Published online Sep 14, 2012. doi: 10.3748/wjg.v18.i34.4798
Revised: April 25, 2012
Accepted: April 27, 2012
Published online: September 14, 2012
We report a rare case of a small-bowel lymphangioma causing massive gastrointestinal (GI) bleeding that we successfully diagnosed and treated using double-balloon enteroscopy (DBE). An 81-year-old woman suffering from repeated GI bleeding of unknown origin underwent a capsule endoscopy at a previous hospital. She was suspected of having bleeding from the jejunum, and was referred to our department for diagnosis and treatment. An oral DBE revealed a 20 mm × 10 mm, regularly surfaced, white to yellowish, elongated, pedunculated jejunal polyp with small erosions at 10 cm distal to the ligament of Treiz. Since no other source of bleeding was identified by endoscopy in the deep jejunum, an endoscopic polypectomy (EP) was performed for this lesion. A subsequent histopathological examination of the resected polyp showed clusters of lymphatic vessels with marked cystic dilatation in the submucosa and the deep layer of the lamina propria mucosae. These characteristics are consistent with the typical features of small-bowel lymphangioma with erosions. Although clipping hemostasis was performed during EP, re-bleeding occurred. Finally, a complete hemostasis was achieved by performing an additional argon plasma coagulation.
- Citation: Kida A, Matsuda K, Hirai S, Shimatani A, Horita Y, Hiramatsu K, Matsuda M, Ogino H, Ishizawa S, Noda Y. A pedunculated polyp-shaped small-bowel lymphangioma causing gastrointestinal bleeding and treated by double-balloon enteroscopy. World J Gastroenterol 2012; 18(34): 4798-4800
- URL: https://www.wjgnet.com/1007-9327/full/v18/i34/4798.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i34.4798
A small-bowel lymphangiomas is a rare benign tumor of the lymphatic system but has been previously reported as a cause of significant gastrointestinal (GI) bleeding[1]. Recently, double-balloon enteroscopy (DBE) has been used for the diagnosis and treatment of obscure GI bleeding. We here report a rare case of a pedunculated polyp-shaped small-bowel lymphangioma causing massive GI bleeding that we successfully treated using DBE. In this patient, DBE therapy was performed using a combination of endoscopic polypectomy (EP), hemoclipping, and argon plasma coagulation (APC). This is a particularly unusual and interesting case as it has not only revealed a further rare form of small-bowel lymphangioma but also that DBE is an effective procedure for not only the diagnosis but also the treatment of this disorder. We conclude from our findings in this case that future differential diagnoses of GI bleeding of unknown origin should include small-bowel lymphangioma even though it is a rare condition.
An 81-year-old woman was treated for chronic heart failure and myeloid dysplasia (MDS). Since MDS was the underlying disease in this patient, her Hb levels were low at approximately 9.0 g/dL and in February 2011 decreased to 5.0 g/dL. Although upper GI endoscopy, lower GI endoscopy, and computed tomography procedures were performed, no source of bleeding could be identified. Subsequently, she had frequent episodes of melena and received a total of 20 transfusions of packed red cells (2800 mL), and underwent capsule endoscopy using a PillCam SB (Given Imaging, Ltd., Israel). This testing raised suspicions that the source of her bleeding was from the jejunum. She was subsequently referred to our hospital for further diagnosis and treatment.
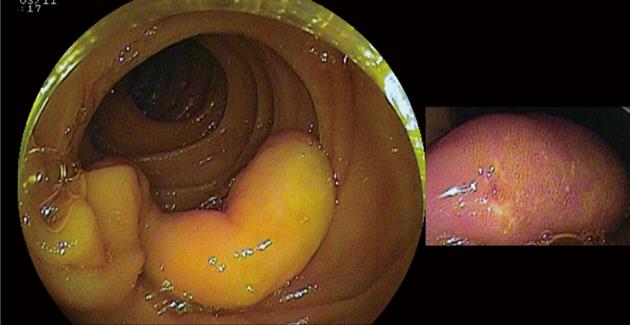
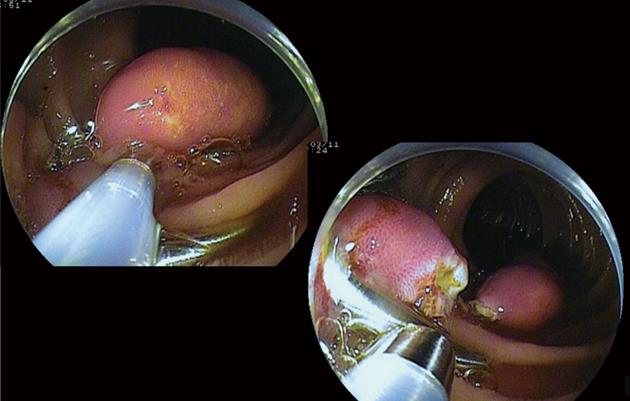
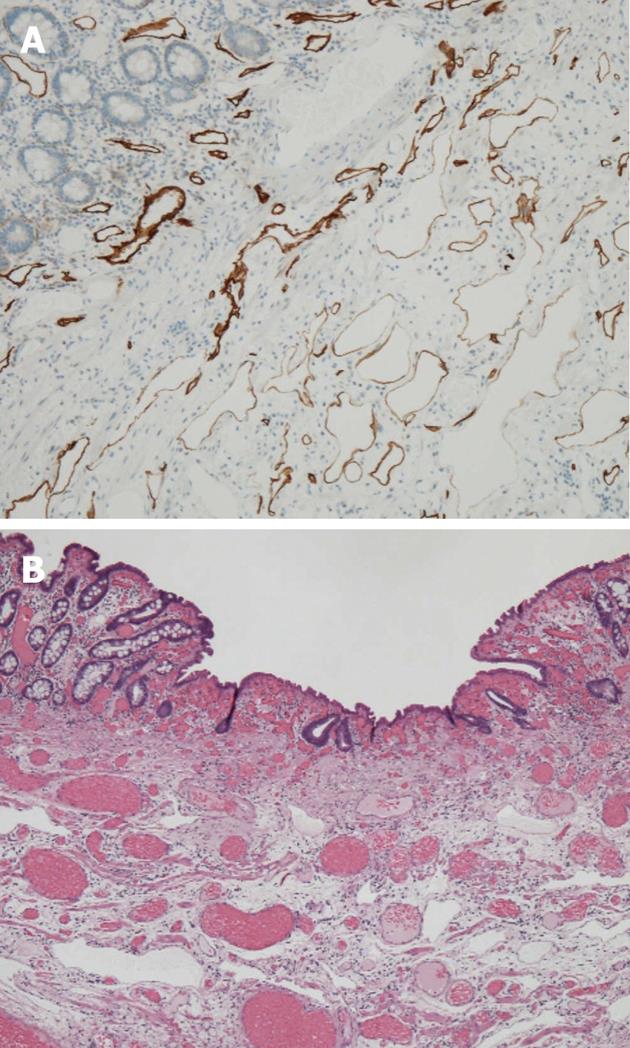
Since the lesion in this patient was located in the jejunum, antegrade DBE (Fujinon EN-450T5/W, Fujinon Corp., Saitama, Japan) was performed under intravenous propofol anesthesia. As a result, a collection of blood was observed at 10 cm distal to the ligament of Treitz, and a 20 mm × 10 mm white to yellowish, elongated, pedunculated jejunal polyp with erosions was identified (Figure 1). The DBE was advanced as far as possible to examine the distal jejunum and ileum, but no other source of bleeding was evident. After the placement of two hemoclips at the polyp base, EP was performed (Figure 2). The total time taken to perform the examinations and treatment, including the examination of the distal jejunum and the EP procedure, was 90 min. Surgery was completed without complications. Subsequent histopathological examination of the resected polyp revealed clusters of lymphatic vessels with marked cystic dilatation in the submucosa and in the deep layer of the lamina propria mucosae (Figure 3). These findings were consistent with the typical features of small-bowel lymphangioma with erosions. Following treatment, re-bleeding occurred twice at one and two months post-surgery. An antegrade DBE revealed that this occurred from the polypectomy site on both occasions. Hemoclipping and APC, after a submucosal saline injection to prevent perforation, were performed to achieve hemostasis at each instance of bleeding (Figure 4). No subsequent progression of anemia or recurrence of melena was observed in the patient.
Small-bowel lymphangiomas are commonly asymptomatic, but sometimes present with symptoms such as GI bleeding, abdominal pain, intussusception, and protein-losing gastroenteropathy[1,2]. Only 15 cases, including our current patient, of small-bowel lymphangioma with GI bleeding have been reported since 1967[1,3-9]. Of these, five individuals including our present case were diagnosed using DBE from 2007 onward[4-6]. The form of small-bowel lymphangioma revealed in the four previous cases was either a circumferential polyp with adjacent intestinal wall thickening or a flat or sessile polyp. The pedunculated polyp identified in our present case is therefore an extremely rare finding for a small-bowel lymphangioma.
Two reported patients, including the current case, have been treated endoscopically using DBE. Li et al[5] reported the treatment of a flat, hemorrhagic lesion by APC after a submucosal epinephrine injection to stop an occurrence of bleeding, thereby achieving complete hemostasis. However, as our present patient had a pedunculated polypoid lesion, EP was first performed by additional hemoclipping. However, re-bleeding occurred in our case, and hemostasis was finally achieved by APC. In terms of the cause of this re-bleeding, we speculate that a residual lymphangioma was present at the polypectomy site. Another previous case report has described a giant pedunculated angiolipofibroma of the distal duodenum for which EP was performed using an endoloop[10]. In this case, re-bleeding did not occur, but it was not certain from this that complete en bloc resection could be achieved by EP using an endoloop in cases of small-bowel lymphangioma.
We conclude from our present analysis that in cases of small-bowel lymphangioma causing GI bleeding, DBE therapy with a combination of EP, hemoclipping, and APC, would likely be beneficial approaches to treatment.
Peer reviewers: Dr. Weekitt Kittisupamongkol, Hua Chiew Hospital, 665 Bumrungmuang Road, Bangkok 10100, Thailand; Marcela Kopacova, MD, PhD, Professor, 2nd Department of Internal Medicine, Charles University in Praha, Faculty of Medicine at Hradec Král, University Teaching Hospital, Sokolska 581, 50005 Hradec Kralove, Czech; Satoshi Osawa, Assistant Professor, The First Department of Medicine, Hamamatsu University School of Medicine, 1-20-1 Handayama, Higashi-ku, Hamamatsu 431-3192, Japan
S- Editor Gou SX L- Editor A E- Editor Xiong L
.
| 1. | Gerosa Y, Bernard B, Lagneau M, You K, Hoang C, Brasseur JL, Opolon P, Valla D. [Cystic lymphangioma of the duodenum revealed by digestive hemorrhage and associated with exudative enteropathy]. Gastroenterol Clin Biol. 1993;17:591-593. [PubMed] [Cited in This Article: ] |
| 2. | Takami A, Nakao S, Sugimori N, Ishida F, Yamazaki M, Nakatsumi Y, Saito M, Otake S, Nakamura S, Matsuda T. Management of disseminated intra-abdominal lymphangiomatosis with protein-losing enteropathy and intestinal bleeding. South Med J. 1995;88:1156-1158. [PubMed] [Cited in This Article: ] |
| 3. | Onozato W, Nakamura T, Hatate K, Ozawa H, Satou T, Kokuba Y, Ihara A, Watanabe M. A case of Lymphangioma of the Ileum Presenting with Intussusception. Jpn J Gastroenterol Surg. 2007;40:1531-1535. [Cited in This Article: ] |
| 4. | Mavrogenis G, Coumaros D, Lakhrib N, Renard C, Bellocq JP, Leroy J. Mixed cavernous hemangioma-lymphangioma of the jejunum: detection by wireless capsule endoscopy. Endoscopy. 2011;43 Suppl 2 UCTN:E217-E218. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Li F, Osuoha C, Leighton JA, Harrison ME. Double-balloon enteroscopy in the diagnosis and treatment of hemorrhage from small-bowel lymphangioma: a case report. Gastrointest Endosc. 2009;70:189-190. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Hsu SJ, Chang YT, Chang MC, Yu SC, Lee JC, Shun CT, Wong JM. Bleeding jejunal lymphangioma diagnosed by double-balloon enteroscopy. Endoscopy. 2007;39 Suppl 1:E5-E6. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Griffa B, Basilico V, Feltri M, Griffa A. [Submucosal jejunal lymphangioma: an unusual case with obscure gastrointestinal bleeding in an adult, detected by video-capsule endoscopy and treated by laparoscopy]. Minerva Chir. 2006;61:529-532. [PubMed] [Cited in This Article: ] |
| 8. | Ugwonali O, Coady M, Saxena R, Robert M, Horowitz N, Topazian M. Intraoperative enteroscopy for diagnosis of a bleeding jejunal lymphangioma. J Clin Gastroenterol. 2000;31:333-335. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Barquist ES, Apple SK, Jensen DM, Ashley SW. Jejunal lymphangioma. An unusual cause of chronic gastrointestinal bleeding. Dig Dis Sci. 1997;42:1179-1183. [PubMed] [Cited in This Article: ] |
| 10. | Bartova J, Bures J, Podhola M, Rejchrt S, Tacheci I, Kopacova M. Endoscopic treatment of a giant pedunculated angiolipofibroma of the distal duodenum. Endoscopy. 2011;43 Suppl 2 UCTN:E96-E97. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |