Published online Jul 28, 2012. doi: 10.3748/wjg.v18.i28.3715
Revised: May 11, 2012
Accepted: June 8, 2012
Published online: July 28, 2012
AIM: To study if and how physicians use the irritable bowel syndrome (IBS) diagnostic criteria and to assess treatment strategies in IBS patients.
METHODS: A questionnaire was sent to 191 physicians regarding IBS criteria, diagnostic methods and treatment. Furthermore, 94 patients who were diagnosed with IBS underwent telephone interview.
RESULTS: A total of 80/191 (41.9%) physicians responded to the survey. Overall, 13 patients were diagnosed monthly with IBS by specialists in gastroenterology (SGs) and 2.5 patients by general practitioners (GPs). All the SGs knew of the criteria to diagnose IBS, as did 46/70 (65.7%) GPs. Seventy-nine percent used the patient’s history, 38% used a physical examination, and 38% exclusion of other diseases to diagnose IBS. Only 18/80 (22.5%) physicians used specific IBS criteria. Of the patients interviewed, 59/94 (62.8%) knew they had experienced IBS. Two out of five patients knew IBS and had seen a physician because of IBS symptoms. Half of those received a diagnosis of IBS. A total of 13% were satisfied with treatment. IBS affected daily activities in 43% of cases.
CONCLUSION: Half of the patients with IBS who consulted a physician received a diagnosis. Awareness and knowledge of diagnostic criteria for IBS differ between SGs and GPs.
- Citation: Olafsdottir LB, Gudjonsson H, Jonsdottir HH, Jonsson JS, Bjornsson E, Thjodleifsson B. Irritable bowel syndrome: Physicians' awareness and patients' experience. World J Gastroenterol 2012; 18(28): 3715-3720
- URL: https://www.wjgnet.com/1007-9327/full/v18/i28/3715.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i28.3715
Irritable bowel syndrome (IBS) is a common functional gastrointestinal disorder. The prevalence of IBS is estimated to range from 3% to 28% depending on the country studied[1-4]. The prevalence of IBS in the western countries is estimated to be 10%-15%[2]. However, ascertaining prevalence is based on various approaches in studies using different diagnostic criteria.
The criteria that have been used to identify IBS patients are the Manning criteria[5], Rome I[6], Rome II[7] and the most recent Rome III criteria[8,9]. The Rome criteria are more refined than the Manning criteria and include the duration of symptoms as part of the definition of IBS[10]. Studies have also shown that the Manning criteria are relatively sensitive but lack specificity[11] (Table 1).
| Manning |
| Pain eased after BM |
| Looser stools at onset of pain |
| More frequent BM at onset of pain |
| Abdominal distension |
| Mucus throughout rectum |
| Feeling of incomplete emptying |
| Rome I criteria |
| 3 mo or more of continuous or recurrent symptoms |
| Abdominal pain or discomfort |
| Relieved with defecation; and/or |
| Associated with a change in frequency of stool; and/or |
| Associated with a change in consistency of stool; and |
| Two or more of the following, at least 25% of occasions or days |
| Altered stool frequency (> 3 BMs/d or < 3/wk) |
| Altered stool form (lumpy/hard or loose/watery stool), |
| Altered stool passage (straining, urgency, tenesmus) |
| Passage of mucus |
| Bloating or feeling of abdominal distension |
| Rome II criteria |
| At least 12 wk (which need not be consecutive) |
| In the preceding 12 mo, of abdominal discomfort or pain that has two out of three features |
| Relieved with defecation; and/or |
| Onset associated with a change in frequency of stool, and/or |
| Onset associated with a change in form (appearance) of stool |
| Rome III criteria |
| Recurrent abdominal pain or discomfort at least 3 d/mo |
| In the last 3 mo association with two or more of the following: |
| Improvement with defecation |
| Onset associated with a change in frequency of stool |
| Onset associated with a change in form (appearance) of stool |
It has been questioned whether the Rome criteria are sensitive enough to diagnose patients in general practice. The current lack of interest in these criteria, especially among general practitioners (GPs), is unlikely to change unless they can be considerably improved[12]. The challenges and uncertainties for diagnosis of IBS have been listed as follows[13,14]: (1) there is currently no consistent biological marker of IBS, leaving clinicians to rely on patient symptoms alone to make the diagnosis; (2) symptoms of IBS are often difficult to quantify objectively; (3) symptoms can vary among individuals with IBS; and (4) many organic conditions can masquerade as IBS.
With these uncertainties, many physicians approach IBS as a diagnosis of exclusion[14]. A recent study concluded that: (1) the best practise diagnostic guidelines have not been uniformly adopted in IBS, particularly among primary care providers; (2) most community providers believe IBS is a diagnosis of exclusion (this belief is associated with increased diagnostic resource use); and (3) despite the dissemination of guidelines regarding diagnostic testing in IBS, there remains extreme variation in beliefs among both experts and non-experts[14].
Patients diagnosed with IBS exhibit a higher use of outpatient visits, inpatient stays, outpatient prescriptions, and number of hospitalizations than those not diagnosed with IBS[15-17]. A recent study showed that knowledge and use of the Rome criteria or their positive predictive values for IBS did not correlate with reduced use of diagnostic tests[18]. The cost for outpatient visits, drugs and diagnostic testing has been shown to be 51% higher for IBS patients than for others[15-17]. IBS patients have been shown to lose time from work more often than others and are less productive while at work[19]. This may reflect the morbidity in this relatively benign disorder, although up to 70% of IBS patients in the United States do not consult a health care provider regarding their symptoms[20]. IBS patients are often reluctant to consult a physician, often because they think their symptoms do not warrant a visit to a physician or are afraid that they have a serious life-threatening illness[2,19]. United States family practitioners have problems with IBS patients, which include difficulties in satisfying patients and difficulties in making a strategy decision and finding the time required, and their lack of knowledge could interfere with patient care[21]. No specific treatment options for IBS are available. In clinical practice, the decision to treat is up to the discretion of the physician[19]. While some physicians recommend lifestyle modification or trials with over-the-counter products, others recommend antispasmodics and antidepressants.
In our study, we aimed to analyze IBS from the physicians’ and patients’ point of view. The specific aims of this study were: First, physician study, to assess if and how physicians [GPs and specialists in gastroenterology (SGs)]: (1) use the diagnostic criteria to identify IBS; (2) diagnose patients with IBS, and which symptoms of IBS they identify; and (3) which treatment they recommend; and Second, patient study, to assess how patients with IBS are diagnosed and treated by physicians, as well as studying the ideas that patients have about IBS. The results of a parallel study based on the same database but focusing on functional dyspepsia, stability of IBS and heartburn have been published[22-24].
Participants and setting: In 1996, an epidemiological study of gastrointestinal diseases was performed in Iceland[25] among 2000 inhabitants aged 18-75 years. The individuals were randomly selected from the National Registry. Equal distribution of sex and age was secured in each age group. In 2006, we attempted to contact all the individuals from 1996, as well as adding 300 new individuals in the 18-27 years age group, who were also randomly selected from the National Registry of Iceland. A questionnaire was mailed to individuals at baseline and the study questionnaire and an explanatory letter mailed to all eligible individuals. Reminder letters were mailed at 2 wk, 4 wk and 7 wk, using the Total Method of Dillman[26]. Individuals who indicated at any point that they did not want to participate in the study were not contacted further.
Questionnaire: The Bowel Disease Questionnaire (BDQ)[27,28] was translated from English into Icelandic and modified for this study. The questionnaire was translated by two gastroenterologists and a pharmacist. A specialist in the Icelandic language at the University of Iceland made linguistic modifications. The questionnaire was piloted within a small group of IBS patients diagnosed by a gastroenterologist. The questionnaire was designed as a self-report instrument to measure symptoms experienced over the previous year and to collect the participants’ past medical history[29].
The Icelandic version of the BDQ questionnaire addressed 47 gastrointestinal symptoms and 32 items that measured past illness, health care use, and sociodemographic and psychosomatic symptoms, together with a valid measure of non-gastrointestinal somatic complaints, the Somatic Symptom Checklist (SSC)[30]. The SSC consisted of 12 non-gastrointestinal and five gastrointestinal symptoms or illnesses. Individuals were instructed to indicate, on a 5-point scale, how often each symptom appeared and how bothersome it was. There were only a few changes in the 2006 questionnaire, which addressed 51 gastrointestinal symptoms and 33 items that measured past illness, health care use, and sociodemographic and psychosomatic symptoms. The 2006 questionnaire furthermore addressed 17 items to identify heartburn and symptoms related to heartburn.
Telephone survey: In the questionnaire, patients were asked to write down their telephone number and give their permission to participate in a telephone survey. Subjects who were diagnosed with IBS based on the Manning criteria and/or the Rome III criteria and had written down their telephone number were called and interviewed.
In Iceland (population approximately 300 000), there are 177 physicians working in general practice and 17 SGs (three physicians who were involved in carrying out this study were excluded). A questionnaire was sent to these 191 physicians regarding awareness and application of the three sets of criteria used to diagnose IBS (Table 1), as well as diagnostic methods and treatment of this disorder. We assessed the knowledge of validated symptom-based criteria for IBS.
Tables were constructed for frequency and percentage. Categorical data were analyzed using the χ2 test. The type I error protection rate was set at 0.05. The exact P values are listed in the tables and text. All the research data were imported into SPSS software.
The National Bioethics Committee of Iceland and The Icelandic Data Protection Authority (Personuvernd) gave their permission for the research.
A total of 94 patients underwent telephone interview (29.8% male, 70.2% female) with a mean age of 47 years. All these had IBS according to the Manning criteria and 56.0% according to the Rome III criteria (the Rome III criteria being more refined and stricter than the Manning criteria). When patients were asked if they had experienced IBS (self-assessed), 62.8% reported yes and 21.3% said they had received an IBS diagnosis from a physician; 60% of these had a Rome-III-based diagnosis, and 100% had a Manning-based diagnosis.
Table 2 shows the awareness of IBS. Two out of five patients had heard of IBS and the same number had seen a physician because of IBS symptoms, but only half of those had received a diagnosis of IBS. Only 12/94 (12.8%) IBS patients were satisfied with the treatment they had been given. IBS did affect daily activities in approximately 43% of the cases (Table 2). One third of the IBS patients thought they would be cured of IBS but a similar proportion thought they would always suffer from IBS (Table 2). IBS patients were found to use more non-traditional medication than prescribed drugs. More than half of patients believed that dietary modification was important for treatment of IBS (Table 2).
| All patients (n = 94) | |
| Diagnosed with IBS | 20 (22.2) |
| Knowledge of IBS | 37 (39.4) |
| Seen a physician because of IBS symptoms | 37 (39.4) |
| Satisfied with treatment for IBS | 12 (12.8) |
| IBS affects daily activities | 40 (42.6) |
| Think they will be cured of IBS | 29 (30.9) |
| Think they will always suffer from IBS | 27 (28.7) |
| Takes medication for IBS | 11 (11.7) |
| Uses untraditional medication | 15 (16.0) |
| Thinks dietary modification is important for the treatment of IBS | 52 (55.3) |
Three out of five IBS patients were diagnosed by a gastroenterologist and two out of five by a GP. Most IBS patients reported abdominal pain (73.7%), bloating (21.1%), constipation (5.3%) and diarrhea (10.5%) as the symptom that led to the diagnosis. More than half (57.9%) of the IBS patients who received management for their IBS symptoms were satisfied.
An anonymous questionnaire was sent to a total of 191 physicians in Iceland in the fields of primary care, or to SGs (excluding three physicians involved in carrying out this study). A total of 80 physicians (41.9%) replied (83% male, 17% female) and completed the questionnaire. Of those who answered, 70/175 were GPs and 9/15 were SGs.
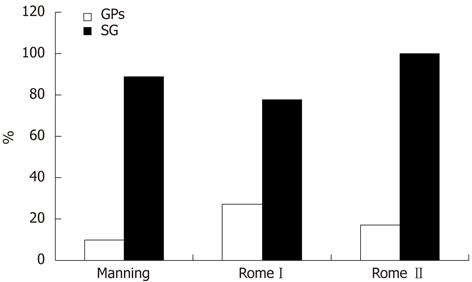
On average, 13 patients were estimated to be diagnosed with IBS monthly by SGs and 2.5 by GPs. Physicians reported how they diagnosed patients with IBS (Table 3). Two thirds of all the physicians knew that special diagnostic criteria exist for defining and diagnosing IBS (Figure 1).
| All patients | SG | GP | |
| n = 801 | n = 9 | n = 70 | |
| Patients history | 79 | 78 | 80 |
| Physical examination | 38 | 22 | 41 |
| Exclusion of other diseases | 38 | 44 | 35 |
| IBS criteria | 22 | 33 | 19 |
| Gastrointestinal endoscopy | 7 | 22 | 6 |
When physicians were asked if they knew of the IBS diagnostic criteria, 71% said yes (64% of GPs, 100% of SGs). Despite the fact that 64% of GPs claimed they knew that diagnostic criteria existed, only 10% had heard of the Manning criteria, 27% of Rome I, and 17% of Rome II (Figure 1).
Physicians stated that abnormal bowel movements such as diarrhea and constipation, abdominal pain and bloating were the most commonly reported symptoms of IBS (Table 4).
| GPs | SGs | |
| Abnormal bowel movements | 61 | 100 |
| Abdominal pain | 86 | 67 |
| Bloating | 20 | 56 |
| Gas | 9 | 11 |
| Passage of mucus | 5 | 0 |
| Incomplete evacuation with defecation | 5 | 11 |
Physicians reported in most cases that they would give advice on diet and education about IBS as a treatment for IBS symptoms. Both GPs and SGs gave their patients mebeverine in most cases. Psyllium was frequently used by SGs and chlordiazepoxide, and clidinium was in some cases used by both GPs and SGs (Table 5).
| GPs | SGs | |
| Medication | ||
| Mebeverine | 89 | 86 |
| Husk | 31 | 43 |
| Chlordiazepoxide and clidinium | 29 | 14 |
| Antidepressants | 7 | 14 |
| Other medicines | 9 | 14 |
| Lifestyle | ||
| Food | 98 | 86 |
| Relaxation | 14 | 14 |
| Exercise | 16 | 14 |
| Education about IBS | 90 | 86 |
| Do not know/something else | 27 | 14 |
Most physicians have used the method of exclusion when diagnosing patients with IBS. Most community providers also believe IBS is a diagnosis of exclusion rather than using positive criteria to support the diagnosis[14]. This approach-or lack of one-has therefore been time consuming and costly for the health care system. The importance of a precise diagnostic tool to diagnose IBS is therefore very important. In recent years, the development of diagnostic criteria for IBS has been ongoing, leading to the recent introduction of the Rome III criteria. There is no doubt that diagnostic criteria constitute a useful and important tool to help physicians make a positive diagnosis of IBS without resorting simply to excluding other diseases. This study has revealed the proportion of Icelandic physicians in two fields of medicine who are aware of the criteria for diagnosing the disease. The study has addressed not only the question of how informed physicians are of the criteria for diagnosing IBS, but also the importance of consensus about the diagnosis of the disease. This study has also addressed the IBS patients’ perspective, how many sought physicians, and how they experienced the disease.
According to the results of this study, most IBS patients were seen by GPs, and this is most likely also the case in other countries, underlining the importance of awareness and knowledge of IBS on the part of the GPs. Although 64% of all GPs reported that they were aware of the fact that special criteria to identify IBS existed, most of them (81%) did not know the criteria and therefore did not rely on them in practice. Most of them seem to make a positive diagnosis of IBS without the use of endoscopy. A United States study showed that only 30% of family practitioners knew that the Manning, Rome and Rome II criteria are used to diagnose IBS, which is in line with the results of the current study[21]. GPs are more likely than hospital specialists to perceive functional gastrointestinal disorders as having a psychological basis, are far less likely to be familiar with diagnostic criteria, and are more likely to use other methods to make such diagnoses[31]. However, physicians are aware of and use the most common IBS symptoms such as abnormal bowel movements, abdominal pain and bloating in their diagnostic approach, and these were the most common symptoms IBS subjects in the present study.
In the current study, physicians reported in most cases that they gave advice on diet and education on IBS as a treatment of IBS symptoms; this finding underlines the importance of providing reliable and useful information on IBS to patients, as well as the fact that there are no specific treatment options for IBS that are useful for all patients.
It is of interest that among interviewer-diagnosed IBS patients, only one out of five was diagnosed with IBS, even though more than half of the IBS patients saw a physician because of their symptoms. These results were irrespective of whether the patients fulfilled the Manning or Rome III criteria for IBS. This was also interesting because the majority of IBS patients reported that IBS affected daily activities. This emphasises the question of whether IBS patients reveal to the physicians the low quality of life caused by IBS. It is also conceivable that physicians do not recognize IBS as a disorder that leads to impaired quality of life. The absence of positive diagnosis of IBS might lead to lack of relevant treatment for specific symptoms of IBS such as abdominal pain. There is a need for a simple, practical and reliable diagnostic tool to be used in everyday clinical practice to diagnose IBS more accurately; a tool that will encourage physicians to be able to make a reliable diagnosis and to provide effective treatment[32,33].
The limitation of this study was the relatively low response rate in the physician study, which raises the question as to whether the level of awareness and knowledge of diagnostic criteria might be even lower than the result obtained. The strengths of the study, however, were that all physicians in Iceland in the relevant fields of general practice and gastroenterology were invited to participate, and the fact that all IBS patients who were contacted by telephone participated in the survey.
In conclusion, in this study, only half of the IBS patients who saw a physician received a diagnosis of IBS. Knowledge of IBS is limited among IBS patients. This study suggests that few physicians use IBS criteria and that awareness and knowledge of diagnostic criteria for IBS differed between SGs and GPs. One out of four physicians used a diagnosis of exclusion.
More widespread knowledge and use of the diagnostic criteria among physicians can be expected to support a more accurate diagnosis of IBS.
Irritable bowel syndrome (IBS) is a common functional gastrointestinal disorder. The prevalence of IBS in western countries is estimated to be 10%-15%. The criteria that have been used to identify IBS patients are the Manning criteria and Rome I, II and III criteria. It has been questioned whether the Rome criteria are sensitive enough to diagnose patients in general practice. Many physicians approach IBS as a diagnosis of exclusion. Patients diagnosed with IBS have a higher number of outpatient visits, inpatient stays, outpatient prescriptions, and hospitalizations than those not diagnosed with IBS. IBS patients are often reluctant to consult a physician, often because they think their symptoms do not warrant a visit to a physician, or they are afraid that they have a serious life-threatening illness. United States family practitioners have problems with IBS patients, which include difficulties in satisfying patients and treatment decision making, and finding the time required, and their lack of knowledge could interfere with patient care.
The prevalence of IBS in the general population is high and physicians often lack the tools to diagnose and treat IBS. It is important for IBS patients as well as the physicians to understand each other and the IBS symptoms, and to improve knowledge of IBS. The aim of the present study was to analyze IBS from the physicians’ and IBS patients’ points of view. The specific aims of this study were: First, physician study, to assess if and how physicians [general practitioners (GPs), specialists in gastroenterology (SGs)]: (1) use the diagnostic criteria to identify IBS; (2) diagnose patients with IBS, and which symptoms of IBS they identify; and (3) which treatment they recommend; and Second, patient study, to assess how patients with IBS based on criteria are diagnosed and treated by physicians and which treatment they receive, as well as studying the ideas that patients have about IBS.
The prevalence of IBS is high in Iceland. The awareness of IBS is low among patients with IBS and two out of five of those saw physicians because of IBS symptoms. Only half of the IBS patients who saw a physician received a diagnosis of IBS. Knowledge of IBS is limited among patients. This study suggests that few physicians use IBS criteria and that awareness and knowledge of the diagnostic criteria for IBS differed between SGs and GPs. One out of four physicians used a diagnosis of exclusion.
IBS patient and physician points of view are important for understanding IBS. It is important for the physicians to understand IBS patients and to know that many who seek medical care will not receive a diagnosis. This study creates a database for further studies and hopefully stimulates studies in other countries. International awareness and knowledge of IBS diagnosis and treatment can contribute towards better understanding of IBS.
The prevalence of IBS in Western countries is estimated to be 10%-15% and is associated with extensive health care expenses and diminished quality of life. Studies that examine IBS from the patients and physicians point of view are important and there is a need to document secular trends and compare various countries.
Peer reviewers: Kok Ann Gwee, FAMS, FRCP, PhD, Adjunct Associate Professor of Medicine, Yong Loo Lin School of Medicine, National University of Singapore, Gleneagles Hospital Annexe Block, 6A Napier Road, Suite No. 05-37, Singapore 258500, Singapore; Damian Casadesus Rodriguez, MD, PhD, Calixto Garcia University Hospital, J and University, Vedado, Havana 999075, Cuba
S- Editor Cheng JX L- Editor Kerr C E- Editor Zhang DN
| 1. | Talley NJ. Irritable bowel syndrome: definition, diagnosis and epidemiology. Baillieres Best Pract Res Clin Gastroenterol. 1999;13:371-384. [PubMed] [Cited in This Article: ] |
| 2. | Hungin AP, Whorwell PJ, Tack J, Mearin F. The prevalence, patterns and impact of irritable bowel syndrome: an international survey of 40,000 subjects. Aliment Pharmacol Ther. 2003;17:643-650. [PubMed] [Cited in This Article: ] |
| 3. | Drossman DA, Li Z, Andruzzi E, Temple RD, Talley NJ, Thompson WG, Whitehead WE, Janssens J, Funch-Jensen P, Corazziari E. U.S. householder survey of functional gastrointestinal disorders. Prevalence, sociodemography, and health impact. Dig Dis Sci. 1993;38:1569-1580. [PubMed] [Cited in This Article: ] |
| 4. | Akhtar AJ, Shaheen MA, Zha J. Organic colonic lesions in patients with irritable bowel syndrome (IBS). Med Sci Monit. 2006;12:CR363-CR367. [PubMed] [Cited in This Article: ] |
| 5. | Manning AP, Thompson WG, Heaton KW, Morris AF. Towards positive diagnosis of the irritable bowel. Br Med J. 1978;2:653-654. [PubMed] [Cited in This Article: ] |
| 6. | Drossman DA, Richter JE, Talley NJ, Thompson WG, Corazziari E, Whitehead WE. The Functional Gastrointestinal Disorders: Diagnosis, pathophysiology, and treatment-a multinational consensus. Boston: Little Brown 1994; . [Cited in This Article: ] |
| 7. | Thompson WG, Longstreth GF, Drossman DA, Heaton KW, Irvine EJ, Müller-Lissner SA. Functional bowel disorders and functional abdominal pain. Gut. 1999;45 Suppl 2:II43-II47. [PubMed] [Cited in This Article: ] |
| 8. | Drossman DA. The functional gastrointestinal disorders and the Rome III process. Gastroenterology. 2006;130:1377-1390. [PubMed] [Cited in This Article: ] |
| 9. | Longstreth GF, Thompson WG, Chey WD, Houghton LA, Mearin F, Spiller RC. Functional bowel disorders. Rome III: The Functional Gastrointestinal Disorders. 3rd ed. McLean, VA: Degnon Associates Inc 2006; . [Cited in This Article: ] |
| 10. | Hungin AP, Chang L, Locke GR, Dennis EH, Barghout V. Irritable bowel syndrome in the United States: prevalence, symptom patterns and impact. Aliment Pharmacol Ther. 2005;21:1365-1375. [PubMed] [Cited in This Article: ] |
| 11. | Fass R, Longstreth GF, Pimentel M, Fullerton S, Russak SM, Chiou CF, Reyes E, Crane P, Eisen G, McCarberg B. Evidence- and consensus-based practice guidelines for the diagnosis of irritable bowel syndrome. Arch Intern Med. 2001;161:2081-2088. [PubMed] [Cited in This Article: ] |
| 12. | Lea R, Hopkins V, Hastleton J, Houghton LA, Whorwell PJ. Diagnostic criteria for irritable bowel syndrome: utility and applicability in clinical practice. Digestion. 2004;70:210-213. [PubMed] [Cited in This Article: ] |
| 13. | Spiegel BM. Do physicians follow evidence-based guidelines in the diagnostic work-up of IBS? Nat Clin Pract Gastroenterol Hepatol. 2007;4:296-297. [PubMed] [Cited in This Article: ] |
| 14. | Spiegel BM, Farid M, Esrailian E, Talley J, Chang L. Is irritable bowel syndrome a diagnosis of exclusion?: a survey of primary care providers, gastroenterologists, and IBS experts. Am J Gastroenterol. 2010;105:848-858. [PubMed] [Cited in This Article: ] |
| 15. | Longstreth GF, Wilson A, Knight K, Wong J, Chiou CF, Barghout V, Frech F, Ofman JJ. Irritable bowel syndrome, health care use, and costs: a U.S. managed care perspective. Am J Gastroenterol. 2003;98:600-607. [PubMed] [Cited in This Article: ] |
| 16. | Eisen GM, Weinfurt KP, Hurley J, Zacker C, Coombs L, Maher S, Schulman KA. 2000. The economic burden of irritable bowel syndrome in a managed care organization. Am J Gastroenterol. 2000;95:2628-2629. [Cited in This Article: ] |
| 17. | Ganguly R, Barghout V, Frech F, Martin BC. The economic burden of irritable bowel syndrome to Medicaid. Am J Gastroenterol. 2001;S267 (abstract). [Cited in This Article: ] |
| 18. | Charapata C, Mertz H. Physician knowledge of Rome symptom criteria for irritable bowel syndrome is poor among non-gastroenterologists. Neurogastroenterol Motil. 2006;18:211-216. [PubMed] [Cited in This Article: ] |
| 19. | Hulisz D. The burden of illness of irritable bowel syndrome: current challenges and hope for the future. J Manag Care Pharm. 2004;10:299-309. [PubMed] [Cited in This Article: ] |
| 20. | Drossman DA, Camilleri M, Mayer EA, Whitehead WE. AGA technical review on irritable bowel syndrome. Gastroenterology. 2002;123:2108-2131. [PubMed] [Cited in This Article: ] |
| 21. | Longstreth GF, Burchette RJ. Family practitioners' attitudes and knowledge about irritable bowel syndrome: effect of a trial of physician education. Fam Pract. 2003;20:670-674. [PubMed] [Cited in This Article: ] |
| 22. | Olafsdottir LB, Gudjonsson H, Jonsdottir HH, Thjodleifsson B. Natural history of functional dyspepsia: a 10-year population-based study. Digestion. 2010;81:53-61. [PubMed] [Cited in This Article: ] |
| 23. | Olafsdottir LB, Gudjonsson H, Jonsdottir HH, Thjodleifsson B. Stability of the irritable bowel syndrome and subgroups as measured by three diagnostic criteria - a 10-year follow-up study. Aliment Pharmacol Ther. 2010;32:670-680. [PubMed] [Cited in This Article: ] |
| 24. | Olafsdottir LB, Gudjonsson H, Jonsdottir HH, Thjodleifsson B. Natural history of heartburn: a 10-year population-based study. World J Gastroenterol. 2011;17:639-645. [PubMed] [Cited in This Article: ] |
| 25. | Olafsdóttir LB, Gudjónsson H, Thjódleifsson B. [Epidemiological study of functional bowel disorders in Iceland]. Laeknabladid. 2005;91:329-333. [PubMed] [Cited in This Article: ] |
| 26. | Dillman Don A. Mail and Telephon Surveys: The total design method. New York: Wiley-Interscience Publication 1978; . [Cited in This Article: ] |
| 27. | Talley NJ, Phillips SF, Wiltgen CM, Zinsmeister AR, Melton LJ. Assessment of functional gastrointestinal disease: the bowel disease questionnaire. Mayo Clin Proc. 1990;65:1456-1479. [PubMed] [Cited in This Article: ] |
| 28. | Talley NJ, Phillips SF, Melton J, Wiltgen C, Zinsmeister AR. A patient questionnaire to identify bowel disease. Ann Intern Med. 1989;111:671-674. [PubMed] [Cited in This Article: ] |
| 29. | Halder SL, Locke GR, Schleck CD, Zinsmeister AR, Melton LJ, Talley NJ. Natural history of functional gastrointestinal disorders: a 12-year longitudinal population-based study. Gastroenterology. 2007;133:799-807. [PubMed] [Cited in This Article: ] |
| 30. | Attanasio V, Andrasik F, Blanchard EB, Arena JG. Psychometric properties of the SUNYA revision of the Psychosomatic Symptom Checklist. J Behav Med. 1984;7:247-257. [PubMed] [Cited in This Article: ] |
| 31. | Gladman LM, Gorard DA. General practitioner and hospital specialist attitudes to functional gastrointestinal disorders. Aliment Pharmacol Ther. 2003;17:651-654. [PubMed] [Cited in This Article: ] |
| 32. | Malagelada JR. A symptom-based approach to making a positive diagnosis of irritable bowel syndrome with constipation. Int J Clin Pract. 2006;60:57-63. [PubMed] [Cited in This Article: ] |
| 33. | Quigley EM, Bytzer P, Jones R, Mearin F. Irritable bowel syndrome: the burden and unmet needs in Europe. Dig Liver Dis. 2006;38:717-723. [PubMed] [Cited in This Article: ] |