.373 |
| Oral analgesics (n) | 10 | 14 | 0.292 |
| Parenteral analgesics (n) | 0 | 1 | 0.313 |
| Recurrence rate (%) | 3.33 | 0 | 0.313 |
| Incontinence score | |||
| Before treatment | |||
| Intersphincteric | 0.00 ± 0.00 | 0.20 ± 0.45 | 0.148 |
| Trans-sphincteric | 0.08 ± 0.28 | 0.12 ± 0.44 | 0.366 |
| After treatment | |||
| Intersphincteric | 0.17 ± 0.41 | 0.40 ± 0.89 | 0.289 |
| Trans-sphincteric | 0.13 ± 0.45 | 0.56 ± 1.35 | 0.071 |
| Manometry | |||
| Maximal anal squeeze pressure (Kpa) | |||
| Before treatment | 24.73 ± 4.39 | 25.31 ± 3.89 | 0.590 |
| After treatment | 23.17 ± 3.73 | 23.74 ± 4.47 | 0.598 |
| Resting pressure (Kpa) | |||
| Before treatment | 13.16 ± 2.23 | 12.66 ± 2.19 | 0.391 |
| After treatment | 12.36 ± 2.15 | 11.71 ± 1.87 | 0.212 |
| Patient satisfaction | 4.07 ± 0.94 | 3.37 ± 1.45 | 0.031 |
The mean time of healing in the two groups was 24.33 ± 4.44 d and 31.57 ± 5.30 d, respectively. It was significant shorter in the SDPC group than in the FSLT group.
The mean maximal postoperative pain scores were 5.83 ± 2.5 and 6.37 ± 2.33 for the SDPC group and the SDPC group, respectively. Ten (33.33%) patients in the SDPC group used oral analgesics and no patient required additional parenteral analgesics. Fifteen (46.67%) patients in the SDPC group used oral analgesics and one (3.33%) patient received parenteral analgesics due to severe pain.
One male patient in the SDPC group had swelling and discharged at week 3 after operation. He became asymptomatic after surgical drainage. All patients in the SDPC group were healed in one stage.
None of the patients had any incontinence before surgery. Two patients with transphincter fistula in the SDPC group and one with intersphincter and two with transsphincter fistula in the SDPC group used pads to prevent underwear contamination. Postoperatively, no patient in the SDPC group experienced incontinence, but one intersphincter and two transsphincter fistulae patients used pads in the first two weeks after surgery. One female patient in the SDPC group with transsphincter fistula had transient gas incontinence from the third day after surgery. Symptoms of this patient disappeared 4 wk later without any treatment. Another one intersphincter and three transsphincter patients in the SDPC group wore pads in the first two weeks after surgery. The Wexner score after treatment of trans-sphincter fistulae was 0.13 ± 0.45 in the SDPC group and 0.56 ± 1.35 in the FSLT group (P = 0.071). None of the patients in this study experienced any problem with liquid and solid fecal incontinence and lifestyle alteration postoperatively.
The maximal anal squeeze pressures before operation were 24.73 ± 4.39 Kpa in SDPC and 25.31 ± 3.89 Kpa in FSLT, and reduced to 23.17 ± 3.73 Kpa in SDPC and 22.74 ± 4.47 Kpa in FSLT after operation. The resting pressures before operation were 13.16 ± 2.23 Kpa in SDPC and 12.66 ± 2.19 Kpa in FSLT, and reduced to 12.36 ± 2.15 Kpa in SDPC and 11.71 ± 1.87 Kpa in FSLT after operation. Both of the maximal squeeze pressure and resting pressure declined, but there were neither significant differences between the two groups and nor significant differences before or after treatment.
The mean satisfaction score at 1-mo postoperative follow-up for the SDPC group was 5 in ten patients, 4 in fifteen patients, 3 in three patients, 2 in one patient and 1 in one patient. It was 5 in six patients, 4 in ten patients, 3 in nine patients, 2 in two patients, 1 in one patient, 0 in one patient and -1 in one patient in the SDPC group. The mean satisfaction score was significant higher in the SDPC group (4.07 ± 0.94 in SDPC vs 3.37 ± 1.45 in FSLT).
The prevalence rate of anal fistulae is 8.6 cases per 100 000 populations[9]. Surgery is the most effective treatment for cryptoglandular fistula. For intersphincteric and low trans-sphincteric fistula, FSLT is a primary therapy[10]. Though complete FSLT is safe, it usually leads to larger wounds that take longer time to heal[11,12]. Recently, Atkin et al[13] reported that the laying open technique was still a good option for the management of complex anal fistulas. Ninety-six percent of their patients healed and the incidence rates of incontinence for flatus, soft stools and hard stools were low. But patients were unsatisfied with the postoperative complications of this laying open technique such as severe pain, longer healing time and unsightly scar[7]. More and more surgeons begin to seek less invasive therapies such as fibrin glue, sealant, anal fistula plug, endorectal mucosal advancement flap and ligation of intersphincteric fistula tract. Fibrin glue injection is technically easy, but results have been disappointing, with a success rate as low as 16%[14-16]. Similarly, the use of the anal fistula plug is a simple, low-risk but very expensive technique, and the reported success rates range between 29% and 87%[17-19]. Mucosal advancement flaps are technically difficult and associated recurrence rates vary from 2% to 54%[20-22]. Modified setons as cable-tie seton, silastic tube, silk, linen, braided silk, rubber band, and so forth were used to deal with complex or high anal fistula in recent years. However, incontinence still can not be avoided[23,24]. The latest conservative technique is ligation of intersphincteric fistula trac[25,26], but this procedure does not suit for fistula with abscess. Some novel techniques for treating complex fistula as video-assisted anal fistula treatment[27] and fistula laser closure[28], have been proposed. But these techniques need special equipments although the success rates were up to 80%. In this research, we found that the traditional Chinese surgical treatment SDPC can preserve the integrity of anal sphincter musculature involved by fistulous tract or abscess and maintain anal function with less postoperative pain and shorter healing time. This method has been used to treat fistulae and abscess diseases since the 1980s, which includes two processes. The "suture dragging" process refers to that the sutures which are put through the fistulous tracks or abscesses, are dragged by doctors postoperatively during dressing change. This process usually takes place at the first two weeks postoperatively. Suture dragging not only has the same functions of loose seton as mark and drainage, but also can stimulate granulation tissue to grow. The "pad compression" process means use thick pad to cover the wound and ask patients to sit on flat chair to accelerate the adhesion of wound cavity. Appropriate compression is good for tissue adhesion in wounds with deep cavity. In the last decade, some hospitals in China applied SDPC therapy to treat breast fistulae, acute mastitis, cutaneous abscess, anorectal horseshoe abscesses, necrotic fasciitis, pilonidal sinus disease and have obtained good results[29-32].
In this study, we used SDPC therapy to treat secondary tracts and abscess of intersphincteric and low trans-sphincteric fistulae. The SDPC therapy did not produce large wounds; the mean time of healing was reduced to 7 d compared with that of the FSLT. For the SDPC group, the postoperative pain mostly happened at dressing change. This was because some patients felt discomfort when doctor dragged sutures. But for the SDPC group, the postoperative pain was severe during bowel movement by stool evacuation. There was one male patient in the SDPC group complicated with edema and pain due to infection 3 wk after surgery during pad compression treatment. He suffered from diarrhea due to taking unhygienic food and not changing dressing regularly. After meticulous debridement and complete wound irrigation, he remained asymptomatic afterwards. One female patient who had gas incontinence in the SDPC group had a complex trans-sphincteric fistula in which internal opening was at 6 o'clock and external openings at 6 o’clock and 7 o’clock, 1.5 cm and 2 cm from the anal verge respectively. The patient’s symptom disappeared while wounds healed at 4 wk postoperatively. Though FSLT is safe in treating low trans-sphincteric fistula, it may damage part of external sphincter, especially for female patients with complex fistula. The Wexner score of trans-sphincteric fistula patients in the SDPC group was higher than in the SDPC group postoperatively. Maximal squeeze pressure and resting pressure after treatment reduced in both groups. This may be because that FSLT divided partial sphincter when managing the internal opening. But no patient experienced any problem concerning solid and liquid incontinence after treatment in both groups. Manometery confirmed that both therapies were safe. Most of the patients were highly satisfied with SDPC therapy for the advantages of less invasiveness, tiny scar, mild pain, shorter healing time and hospitalization.
Notably, the pattern of medical treatment in China is different from that of the Western countries. Doctors take care of patients' wounds postoperatively and patients can be discharged until their wounds are mostly epithelialized. On the contrary, in most developed countries, the procedures for most benign anorectal conditions are usually performed in outpatient settings, and patients can take care of their wounds themselves after hospital discharge. However, the treatment outcomes are quite good in this research, possibly due to this special pattern of treatment.
However, there are some limitations of this study. First, the sample size was small, and follow-up period was not long enough to assess the recurrence. SDPC therapy for complex trans-sphincteric fistulae is superior to that for intersphincteric fistulae. For intersphincteric fistulous tracks are usually short and laying open of this kind of fistulae is easy and safe. But for longer fistulous tracts and secondary abscesses, the advantages of this traditional Chinese surgical treatment are more apparent. In addition, the SDPC and FSLT are different techniques, it is impossible to be blinded to either surgeons or patients. In the future, we will conduct multi-center randomized controlled trials to compare SDPC with "cutting seton" or FSLT for high and low complex trans-sphincteric and supersphincteric anal fistulae.
As one of the traditional Chinese surgical therapies, the SDPC is successful in the treatment of perianal fistulae and abscesses disease. But the rationale of this treatment remains unclear. Why could dragging threads stimulate granulation tissue growth? When is the best time to remove sutures and start pad compression? What kind of appropriate pressure and duration can accelerate tissue adhesion without ischemia? Only when these questions have been clearly answered, can this traditional Chinese surgical sphincter-saving method be well accepted. More rigorous prospective randomized controlled trials with a larger sample size and longer follow-up are urgently needed.
In conclusion, traditional Chinese surgical treatment SDPC is safe, effective and less invasive. It can be used as an alternative to the treatment of complex anal fistulae.
Surgery is one of the most effective therapies for anal fistulae. More and more surgeons begin to seek less invasive therapies. However, classical procedures such as fistulotomy (FSLT) and fistulectomy, may produce complications such as longer healing time, larger defects, and higher risk of incontinence when dealing with fistulae with secondary tracts or abscess. In China, traditional Chinese surgical method suture dragging combined with pad compression (SDPC) has been used to treat anal fistulae and achieved good results.
The postoperative complications of anal fistulae mostly include high risk of incontinence, severe pain, longer healing time and unsightly scar. Surgeons begin to seek less invasive therapies such as fibrin glue, sealant, anal fistula plug, endorectal mucosal advancement flap and ligation of intersphincteric fistula tract. The hotspot of anal fistula surgery is how to eradicate the fistula tract while maintaining anal continence and improving patient’s quality of life.
There has been few studies about traditional Chinese surgical treatment for fistula diseases. This study reported that the traditional Chinese surgical method is effective and safe compared with the method used in modern medicine. The SDPC used in this study was less invasive with a higher patient’s satisfaction.
The study results suggest that traditional Chinese surgical method SDPC is safe, effective and less invasive. It could be used as an alternative to the treatment of complex anal fistulae.
Traditional Chinese surgical treatment SDPC includes two processes. The "suture dragging" refers to that the sutures which were put through the fistulous tracks or abscess during the operation, are dragged by doctor postoperatively during dressing change. The "pad compression" means use thick pad to cover the wound and ask patients to sit on flat chair to accelerate the adhesion of wound cavity. By this method, surgeons can preserve the integrity of anal sphincter musculature involved in fistulous tract or abscess, and maintain anal function with less postoperative pain and shorter healing time.
The article presents an interesting novel technique to show the Western world another method of treatment. There was a significant shorter time to healing and higher patients’ satisfaction in the study group, without difference in continence or complications. The described technique seems interesting, however it takes a greater deal of postoperative care compared with the traditional FSLT.
Peer reviewers: Benjamin Perakath, Professor, Department of Colorectal Surgery, Christian Medical College, Vellore 632004, India; Dr. Paola De Nardi, Department of Surgery, Scientific Institute San Raffaele Hospital, Via Archimede 32, 20129 Milano, Italy; Dr. Pankaj Garg, Consultant, Department of General Surgery, Fortis Super Speciality Hospital, Panchkula 134112, India
S- Editor Wu X L- Editor Ma JY E- Editor Xiong L
| 1. | Joy HA, Williams JG. The outcome of surgery for complex anal fistula. Colorectal Dis. 2002;4:254-261. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 49] [Cited by in F6Publishing: 52] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 2. | Steele SR, Kumar R, Feingold DL, Rafferty JL, Buie WD. Practice parameters for the management of perianal abscess and fistula-in-ano. Dis Colon Rectum. 2011;54:1465-1474. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 201] [Cited by in F6Publishing: 149] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 3. | Ommer A, Herold A, Berg E, Fürst A, Sailer M, Schiedeck T. Cryptoglandular anal fistulas. Dtsch Arztebl Int. 2011;108:707-713. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 22] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 4. | Ding M, Huang HX, Cao YQ. [Experience of tunnel drainage and thread-drawing therapy for deep perianal abscess: a report of 62 cases]. Zhongxiyi Jiehe Xuebao. 2008;6:1068-1070. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 5. | He CM, Lu JG, Cao YQ, Yao YB. [Design characteristics of clinical surgery trial based on treatment program of tunnel thread-drawing method for anal fistula: a prospective randomized controlled multicenter trial]. Zhongxiyi Jiehe Xuebao. 2009;7:1113-1118. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Xing YL, Yang W, Zheng D. Clinical Observation of therapeutic effect of Countraincision and indwelling with compressed coller in the treatment of high complex anal fistula. Shanghai Zhongyiyao Zazhi. 2008;42:64-65. [Cited in This Article: ] |
| 7. | Wang C, Lu JG. [Comparison of tunnel thread-drawing therapy and fistulectomy therapy for low-complex anal fistula]. Zhongxiyi Jiehe Xuebao. 2007;5:193-194. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 8. | Lu JG, Que HF, Chen HF, Cao YQ, Wang YF, Wang C, Yao YB. [Superiority of thread-dragging therapy in treatment of refractory sinus tracts or fistulae]. Zhongxiyi Jiehe Xuebao. 2008;6:991-994. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Sainio P. Fistula-in-ano in a defined population. Incidence and epidemiological aspects. Ann Chir Gynaecol. 1984;73:219-224. [PubMed] [Cited in This Article: ] |
| 10. | Williams JG, Farrands PA, Williams AB, Taylor BA, Lunniss PJ, Sagar PM, Varma JS, George BD. The treatment of anal fistula: ACPGBI position statement. Colorectal Dis. 2007;9 Suppl 4:18-50. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 130] [Cited by in F6Publishing: 131] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 11. | Practice parameters for treatment of fistula-in-ano--supporting documentation. The Standards Practice Task Force. The American Society of Colon and Rectal Surgeons. Dis Colon Rectum. 1996;39:1363-1372. [PubMed] [Cited in This Article: ] |
| 12. | Sangwan YP, Rosen L, Riether RD, Stasik JJ, Sheets JA, Khubchandani IT. Is simple fistula-in-ano simple? Dis Colon Rectum. 1994;37:885-889. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 99] [Cited by in F6Publishing: 92] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 13. | Atkin GK, Martins J, Tozer P, Ranchod P, Phillips RK. For many high anal fistulas, lay open is still a good option. Tech Coloproctol. 2011;15:143-150. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 62] [Cited by in F6Publishing: 66] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 14. | Sentovich SM. Fibrin glue for all anal fistulas. J Gastrointest Surg. 2001;5:158-161. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 83] [Cited by in F6Publishing: 90] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 15. | Gisbertz SS, Sosef MN, Festen S, Gerhards MF. Treatment of fistulas in ano with fibrin glue. Dig Surg. 2005;22:91-94. [PubMed] [Cited in This Article: ] |
| 16. | Ellis CN, Clark S. Fibrin glue as an adjunct to flap repair of anal fistulas: a randomized, controlled study. Dis Colon Rectum. 2006;49:1736-1740. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 114] [Cited by in F6Publishing: 117] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 17. | Johnson EK, Gaw JU, Armstrong DN. Efficacy of anal fistula plug vs. fibrin glue in closure of anorectal fistulas. Dis Colon Rectum. 2006;49:371-376. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 240] [Cited by in F6Publishing: 247] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 18. | Malik AI, Nelson RL. Surgical management of anal fistulae: a systematic review. Colorectal Dis. 2008;10:420-430. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 104] [Cited by in F6Publishing: 94] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 19. | Wang JY, Garcia-Aguilar J, Sternberg JA, Abel ME, Varma MG. Treatment of transsphincteric anal fistulas: are fistula plugs an acceptable alternative? Dis Colon Rectum. 2009;52:692-697. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 49] [Cited by in F6Publishing: 54] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 20. | Aguilar PS, Plasencia G, Hardy TG, Hartmann RF, Stewart WR. Mucosal advancement in the treatment of anal fistula. Dis Colon Rectum. 1985;28:496-498. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 126] [Cited by in F6Publishing: 111] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 21. | Schouten WR, Zimmerman DD, Briel JW. Transanal advancement flap repair of transsphincteric fistulas. Dis Colon Rectum. 1999;42:1419-1422; discussion 1419-1422. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 201] [Cited by in F6Publishing: 206] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 22. | Sonoda T, Hull T, Piedmonte MR, Fazio VW. Outcomes of primary repair of anorectal and rectovaginal fistulas using the endorectal advancement flap. Dis Colon Rectum. 2002;45:1622-1628. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 286] [Cited by in F6Publishing: 222] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 23. | Memon AA, Murtaza G, Azami R, Zafar H, Chawla T, Laghari AA. Treatment of complex fistula in ano with cable-tie seton: a prospective case series. ISRN Surg. 2011;2011:636952. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 24. | Ritchie RD, Sackier JM, Hodde JP. Incontinence rates after cutting seton treatment for anal fistula. Colorectal Dis. 2009;11:564-571. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 124] [Cited by in F6Publishing: 99] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 25. | Rojanasakul A, Pattanaarun J, Sahakitrungruang C, Tantiphlachiva K. Total anal sphincter saving technique for fistula-in-ano; the ligation of intersphincteric fistula tract. J Med Assoc Thai. 2007;90:581-586. [PubMed] [Cited in This Article: ] |
| 26. | Shanwani A, Nor AM, Amri N. Ligation of the intersphincteric fistula tract (LIFT): a sphincter-saving technique for fistula-in-ano. Dis Colon Rectum. 2010;53:39-42. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 157] [Cited by in F6Publishing: 130] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 27. | Meinero P, Mori L. Video-assisted anal fistula treatment (VAAFT): a novel sphincter-saving procedure for treating complex anal fistulas. Tech Coloproctol. 2011;15:417-422. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 184] [Cited by in F6Publishing: 167] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 28. | Wilhelm A. A new technique for sphincter-preserving anal fistula repair using a novel radial emitting laser probe. Tech Coloproctol. 2011;15:445-449. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 120] [Cited by in F6Publishing: 108] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 29. | He CM, Cao YQ, Lu JG. [Treatment of acute perianal necrotizing fasciitis with integrated traditional Chinese and Western medicine: a report of 9 cases]. Zhongxiyi Jiehe Xuebao. 2005;3:233-234, 237. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 30. | Sun YH, Cao YQ, Lu JG, Huang HX, Guo XT. [Internal opening incision with harmonic scalpel, remaining and tunnel thread-dragging methods in surgical management of posterior horseshoe fistula]. Zhongxiyi Jiehe Xuebao. 2007;5:589-591. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 31. | Lin H. [Tunnel thread-drawing therapy in treating patients with horseshoe-shaped low-position perianal abscess: a randomized controlled trial]. Zhongxiyi Jiehe Xuebao. 2009;7:1119-1122. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 32. | Lu JG, Wang C, Cao YQ, Yao YB. Thread-dragging and pad pressure therapy in traditional Chinese medicine for treatment of pilonidal sinus: a case report. Zhongxiyi Jiehe Xuebao. 2011;9:36-37. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |