Published online Dec 28, 2011. doi: 10.3748/wjg.v17.i48.5289
Revised: May 14, 2011
Accepted: May 21, 2011
Published online: December 28, 2011
AIM: To clarify whether the incidence of post-endoscopic retrograde cholangiopancreatography (ERCP) pancreatitis (PEP) after pancreatic guidewire placement (PGW) can be reduced by using a different cannulation method.
METHODS: Between April 2001 and October 2009, PGW was performed in 142 patients with native papilla to overcome difficult biliary cannulation. Our cannulation method for ERCP was changed from contrast injection (CI) using a single-lumen catheter (April 2001-May 2008) to wire-guided cannulation (WGC) using a double-lumen catheter (June 2008-October 2009). The CI protocol was also changed during the study period: in the first period it was used for routine pancreatography for detecting small pancreatic cancer (April 2001-November 2002), whereas in the second period it was not (December 2002-May 2008). In PGW with CI using a single-lumen catheter, the contrast medium in the catheter lumen was injected into the pancreatic duct. The success rate of biliary cannulation, the incidence of PEP according to the cannulation method, and the impact of CI using a single-lumen catheter on PEP in comparison with WGC using a double-lumen catheter were investigated.
RESULTS: CI with routine pancreatography, CI without routine pancreatography, and WGC were performed in 27 patients, 77 patients and 38 patients, respectively. Routine pancreatography did not contribute to the early diagnosis of pancreatic cancer in our study period. In CI without routine pancreatography and WGC, diagnostic pancreatography was performed in 17 patients and no patients, respectively. The success rate of biliary cannulation by PGW alone was 69%, and the final success rate was increased to 80.3% by the addition of consecutive maneuvers or a second ERCP. PEP occurred in 22 patients (15.5%), and the severity was mild in all cases. When analyzed according to cannulation method, the incidence of PEP was 37.0% (10/27) in the patients who underwent CI with routine pancreatography, 14.3% (11/77) in those who underwent CI without routine pancreatography, and 2.6% (1/38) in those who underwent WGC. In all patients who underwent CI using a single-lumen catheter, the incidence of PEP was 20% (21/104), which was significantly higher than that in WGC using a double-lumen catheter. In univariate and multivariate analysis, CI using a single-lumen catheter showed a high, statistically significant, odds ratio for PEP after PGW.
CONCLUSION: The practice of a cannulation method involving the use of a double-lumen catheter minimizes the CI dose administered to the pancreatic duct and reduces the incidence of PEP after PGW.
- Citation: Hisa T, Matsumoto R, Takamatsu M, Furutake M. Impact of changing our cannulation method on the incidence of post-endoscopic retrograde cholangiopancreatography pancreatitis after pancreatic guidewire placement. World J Gastroenterol 2011; 17(48): 5289-5294
- URL: https://www.wjgnet.com/1007-9327/full/v17/i48/5289.htm
- DOI: https://dx.doi.org/10.3748/wjg.v17.i48.5289
Recently, it has been emphasized that the use of wire-guided cannulation (WGC) in endoscopic retrograde cholangiopancreatography (ERCP) is associated with a reduced incidence of post-ERCP pancreatitis (PEP) compared with contrast injection (CI)[1-3]. In Japan, ERCP is usually performed under CI using a single-lumen catheter and a duodenoscope with a 15-degree backward-oblique angle because this technique allows selective biliary cannulation[4]. On the other hand, pancreatic guidewire placement (PGW) is one of the rescue maneuvers used to overcome difficult biliary cannulation[5-11]; however, it carries a risk of PEP[9-11]. We changed our cannulation method from CI using a single-lumen catheter to WGC using a double-lumen catheter and investigated whether the incidence of PEP after PGW was reduced by this change.
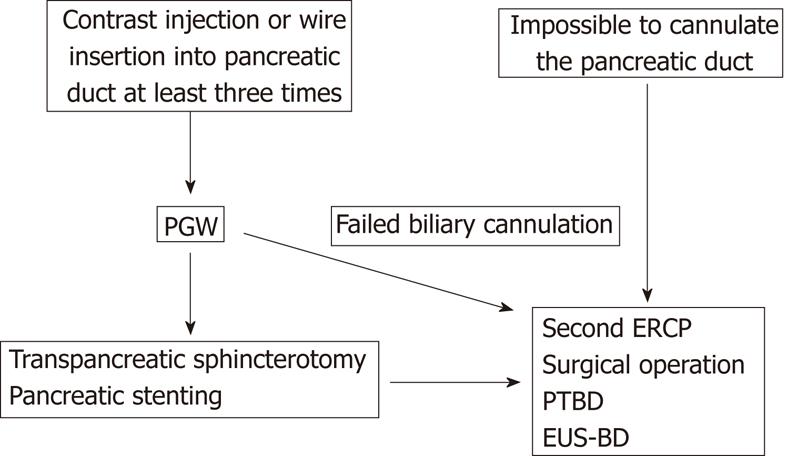
Between April 2001 and October 2009, 2060 ERCP procedures were performed in patients with pancreatobiliary disease at Saku Central Hospital. PGW was performed in 142 patients with native papilla, in whom CI or guidewire insertion into the pancreatic duct via biliary cannulation was unintentional on at least three occasions, which was defined as difficult biliary cannulation. We did not establish a maximum number of cannulation attempts. Our strategy for difficult biliary cannulation is shown in Figure 1. When PGW did not successfully achieve biliary cannulation, pancreatic stenting, transpancreatic sphincterotomy, or another maneuver was attempted. In cases in which it was not possible to access the bile duct within 30 min, the procedure was stopped.
Our cannulation method for ERCP was changed from CI using a single-lumen catheter (April 2001-May 2008) to WGC using a double-lumen catheter (June 2008-October 2009). The CI protocol was also changed during the study period: in the first period it was used for routine pancreatography for detecting small pancreatic cancer (April 2001-November 2002), whereas in the second period it was not (December 2002-May 2008). The procedure was performed using a duodenoscope with a 15-degree backward-oblique angle (JF230, 260V: Olympus Optical Co., Tokyo, Japan). Biliary cannulation was attempted with a single-lumen catheter (Contour: Microinvasive, Boston Scientific Corp., Natrick, MA, United States; PR-4Q-1, PR-10Q-1: Olympus Optical Co., Tokyo, Japan) under CI, a double-lumen catheter (MTW Endoskopie, Wesel, Germany), or a sphincterotome (CleverCut: Olympus Optical Co., Tokyo, Japan) for WGC.
In PGW, the tip of a 0.025 or 0.035 inch-guidewire (Revowave: Olympus Optical Co., Tokyo, Japan; Jagwire: Microinvasive, Boston Scientific Corp., Natrick, MA, United States) was placed between the pancreatic body and tail. In CI using a single-lumen catheter, the contrast medium in the catheter lumen was injected into the pancreatic duct during guidewire insertion, as shown in Figure 2. After PGW, biliary cannulation was attempted in the region towards the upper left of the pancreatic guidewire.
In WGC, the tip of the guidewire was passed through the catheter lumen and exposed/fixed at 2 mm from the tip of the catheter. The operator controlled the catheter and used it to adjust the axis between bile duct terminal and the catheter. In principle, the use of CI into the pancreatic duct was limited except during diagnostic pancreatography in WGC. When guidewire resistance arose during PGW, the minimum amount of contrast medium was used to identify the running direction of the main pancreatic duct to prevent the branch ducts from being injured by the tip of the guidewire.
All patients were administered a protease inhibitor drip infusion (ulinastatin, 100 000 units for 1 d) during and after the ERCP, and their serum amylase levels were measured before the ERCP and at 3 h, 6 h, and 18-24 h after. The diagnosis and grade of PEP were defined according to the international consensus criteria[12].
All procedures were performed by one operator (Hisa T), who experienced about 250-300 ERCPs per year.
In the 142 patients subjected to PGW, the success rate of biliary cannulation, the incidence of PEP according to the cannulation method, and the impact of CI using a single-lumen catheter on PEP in comparison with WGC using a double-lumen catheter were investigated.
The patients’ basic characteristics and the outcome of PGW were compared between CI using a single-lumen catheter and WGC using a double-lumen catheter using the χ2 test. Logistic regression modeling was used to evaluate the impact of CI using a single-lumen catheter on the incidence of PEP after PGW, compared with that of WGC using a double-lumen catheter. First, a crude odds ratio was estimated by univariate analysis in Model 1, and then it was adjusted for basic characteristics such as sex and age by multivariate analysis in Model 2. Finally, it was also adjusted for potential confounding variables including failed cannulation, bile duct stone removal, pancreatic brush cytology, and biliary sphincterotomy by multivariate analysis in Model 3. These potential confounders were selected as risk factors for PEP.
Statistical analysis was performed using SPSS software, version 14.0J (SPSS Inc, Japan). Odds ratios and 95% confidence intervals were used, and two-sided P values of less than 0.05 were considered statistically significant.
The patients’ characteristics and the endoscopic procedures used for PGW was illustrated in Table 1. There were no significant differences in these parameters, except for the incidence of choledocholithiasis, between CI using a single-lumen catheter and WGC using a double-lumen catheter.
| Total (n = 142) | Cannulation method | |||
| CI using a single-lumen catheter (n = 104) | WGC using a double-lumen catheter (n = 38) | P value | ||
| Mean age (mean ± SD) | 72.7 (11.5) | 68.5 (10.9) | 75.3 (13.2) | |
| Male sex (%) | 71 (50) | 48 (46) | 23 (61) | 0.18 |
| Periampullary diverticulum (%) | 28 (20) | 21 (20) | 7 (18) | 1.00 |
| Diagnosis (%) | ||||
| Choledocholithiasis | 55 (39) | 33 (32) | 22 (58) | 0.01 |
| Biliary cancer | 33 (23) | 25 (24) | 8 (21) | 0.90 |
| Pancreatic cancer | 24 (17) | 20 (19) | 4 (11) | 0.33 |
| Ampullary cancer | 4 (2.8) | 4 (3.8) | 0 (0) | 0.57 |
| ERCP maneuvers (%) | ||||
| Biliary sphincterotomy | 69 (49) | 50 (48) | 19 (50) | 0.99 |
| Transpancreatic sphincterotomy | 2 (1.4) | 1 (0.96) | 1 (2.6) | 0.87 |
| Papillary ballon dilatation | 4 (2.8) | 4 (4) | 0 (0) | 0.63 |
| Bile duct stone removal | 20 (14) | 14 (13) | 6 (16) | 0.91 |
| Biliary stenting | 55 (39) | 36 (35) | 19 (50) | 0.14 |
| Pancreatic stenting | 9 (6.3) | 8 (7.7) | 1 (2.6) | 0.50 |
CI with routine pancreatography, CI without routine pancreatography, and WGC were performed in 27 patients, 77 patients and 38 patients, respectively. Routine pancreatography did not contribute to the early diagnosis of pancreatic cancer in our study period. In CI without routine pancreatography and WGC, diagnostic pancreatography was performed in 17 patients and no patients, respectively.
The success rate of biliary cannulation by PGW alone was 69% (98/142), and the final success rate increased to 80.3% (114/142) after the addition of consecutive maneuvers or a second ERCP. In the 28 patients for whom biliary cannulation failed, a surgical operation was performed in 6 patients, percutaneous transhepatic biliary drainage was performed in 12 patients, endoscopic ultrasound-guided biliary drainage was performed in 2 patients, and an alternative examination or a follow-up study was performed in 8 patients. When analyzed according to the cannulation method, the success rate of biliary cannulation by PGW alone was 66% (69/104) in the patients who underwent CI using a single-lumen catheter and 76% (29/38) in the patients who underwent WGC using a double-lumen catheter, as shown in Table 2. There were no significant differences between the two cannulation methods with regard to the success rate of biliary cannulation.
| Total (n = 142) | Cannulation method | |||
| CI using a single-lumen catheter (n = 104) | WGC using a double-lumen catheter (n = 38) | P value | ||
| Successful biliary cannulation | 98 (69) | 69 (66) | 29 (76) | 0.35 |
| Post-ERCP pancreatitis | 22 (16) | 21 (20) | 1 (2.6) | 0.012 |
PEP occurred in 22 patients (15.5%), and the severity was mild in all cases. When analyzed according to the cannulation method, the incidence of PEP was 37.0% (10/27) in the patients who underwent CI with routine pancreatography, 14.3% (11/77) in those who underwent CI without routine pancreatography, and 2.6% (1/38) in those who underwent WGC. In all patients who underwent CI using a single-lumen catheter, the incidence of PEP was 20% (21/104), and it was significantly higher than that in the patients who underwent WGC using a double-lumen catheter, as shown in Table 2. In univariate and multivariate analysis, CI using a single-lumen catheter showed a high, statistically significant, odds ratio for PEP after PGW, as shown in Table 3. PEP did not occur in any patient who underwent pancreatic stenting.
| Model 1 crude OR (95% C.I.) | Model 2adjusted OR (95% C.I.) | Model 3adjusted OR (95% C.I.) | |
| CI using a single-lumen catheter | 9.4 (1.2-72)a | 10.2 (1.3-83)a | 10.8 (1.3-88)a |
| Female | 1.5 (0.56-3.9) | 1.4 (0.50-3.7) | |
| < 50 yr | 6.8 (0.79-59) | 6.1 (0.67-56) | |
| Failed cannulation | 1.2 (0.30-4.9) | ||
| Bile duct stone removal | 1.9 (0.46-7.5) | ||
| Pancreatic brush cytology | 0.55 (0.061-5.0) | ||
| Biliary sphincterotomy | 1.3 (0.36-4.7) |
In the present study, the incidence of PEP in the patients treated with PGW was 15.5%. When analyzed according to cannulation method, it was 37.0% in the patients who underwent CI with routine pancreatography, 14.5% in those who underwent CI without routine pancreatography, and 2.6% in those who underwent WGC. When CI using a single-lumen catheter is followed by PGW, the contrast medium in the catheter lumen is injected into the pancreatic duct and causes opacification of the entire pancreatic duct, as shown in Figure 2. Adding routine pancreatography to PGW is equal to performing two pancreatic ductal opacification procedures. Our data indicate that contrast injection into the entire pancreatic duct strongly correlates with the incidence of PEP after PGW. Cheon et al[13] also emphasized that a progressively higher frequency of PEP was detected as the extent of pancreatic ductal system opacification increased. In univariate and multivariate analysis, CI using a single-lumen catheter showed a high, statistically significant, odds ratio for PEP after PGW. Hence, a cannulation method involving the use of a double-lumen catheter to minimize the CI dose delivered into the pancreatic duct would be expected to reduce the incidence of PEP after PGW compared with CI using a single lumen catheter.
Herreros de Tejada et al[10] performed a multicenter, randomized, controlled trial involving 188 patients who had been subjected to 5 unsuccessful biliary cannulation attempts by WGC alone and divided them into the standard cannulation group (n = 87) and the attempted PGW group (n = 76). They emphasized that the incidence of PEP in the attempted PGW group was 17% (13/76), compared with 8% (7/87) in the standard cannulation group. However, as their attempted PGW group included 19 patients for whom PGW was unsuccessful and they did not explain in which cases PEP occurred, the incidence of PEP in the patients who successfully underwent PGW might have been lower. Ito et al[11] performed a prospective, randomized, controlled trial involving 70 patients who underwent PGW with CI, and they divided their subjects into the pancreatic stent group (n = 35) and the no-pancreatic stent group (n = 35). They concluded that the frequency of PEP in the pancreatic stent group was significantly lower than that in the no-pancreatic stent group (2.9% vs 23%). Hence, this suggests that papillary edema and/or CI into the pancreatic duct are strongly associated with the risk of PEP after PGW combined with CI. If PEP occurs due to pancreatic branch duct injuries caused by the PGW, pancreatic stenting will not be useful for preventing PEP. One concern about WGC without CI, especially in cases involving tortuous pancreatic ducts, is the risk of duct injury due to accidental guidewire insertion into a pancreatic branch duct. When guidewire resistance arises during PGW, we inject the minimal dose of contrast medium into the pancreatic duct in order to adjust the direction of the GW. It is interesting that the frequency of PEP in the pancreatic stent group in Ito’s study[11] was similar to that in the WGC group treated with a double-lumen catheter in our study (2.9% vs 2.6%). Nevertheless, pancreatic branch duct injury caused by PGW can lead to PEP. Therefore, it is necessary to investigate PGW cases in combination with information about accidental guidewire insertion/placement into the branch pancreatic duct in order to clarify whether PGW has a powerful effect on PEP.
Our study has the following limitations: it is not a prospective controlled study; the routine administration of protease inhibitors or improvements in the operator’s technique might have influenced the reduction in the incidence of PEP; information regarding the extent of pancreatic ductal system opacification is not investigated. However, our results suggest that the incidence of PEP after PGW is reduced by the use of a double-lumen catheter as it minimizes the CI dose delivered into the pancreatic duct.
In our study, the success rate of biliary cannulation by PGW alone was 69%. There have been 3 previous studies on PGW[8-11], as shown in Table 4, and the success rate of biliary cannulation by PGW alone ranged from 47% to 93%. The lowest success rate, which was found in Tejada’s study[10], can be attributed to the setting of a maximum number of cannulation attempts (15 attempts), since there was no limitation on the number of cannulation attempts in other studies. In contrast, the highest success rate, which was found in Maeda’s study[8], may have arisen from the small study population and the use of the vasodilator isosorbide dinitrate to improve the biliary cannulation rate. Our study is similar to Ito’s study[9] as it had a large study population; there were no limitations on the number of cannulation attempts; and it obtained a success rate of approximately 70% for PGW alone, which is acceptable. If PGW alone cannot successfully achieve biliary cannulation, PGW permits the use of another rescue technique such as transpancreatic sphincterotomy, another attempt at biliary cannulation, or precut sphincterotomy under pancreatic stenting. PGW is useful as a rescue maneuver for patients in whom biliary cannulation is difficult, providing the pancreatic duct is accessible.
| Primary author | Study design | No. of patients | Cannulation method | Success rate fo biliary cannulation | Incidence fo post-ERCP pancreatitis |
| Maeda[8] | RCT | Control (n = 26), attempted PGW (n = 27) | CI | 54%, 93% | 0%, 0% |
| Ito[9] | OS | PGW (n = 113) | CI | 73% | 12% |
| Herreros de Tejada[10] | RCT | Control (n = 87), attempted PGW (n = 76) | WGC | 56%, 47% | 8%, 17% |
| Ito[11] | RCT | PGW with no-PS (n = 35), PGW with PS (n = 35) | CI | 94%, 80% | 23%, 2.9% |
| Present study | OS | PGW (n = 142) | CI/WGC (104/38) | 69% (CI 66%, WGC 76%) | 16% (CI 20%, WGC 2.6%) |
In conclusion, when PGW is used as the initial rescue technique for difficult biliary cannulation, a cannulation method involving the use of a double-lumen catheter is recommended to minimize the dose of contrast medium injected into the pancreatic duct and hence reduce the incidence of PEP after PGW.
The authors thank Hirokazu Komatsu for his statistical advice, and Kuniyuki Horigome and Yuji Sakurai for their skillful technical assistance.
In Japan, endoscopic retrograde cholangiopancreatography (ERCP) is usually performed under contrast injection (CI) using a single-lumen catheter and a duodenoscope with 15-degree backward-oblique angle. Pancreatic guidewire placement (PGW) is one of the rescue maneuvers used to overcome difficult biliary cannulation. In CI using a single-lumen catheter, the contrast medium in the catheter lumen is injected into the pancreatic duct during PGW, and it carries a risk of post-ERCP pancreatitis (PEP).
It has been emphasized that the use of wire-guided cannulation (WGC) is associated with a reduced incidence of PEP compared with CI. WGC using a double-lumen catheter can minimize the dose of contrast medium injected into the pancreatic duct during PGW.
The authors changed their cannulation method from CI using a single-lumen catheter to WGC using a double-lumen catheter. In the patients who underwent CI using a single-lumen catheter, the incidence of PEP after PGW was significantly higher than that in WGC using a double-lumen catheter (20% vs 2.6%). In univariate and multivariate analysis, CI using a single-lumen catheter showed a high, statistically significant, odds ratio for PEP after PGW.
When PGW is used as the initial rescue technique for difficult biliary cannulation, a cannulation method involving the use of a double-lumen catheter is recommended to reduce the incidence of PEP after PGW.
PGW is used to overcome difficult biliary cannulation during ERCP. After PGW, biliary cannulation is attempted in the region towards the upper left of the pancreatic guidewire. WGC is a cannulation method in ERCP using a guidewire passed through the catheter lumen under fluoroscopic guidance.
This is an interesting article describing the utility of PGW without injection of the contrast for achieving biliary cannulation.
Peer reviewer: Dr. Kei Ito, Department of Gastroenterology, Sendai City Medical Center, 5-22-1, Tsurugaya, Miyagino-ku, Sendai City 983-0824, Japan
S- Editor Sun H L- Editor Logan S E- Editor Xiong L
| 1. | Lella F, Bagnolo F, Colombo E, Bonassi U. A simple way of avoiding post-ERCP pancreatitis. Gastrointest Endosc. 2004;59:830-834. [PubMed] [Cited in This Article: ] |
| 2. | Artifon EL, Sakai P, Cunha JE, Halwan B, Ishioka S, Kumar A. Guidewire cannulation reduces risk of post-ERCP pancreatitis and facilitates bile duct cannulation. Am J Gastroenterol. 2007;102:2147-2153. [PubMed] [Cited in This Article: ] |
| 3. | Lee TH, Park do H, Park JY, Kim EO, Lee YS, Park JH, Lee SH, Chung IK, Kim HS, Park SH. Can wire-guided cannulation prevent post-ERCP pancreatitis? A prospective randomized trial. Gastrointest Endosc. 2009;69:444-449. [PubMed] [Cited in This Article: ] |
| 4. | Kawakami H, Maguchi H, Hayashi T, Yanagawa N, Chiba A, Hisai H, Amizuka H. A prospective randomized controlled multicenter trial of duodenoscopes with 5 degrees and 15 degrees backward-oblique angle using wire-guided cannulation: effects on selective cannulation of the common bile duct in endoscopic retrograde cholangiopancreatography. J Gastroenterol. 2009;44:1140-1146. [PubMed] [Cited in This Article: ] |
| 5. | Dumonceau JM, Devière J, Cremer M. A new method of achieving deep cannulation of the common bile duct during endoscopic retrograde cholangiopancreatography. Endoscopy. 1998;30:S80. [PubMed] [Cited in This Article: ] |
| 6. | Gotoh Y, Tamada K, Tomiyama T, Wada S, Ohashi A, Satoh Y, Higashizawa T, Miyata T, Ido K, Sugano K. A new method for deep cannulation of the bile duct by straightening the pancreatic duct. Gastrointest Endosc. 2001;53:820-822. [PubMed] [Cited in This Article: ] |
| 7. | Hayashi H, Maeda S, Hosokawa O, Doden K, Hattori M, Tanikawa Y, Watanabe K, Ibe N, Tatsumi S. A technique for selective cannulation of the common bile duct in endoscopic retrograde cholangiopancreatography. Insertion of guidewire into the pancreatic duct (in Japanese with English abstract). Gastroenterol Endoscopy. 2001;43:828-832. [Cited in This Article: ] |
| 8. | Maeda S, Hayashi H, Hosokawa O, Dohden K, Hattori M, Morita M, Kidani E, Ibe N, Tatsumi S. Prospective randomized pilot trial of selective biliary cannulation using pancreatic guide-wire placement. Endoscopy. 2003;35:721-724. [PubMed] [Cited in This Article: ] |
| 9. | Ito K, Fujita N, Noda Y, Kobayashi G, Obana T, Horaguchi J, Takasawa O, Koshita S, Kanno Y. Pancreatic guidewire placement for achieving selective biliary cannulation during endoscopic retrograde cholangio-pancreatography. World J Gastroenterol. 2008;14:5595-5600; discussion 5599. [PubMed] [Cited in This Article: ] |
| 10. | Herreros de Tejada A, Calleja JL, Díaz G, Pertejo V, Espinel J, Cacho G, Jiménez J, Millán I, García F, Abreu L. Double-guidewire technique for difficult bile duct cannulation: a multicenter randomized, controlled trial. Gastrointest Endosc. 2009;70:700-709. [PubMed] [Cited in This Article: ] |
| 11. | Ito K, Fujita N, Noda Y, Kobayashi G, Obana T, Horaguchi J, Takasawa O, Koshita S, Kanno Y, Ogawa T. Can pancreatic duct stenting prevent post-ERCP pancreatitis in patients who undergo pancreatic duct guidewire placement for achieving selective biliary cannulation? A prospective randomized controlled trial. J Gastroenterol. 2010;45:1183-1191. [PubMed] [Cited in This Article: ] |
| 12. | Cotton PB, Lehman G, Vennes J, Geenen JE, Russell RC, Meyers WC, Liguory C, Nickl N. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991;37:383-393. [PubMed] [Cited in This Article: ] |
| 13. | Cheon YK, Cho KB, Watkins JL, McHenry L, Fogel EL, Sherman S, Lehman GA. Frequency and severity of post-ERCP pancreatitis correlated with extent of pancreatic ductal opacification. Gastrointest Endosc. 2007;65:385-393. [PubMed] [Cited in This Article: ] |