Published online Jul 14, 2010. doi: 10.3748/wjg.v16.i26.3239
Revised: May 15, 2010
Accepted: May 22, 2010
Published online: July 14, 2010
Interstitial cells of Cajal (ICC) are important players in the symphony of gut motility. They have a very significant physiological role orchestrating the normal peristaltic activity of the digestive system. They are the pacemaker cells in gastrointestinal (GI) muscles. Absence, reduction in number or altered integrity of the ICC network may have a dramatic effect on GI system motility. More understanding of ICC physiology will foster advances in physiology of gut motility which will help in a future breakthrough in the pharmacological interventions to restore normal motor function of GI tract. This mini review describes what is known about the physiologic function and role of ICCs in GI system motility and in a variety of GI system motility disorders.
- Citation: Mostafa RM, Moustafa YM, Hamdy H. Interstitial cells of Cajal, the Maestro in health and disease. World J Gastroenterol 2010; 16(26): 3239-3248
- URL: https://www.wjgnet.com/1007-9327/full/v16/i26/3239.htm
- DOI: https://dx.doi.org/10.3748/wjg.v16.i26.3239
Physiology of gut motility has been always a fascinating chapter in gastroenterology. It poses interesting challenges to physiologists. Our understanding of basic gut motility processes is advancing; a major emphasis is placed on elucidating gut regulatory mechanisms. A better appreciation of the importance of the presence of normal function of interstitial cells of Cajal (ICC) transformed this field of research. In 1893, Spanish Nobel Laureate physician and neuropathologist Santiago Ramon y Cajal, was the first to describe cells that are located between the nerve endings and smooth muscle cells in the gastrointestinal (GI) tract. Their location prompted him to call them “interstitial”. They are now known as the ICC.
ICC may be considered to be a specialized population of smooth muscle cells. Both arise from common mesenchymal cells[1-3]. However, whereas smooth muscle cells develop an extensive array of contractile elements, ICC have few contractile elements but contain large numbers of mitochondria, an abundance of endoplasmic reticulum and distinct sets of channels in their membrane. The ICC consist of a fusiform cell body with a thin cytoplasm, a large oval nucleus and dendritic-like processes[4]. Two to five primary dendritic processes divide further into secondary and tertiary processes[5]. Many ICC express Kit, a tyrosine kinase receptor (Kit-ir); this allows them to be recognized by their ability to bind antibodies to Kit[4]. Similarly ICC readily react with antibodies to vimentin whereas nearby smooth muscle cells do not[6]. The presence of ICC is not restricted to the GI tract. They can be found in the bladder[7,8], the ureteropelvic junction[9], the vas deferens[10], the prostate[11], the penis[12,13], the mammary gland, the uterus[14], the pancreas[15], blood vessels[16] such as the portal vein[17] and the vagina[18]. More recently, they have been found in the vermiform appendix in childhood[19]. Some of these cells are thought to have a pacemaker function (such as those in the portal vein, in the lymphatics or prostate) but not those in the arteries, uterus (where the influence is, if any, an inhibitory one) or bladder[20].
The motor activity of the GI tract is critical for life[21]. It is a complex process involving multiple cell types such as enteric neurons that can sense the contents of the GI tract, integrate information and devise a suitable motor pattern, ICC that transduce inputs from enteric motor neurons and generate intrinsic electrical rhythmicity, and smooth muscle cells that can interpret and integrate large arrays of inputs and develop appropriate responses[22]. ICC are a minor component of the tunica muscularis of the GI tract (only about 5% of cells present[23]); however, these cells have very significant physiological roles in GI motility[22].
Many tissues, isolated from different regions of the GI tract, contract rhythmically in the absence of neuronal or hormonal stimulation. When contractions and membrane potential are recorded simultaneously each contraction is seen to be triggered by a long lasting wave of depolarization: because of their low frequency of occurrence and long duration, the waves of depolarization have been termed slow waves[24]. The origin and basis of the generation of slow waves have been debated for many years. It was initially thought that the generation of slow waves reflected some properties of GI smooth muscle cells[25,26], but studies on isolated smooth muscle cells have consistently failed to demonstrate a capability to generate slow wave activity[27]. It has also long been recognized that the generation of slow waves does not rely on the sequential activation of voltage-dependent ion channels as do cardiac pacemaker cells. Rather, many early studies raised the possibility that rhythmical activity relied on the cycling of one or more metabolic processes within cells of the gut wall. Thus Conner and his colleagues proposed that the generation of slow waves involved changes in the activity of the sodium pump[25].
Subsequently Nakayama et al[28] suggested an involvement of glycolytic pathways, again assuming that pace making activity originated in smooth muscle cells. Although ICC were first described in the intestine a century ago by Cajal, they were long viewed as an oddity. Their role in the generation of pacemaker activity in the GI tract was suggested on the basis of histological studies[29]. More recently, studies on mutants that lack subpopulations of ICC revealed their role in the generation of rhythmicity[30].
Critically, whereas isolated smooth muscle cells rarely generate spontaneous electrical activity[27], isolated ICC invariably do[31,32].
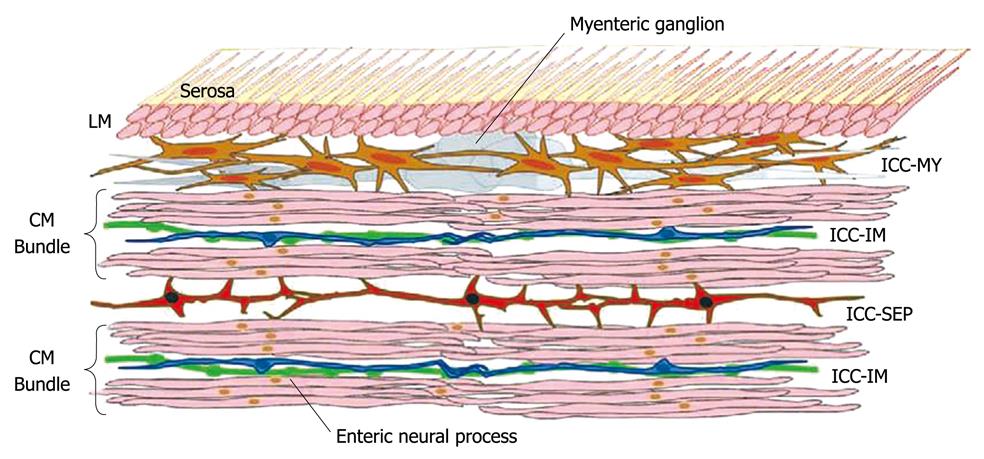
The discovery that ICC express c-Kit, the proto-oncogene that encodes the receptor tyrosine kinase Kit has offered a simple and reliable immunohistochemical method for determining the structure and distribution of ICC networks[30]. ICC are found throughout the GI tract from the esophagus to the internal anal sphincter[33,34]. Hanani et al[35] mentioned that while it is becoming clear that more than one type of ICC exists, based on both morphological and functional data, we still subdivide ICC based on location. Furthermore, Farrugia[36] emphasized the importance of revisiting a classification based solely on location and move towards a classification that is based on function, suggesting a reasonable start, to subdivide ICC into those that have the machinery to, and generate, unitary potential and slow waves and those that do not. Morphological studies now supported by some functional evidence suggest that at least three separate functional groups of ICC exist. In most regions of the GI tract, a network of ICC are located within the intermuscular space at the level of the myenteric plexus (ICC-MY) between the circular and longitudinal muscle layers. ICC-MY are the pacemaker cells in the stomach and small intestine that trigger the generation of slow waves in the tunica muscularis[37].
A second population of ICC (referred to as intramuscular ICC or ICC-IM) are found within the muscle layers of the GI tract and are innervated preferentially by enteric motor nerves[37]. ICC-IM are closely associated with not only enteric motor nerves but also vagal afferent nerves. Vagal afferent nerve fibers, labeled by the injection of neural tracers into the nodose ganglia, can terminate as intramuscular arrays within the musculature and as intraganglionic laminar ending within the myenteric ganglion of the stomach and duodenum. These afferent fibers transmit mechanoreceptive information from the muscle wall[38,39]. Horiguchi et al[40] gave histological evidence that a third population of ICC, ICC-SEP, lies within the septa between the circular muscle bundles, and suggested that it may play a role in conducting electrical information from ICC-MY deep into the distant circular muscle bundles, Figure 1 showing functional organization of ICC in the canine gastric antrum[41].
Electrophysiological data are presented which indicate that when the normal pathway from ICC-MY is sectioned, electrical stimulation of the cut ends of the muscle bundles can initiate slow waves over considerable distances. In the absence of stimulation, the muscle bundles isolated from ICC-MY can generate rhythmical activity but do so at low frequencies. Thus a distinct population of ICC, ICC-SEP, exists which can transfer pacemaker depolarization from ICC-MY deep into the distant bundles of circular muscle. Although ICC-SEP have the potential to generate pacemaker activity they are not normally the dominant pacemaker centre. As an analogy with the generation of pacemaker activity in the heart, the plexus of ICC-MY, like the sino-atrial node, is the dominant pacemaker centre. ICC-SEP, like Purkinje fibers, have the potential to generate pacemaker activity, but normally function to convey electrical activity from the dominant pacemaker region to more distant tissues[41].
Peristaltic motor activity is a motor pattern orchestrated by complex sequencing of neural excitation and inhibition in cooperation with intrinsic muscular control mechanisms, including those residing in ICC[42]. Peristalsis is defined as waves of contraction propagating along the GI tract for various distances as a means of mixing and propelling its content distally. Both the type of neural activity and the type of intrinsic myogenic control mechanism differ widely throughout the GI tract[42]. Physiological activation of peristalsis will in most cases involve the stretching of a segment of stomach, intestine, or colon and it will occur by neural pathways that contain additional mechanisms to those required for the ascending excitatory reflex[43]. When peristaltic motor activity occurs, in particular in stomach and proximal small intestine, the waves of contraction always have rhythmicity to it. This rhythmicity is determined by electrical slow wave activity in the musculature, referred to as pace maker activity[44].
New reagents, coupled with immunohistochemical techniques and new electrophysiological experimental approaches opened the door to recent progress in identification of the important roles of ICC as pacemakers, in propagation of slow waves and as mediators of inputs from enteric motor neurons[45]. Other functions, such as mechanosensors have also been proposed, but little physiological evidence supporting this function has been published[45].
Isolated ICC have been examined using conventional patch clamp recording techniques. This approach, which has been applied to ICC-MY, allows a description of the specific populations of ion channels present in their membrane[31,32,46] and an analysis of the cellular mechanisms which regulate the channels[47,48]. Simple intracellular recording from smooth muscle cells in isolated segments of GI tissues and isolated segments of urethra, after blocking smooth muscle L-type Ca2+ channels, record primarily the activity of the ICC in the tissues. The properties of ICC-MY can be determined in situ using sharp electrodes, allowing one to monitor the behavior of populations of interconnected ICC-MY and to determine how pacemaker potentials generate signals in adjacent smooth muscle layers[47,49,50]. A third method used to study the properties of ICC IM involves recording from small isolated segments of circular muscles; if dissected appropriately the preparations are isopotential and contain up to 2000 smooth muscle cells linked to up to 200 ICC-IM. The membrane potential of both smooth muscle cells and ICC-IM, can be varied over a limited range and the effects of nerve stimulation can be analyzed[51-53]. Finally, the use of mutant mice in which specific sets of ICC are either absent of dramatically reduced in numbers has allowed an evaluation of the physiological properties of tissues, with and without different sets of ICC[24].
Many GI motor disorders can be related to changes in number and/or structure and/or density of ICCs[54-57]. These changes can be primary, due to toxin substances, neurotoxins or viral diseases, or secondary as a consequence of neural damage, degraded tissue or treatment effect[54,58].
An absence or reduction in the number of ICCs causes abnormal electrical slow waves causing a decreased contractility of smooth muscle cells resulting in a diminished intestinal transit[56]. Although the density decreases, the slow wave is still present in most affected patients but the frequency and duration are prolonged[54].
ICC in human esophagus has a myoid ultrastructure with abundant smooth endoplasmic reticulum, numerous mitochondria, intermediate filaments, scattered caveolae, and discontinuous basal lamina. They are most frequent in the esophageal part of the lower esophageal sphincter (LES) but rare in the gastric part. They are in close contact with nerve terminals and make specific junctions with smooth muscle cells[59,60].
Achalasia: Achalasia is a disorder of esophageal motility that has been well documented for over 300 years[61]. Achalasia is characterized by relaxation failure of the LES and lack of peristaltic contraction of the esophageal body[62]. The mechanism of LES relaxation is complex, requiring the coordinated interaction of nerves, smooth muscle, ICC and hormones. The LES is a functional and anatomic barrier between the stomach and esophagus. It consists of a thickening of the circular smooth muscle layer of the esophagus at the gastroesophageal junction. It is anatomically asymmetric, and this is reflected in the physiology of the sphincter as demonstrated by ultrasound and pharmacologic manometric studies[63]. The LES is tonically contracted. Initiation of a peristaltic wave in the esophagus is accompanied by a decrease in LES pressure as a result of smooth muscle relaxation. This allows the swallowed bolus to enter the stomach[61].
ICC involvement in achalasia is debated. Electron microscope studies of the muscle coat of the LES in seven patients with achalasia showed that muscle wall components (nerve endings, smooth muscle cells, ICC and connective tissue) were modified. ICC ultrastructure was altered, namely clear cytoplasm, fewer mitochondria, and scarce smooth endoplasmic reticulum[64].
A reduced number of contacts between nerves and ICC were reported. Specific changes in smooth muscle cells were also documented, whereas the nerve endings had abnormal ultrastructure. Alterations in older patients were more pronounced[65]. Since the LES components specifically altered in achalasia are the nerve endings and ICC, they are regarded as principally responsible for abnormal motility[65].
Achalasia is uncommon among the pediatric population. It is usually sporadic and affects mainly teenagers[66]. A rare familial form combining early onset achalasia of cardia, alacrymia (absence of tears), and ACTH insensitivity, are known as Allgrove’s syndrome[67,68] or “Triple A” syndrome[69]. These forms are inherited on the autosomal recessive mode[70]. Massive loss of neural elements and neuronal nitric oxide synthase as well as a marked fibrotic process of the muscle layers of the cardia have been observed in “Triple A” syndrome[71]. ICC in the cardia are also markedly diminished or are completely absent while ICC (and neural structures) are preserved in the pylorus[59].
Gastroesophageal reflux: Gastroesophageal reflux (GERD) is a common condition and its prevalence varies in different parts of the World[72]. Typical symptoms of heartburn and acid regurgitation are encountered in 15%-20% of the general population[62]. The major mechanism for GERD is transient relaxation of the LES[73]. The role of the ICC in inhibitory transmission in the LES is still being discussed[62].
In W/Wv mutant mice (lack of ICC) LES pressure was lower than wild-type mice but a normal swallow still induced LES relaxation, arguing against the role of ICC in inhibitory transmission[74]. Another study demonstrated that in W/Wv animals, cholinergic and nitrergic neurotransmission is greatly reduced pleading for the role of ICC in mediating neural inputs[37]. However, enteric neurons, varicose processes, and the ability to release neurotransmitters are not reduced, and smooth muscle cells demonstrate responsiveness to exogenous transmitters[37].
Loss of ICC during development or in pathologic conditions would significantly compromise the ability of GI muscles to generate typical motor reflexes[75].
Esophagitis itself may be at the origin of an alteration of normal function of the Cajal cells: in advanced stages of GERD, inflammatory changes in the esophageal wall will also involve the ICC. That way, the more severe the esophagitis, the more severe is the ICC impairment. This destruction leads to loss of effective contraction of esophagus, maintaining reflux and thus aggravating the symptoms[76].
Gastroparesis: The pathogenesis of gastroparesis is complicated and poorly understood. This lack of understanding remains a major impediment to the development of effective therapies for this condition. Most of the scientific information available on the pathogenesis of gastroparesis has been derived from experimental studies of diabetes in animals. These studies suggest that the disease process can affect nerves (particularly those producing nitric oxide, but also the vagus nerve), ICC and smooth muscle[77]. It is broadly defined as disordered gastric emptying, and is a commonly encountered clinical problem[78]. Delayed gastric emptying can be secondary to muscular, neural, humoral causes or use of anticholinergic and opiate medicines. In the absence of an identified cause, gastroparesis is termed as idiopathic[79]. Gastroparesis has a broad range of clinical presentations ranging from dyspeptic symptoms to nausea, vomiting, abdominal pain, malnutrition, frequent hospitalizations and incapacitation[80], chronic abdominal pain and vomiting leading to dehydration, electrolyte imbalance, nutritional impairment and weight loss[81].
The ICC are fundamental in the generation of gastric slow waves[79]. A decrease in ICC density ranging from 60%-100% depending on the area investigated was demonstrated in histologic studies of the stomach of type 1 diabetic patients[55]. The number of immunopositive cells for c-kit was significantly decreased in the corpus and antrum of the gastroparesis patients compared with control tissues[62]. The loss of intramuscular ICC and associated nerves in the gastric fundus could explain the low basal gastric tone and increased compliance of the stomach. The hypomotility of the antrum can also be explained by the absence of slow wave generation by the ICC[23].
Infantile hypertrophic pyloric stenosis: Infantile hypertrophic pyloric stenosis (IHPS) is common in infants, characterized by marked delayed gastric emptying and hypertrophy of the inner (circular) muscle layer of the pylorus[59]. IHPS has been known for more than a century[82] but it remains a puzzling disorder[83]. The genetic susceptibility to development of IHPS seems to be multifactorial[84]. Hypertrophy of the pyloric musculature develops after birth[85] and produces the characteristic palpable pyloric “olive.” The pyloric lumen is however not fully occluded[86] and can be intubated relatively easily[87], suggesting that the obstruction of the gastric outlet in IHPS is not merely due to a mechanical obstruction by the hypertrophied musculature. The extent of muscle hypertrophy appeared to be unrelated to the age or duration of symptoms[88].
Various neurotransmitters[89-91] and the neuronal isoform of NO synthase[92] are reduced or lacking in the hypertrophic musculature. The increased thickness of the pyloric muscular coats appears to be due to hypertrophy, rather than to hyperplasia, of the smooth muscle cells[93]. ICC, identified either by electron microscopy[94] or by Kit-ir[95,96] were consistently lacking in the hypertrophic circular muscle layer. However, Kit-ir cells, similar to Kit-ir ICC observed in controls, were observed in the innermost part of the hypertrophic pylorus and in the antrum, indicating that the lack of Kit-ir is restricted to the hypertophic pyloric musculature[95].
The lack of ICC in IHPS may interfere with the propagation of slow waves and may be, at least partly, involved in antro-pyloric incoordination[59]. Homozygous transgenic mice carrying inactivated genes (‘‘knock-out’’) coding for the neuronal NO synthase developed hypertrophy of the pylorus[97]. The link between the lack of ICC, the lack of inhibitory nitrergic neurotransmission, and the hypertrophy of the smooth musculature in IHPS remains to be elucidated[59].
Hirschsprung’s disease: Hirschsprung’s disease (HD) is characterized by the lack of intrinsic enteric nervous system (ENS) in the distal part of the GI tract (‘‘aganglionosis’’). The affected segment extends cranially from the anus and encompasses a variable portion of the gut. Functionally, the lack of propulsive movements may lead either to an early obstructive syndrome in infancy or to a severe constipation[98]. Lack of slow wave activity in the aganglionic segment has been identified[99]. Kit immunohistochemistry identified ICC in HD. However, the cellular density of Kit+ ICC appeared markedly reduced in the aganglionic segment[100]. ICC-MP were rather abundant in the (aganglionic) space between the muscle layers. Kit+ ICC were specially scarce in the inner part of the circular musculature and in the submuscular plexus. However, the presence of some ICC-SMP was confirmed by electron microscopy.
In contrast, another study reported a distribution of Kit+ ICC in HD comparable to controls and claimed that Kit1 ICC-MP form “normal” networks in aganglionic segments when studied by confocal microscopy on whole mount preparations[101].
Differences in interpretation may be less significant than it appears as there is an agreement in the literature to acknowledge the presence of a number of interconnecting ICC-MP in aganglionic segments but there is no objective criterion to assess the “normality” of networks. Considering the very close relationships of ICC with intrinsic nerves and glial cells in the normal gut, a normal arrangement of ICC appears quite unlikely in the absence of both intrinsic nerves and glial cells as encountered in aganglionic segments. In the embryonic chicken[1] or mouse[102] gut experimentally deprived of neural crest derivatives, ICC develop in the absence of ENS, confirming the mesenchymal nature of ICC. But it has not been established if ICC fully develop morphologically and functionally in such conditions.
HD is a heterogenous, multigenic disease and reviewing its genetic aspects is beyond the scope of this paper. Several systems regulating neural crest migration have recently been identified[103]. Some genes are expressed by the neural crest, others by the mesenchyme of the gut. Kit has previously been considered as a possible candidate in the search for genes involved in hereditary forms of HD[104] but the absence of linkage between HD and the region of the Kit gene has been more recently reported[105]. The genetic defects leading to aganglionosis in the HD patients enrolled in all studies on ICC published so far have not been assessed. Subtle differences may explain the discrepancies observed between studies, and a link between some specific genetic defect leading to aganglionosis and the differentiation of ICC in HD patients cannot be ruled out.
Intestinal neural dysplasia: A clinical condition that resembles HD was first described by Meier-Ruge[106] in 1971 as a malformation of the enteric plexus. In 1983, Fadda et al[107] subclassified intestinal neural dysplasia (IND) into two clinically and histologically distinct subtypes. Type A occurs in less than 5% of cases, is characterized by congenital aplasia or hypoplasia of the sympathetic innervations, and presents acutely in the neonatal period with episodes of intestinal obstruction, diarrhea and bloody stools. The clinical picture of Type B resembles HD and is characterized by malformation of the parasympathetic submucous and myenteric plexuses and accounts for over 95% of cases of isolated IND. IND occurring in association with HD is of Type B[108]. IND have been reported to be associated with loss or deficiency of ICC networks[109].
Chronic intestinal pseudo-obstruction: Chronic intestinal pseudoobstruction (CIPO) is characterized by defective GI propulsion together with symptoms and signs of bowel obstruction in the absence of any lesions or mechanical obstacle[110]. It is generally a serious, even life-threatening, condition with frequent need for long-term parenteral nutrition. CIPO can either be restricted to the intestine, can involve other parts of the GI tract, or can be part of a multisystemic disorder[59]. CIPO can be secondary to a number of identified disorders or can be “idiopathic”[111]. Very little is known about the etiology of idiopathic CIPO. Pathological features of CIPO are pleiomorphic. A number of alterations of the ENS (‘‘neuropathic” forms)[112] and “myopathic” forms, limited to the musculature of the GI tract or involving also the musculature of the urinary system[113,114], have been described.
Slow transit constipation: Functional constipation encompasses a group of functional disorders that exhibit persistent difficult, infrequent, or seemingly incomplete defecation and infrequent, lumpy, or hard stools[115,116]. This symptom is very common and may occur in up to 20% of populations, depending on demographic factors, sampling, and the definitions employed[115,117]. The term constipation is probably better viewed as a sort of semantic umbrella, covering pathophysiologic subtypes, among which 2 major groups may now be identified: slow transit constipation (STC) and pelvic floor dysfunction[118].
STC is thought to have, as a primary defect, slower than normal movement of contents from the cecum to the rectum[119]. This is a very prevalent motility problem, but its mechanisms are unclear[62]. Although STC may not be a congenital disease, the frequent onset in adolescence and strong female predominance suggest that STC could be a result of a sex modified multifactorial disorder of the GI tract with a genetic basis[120].
ICC volume was significantly lower in the STC patien+cross all colonic regions[121]. Expression of c-kit mRNA and c-kit protein was significantly decreased in the colon of STC, suggesting that the c-kit signal pathway may play an important role in ICC reduction in STC[122]. Shafik et al[123] concluded that a disorder of the ICC, which generate electric activity, may have a role in inducing diminished or absent colonic motor activity, a point that should be further investigated.
GI stromal tumors (GISTs) have been recognized as a biologically distinctive tumor type, different from smooth muscle and neural tumors of the GI tract. They constitute the majority of GI mesenchymal tumors[124].
GISTs exhibit considerable phenotypic heterogeneity[125]. Their origin remains unclear, although origin in smooth muscle cells has been proposed[126,127]. CD34-ir is often present in GIST[125,128-130], a property shared with various other solid tumors[131,132].
Kit-ir may be a suitable marker for GIST[133], possibly superior to CD34-ir[134]. Mutations (usually activating) of the proto-oncogene Kit have been identified in GIST[133,135-137]. GIST with Kit mutation appear to have a poorer prognosis[133,135-138]. Therefore Kit mutations may merely be part of the oncogenic process rather than an indication of the origin of these tumors.
Recent studies suggesting that ICC in the human gut were both Kit-ir and CD34-ir raised the idea that Kit+ CD34+ GIST may derive from ICC[128,133,137].
The majority of GISTs occurs in the stomach (60%-70%), small intestine (20%-30%) and only 10% or less in the esophagus, colon and rectum, and they affect mainly middle aged patients. Similar tumors, sometimes known as extra-GIST, may arise in the omentum, mesentery, or retroperitoneum and at least one case of pancreatic tumor was described[139,140]. The presence of ICC in normal pancreas was demonstrated recently[15].
The symptoms may vary from none or slight abdominal discomfort to brisk GI hemorrhage, perforation or obstruction.
Imatinib mesylate, a synthetic tyrosine kinase inhibitor developed for the use in the management of interferon resistant chronic myeloid leukemia, was shown to be effective against a number of other tyrosine kinases including c-kit and platelet derived growth factor and now it is considered to be the drug of choice for metastatic and inoperable GISTs[124,141].
Knowledge on the role of ICC in GI disorders is increasing and there is currently overwhelming evidence to support the idea that ICC play important roles in GI motility in laboratory animals. Studies of several animal models have shown that the lack of specific ICC subpopulations produces major disturbances of GI motility. ICC are unique cell types with a central role in the control of gut function. Further studies of ICC may, therefore, lead to a major breakthrough in more understanding of GI physiology which may be considered as a promising target, at least in the long run, for specific pharmacological interventions to restore the normal physiology and motor functions of the GI tract.
Peer reviewers: Akio Inui, MD, PhD, Professor, Department of Behavioral Medicine, Kagoshima University Graduate School of Medical and Dental Sciences, 8-35-1 Sakuragaoka, Kagoshima 890-8520, Japan; Tomohiko Shimatani, Assistant Professor, Department of General Medicine, Hiroshima University Hospital, 1-2-3 Kasumi, Minami-ku, Hiroshima 7348551, Japan
S- Editor Tian L L- Editor O’Neill M E- Editor Zheng XM
| 1. | Lecoin L, Gabella G, Le Douarin N. Origin of the c-kit-positive interstitial cells in the avian bowel. Development. 1996;122:725-733. [Cited in This Article: ] |
| 2. | Young HM, Ciampoli D, Johnson PJ, Stebbing MJ. Inhibitory transmission to the longitudinal muscle of the mouse caecum is mediated largely by nitric oxide acting via soluble guanylyl cyclase. J Auton Nerv Syst. 1996;61:103-108. [Cited in This Article: ] |
| 3. | Young HM. Embryological origin of interstitial cells of Cajal. Microsc Res Tech. 1999;47:303-308. [Cited in This Article: ] |
| 4. | Sanders KM. A case for interstitial cells of Cajal as pacemakers and mediators of neurotransmission in the gastrointestinal tract. Gastroenterology. 1996;111:492-515. [Cited in This Article: ] |
| 5. | Faussone-Pellegrini MS, Thuneberg L. Guide to the identification of interstitial cells of Cajal. Microsc Res Tech. 1999;47:248-266. [Cited in This Article: ] |
| 6. | Rumessen JJ, Thuneberg L. Pacemaker cells in the gastrointestinal tract: interstitial cells of Cajal. Scand J Gastroenterol Suppl. 1996;216:82-94. [Cited in This Article: ] |
| 7. | Piaseczna Piotrowska A, Rolle U, Solari V, Puri P. Interstitial cells of Cajal in the human normal urinary bladder and in the bladder of patients with megacystis-microcolon intestinal hypoperistalsis syndrome. BJU Int. 2004;94:143-146. [Cited in This Article: ] |
| 8. | Shafik A, El-Sibai O, Shafik AA, Shafik I. Identification of interstitial cells of Cajal in human urinary bladder: concept of vesical pacemaker. Urology. 2004;64:809-813. [Cited in This Article: ] |
| 9. | Solari V, Piotrowska AP, Puri P. Altered expression of interstitial cells of Cajal in congenital ureteropelvic junction obstruction. J Urol. 2003;170:2420-2422. [Cited in This Article: ] |
| 10. | Fischer C, Johnson J, Stillwell B, Conner J, Cerovac Z, Wilson-Rawls J, Rawls A. Activating transcription factor 4 is required for the differentiation of the lamina propria layer of the vas deferens. Biol Reprod. 2004;70:371-378. [Cited in This Article: ] |
| 11. | Shafik A, Shafik I, el-Sibai O. Identification of c-kit-positive cells in the human prostate: the interstitial cells of Cajal. Arch Androl. 2005;51:345-351. [Cited in This Article: ] |
| 12. | Hashitani H, Suzuki H. Identification of interstitial cells of Cajal in corporal tissues of the guinea-pig penis. Br J Pharmacol. 2004;141:199-204. [Cited in This Article: ] |
| 13. | Shafik A. Study of interstitial cells in the penis: human study. J Sex Med. 2007;4:66-71. [Cited in This Article: ] |
| 14. | Shafik A, El-Sibai O, Shafik I. Identification of c-kit-positive cells in the uterus. Int J Gynaecol Obstet. 2004;87:254-255. [Cited in This Article: ] |
| 15. | Popescu LM, Hinescu ME, Ionescu N, Ciontea SM, Cretoiu D, Ardelean C. Interstitial cells of Cajal in pancreas. J Cell Mol Med. 2005;9:169-190. [Cited in This Article: ] |
| 16. | Harhun MI, Pucovský V, Povstyan OV, Gordienko DV, Bolton TB. Interstitial cells in the vasculature. J Cell Mol Med. 2005;9:232-243. [Cited in This Article: ] |
| 17. | Povstyan OV, Gordienko DV, Harhun MI, Bolton TB. Identification of interstitial cells of Cajal in the rabbit portal vein. Cell Calcium. 2003;33:223-239. [Cited in This Article: ] |
| 18. | Shafik A, El-Sibai O, Shafik I, Shafik AA. Immunohistochemical identification of the pacemaker cajal cells in the normal human vagina. Arch Gynecol Obstet. 2005;272:13-16. [Cited in This Article: ] |
| 19. | Richter A, Wit C, Vanderwinden JM, Wit J, Barthlen W. Interstitial cells of Cajal in the vermiform appendix in childhood. Eur J Pediatr Surg. 2009;19:30-33. [Cited in This Article: ] |
| 20. | McHale N, Hollywood M, Sergeant G, Thornbury K. Origin of spontaneous rhythmicity in smooth muscle. J Physiol. 2006;570:23-28. [Cited in This Article: ] |
| 21. | Huizinga JD, Lammers WJ. Gut peristalsis is governed by a multitude of cooperating mechanisms. Am J Physiol Gastrointest Liver Physiol. 2009;296:G1-G8. [Cited in This Article: ] |
| 22. | Sanders KM, Ward SM. Kit mutants and gastrointestinal physiology. J Physiol. 2007;578:33-42. [Cited in This Article: ] |
| 23. | Ordög T, Redelman D, Horváth VJ, Miller LJ, Horowitz B, Sanders KM. Quantitative analysis by flow cytometry of interstitial cells of Cajal, pacemakers, and mediators of neurotransmission in the gastrointestinal tract. Cytometry A. 2004;62:139-149. [Cited in This Article: ] |
| 24. | Hirst GD, Ward SM. Interstitial cells: involvement in rhythmicity and neural control of gut smooth muscle. J Physiol. 2003;550:337-346. [Cited in This Article: ] |
| 25. | Connor JA, Prosser CL, Weems WA. A study of pace-maker activity in intestinal smooth muscle. J Physiol. 1974;240:671-701. [Cited in This Article: ] |
| 26. | El-Sharkaway TY, Daniel EE. Ionic mechanisms of intestinal electrical control activity. Am J Physiol. 1975;229:1287-1298. [Cited in This Article: ] |
| 27. | Farrugia G. Ionic conductances in gastrointestinal smooth muscles and interstitial cells of Cajal. Annu Rev Physiol. 1999;61:45-84. [Cited in This Article: ] |
| 28. | Nakayama S, Chihara S, Clark JF, Huang SM, Horiuchi T, Tomita T. Consequences of metabolic inhibition in smooth muscle isolated from guinea-pig stomach. J Physiol. 1997;505:229-240. [Cited in This Article: ] |
| 29. | Thuneberg L. Interstitial cells of Cajal: intestinal pacemaker cells? Adv Anat Embryol Cell Biol. 1982;71:1-130. [Cited in This Article: ] |
| 30. | Huizinga JD, Thuneberg L, Klüppel M, Malysz J, Mikkelsen HB, Bernstein A. W/kit gene required for interstitial cells of Cajal and for intestinal pacemaker activity. Nature. 1995;373:347-349. [Cited in This Article: ] |
| 31. | Langton P, Ward SM, Carl A, Norell MA, Sanders KM. Spontaneous electrical activity of interstitial cells of Cajal isolated from canine proximal colon. Proc Natl Acad Sci USA. 1989;86:7280-7284. [Cited in This Article: ] |
| 32. | Tokutomi N, Maeda H, Tokutomi Y, Sato D, Sugita M, Nishikawa S, Nishikawa S, Nakao J, Imamura T, Nishi K. Rhythmic Cl- current and physiological roles of the intestinal c-kit-positive cells. Pflugers Arch. 1995;431:169-177. [Cited in This Article: ] |
| 33. | Daniel EE, Posey-Daniel V. Neuromuscular structures in opossum esophagus: role of interstitial cells of Cajal. Am J Physiol. 1984;246:G305-G315. [Cited in This Article: ] |
| 34. | Hagger R, Gharaie S, Finlayson C, Kumar D. Distribution of the interstitial cells of Cajal in the human anorectum. J Auton Nerv Syst. 1998;73:75-79. [Cited in This Article: ] |
| 35. | Hanani M, Farrugia G, Komuro T. Intercellular coupling of interstitial cells of cajal in the digestive tract. Int Rev Cytol. 2005;242:249-282. [Cited in This Article: ] |
| 36. | Farrugia G. Interstitial cells of Cajal in health and disease. Neurogastroenterol Motil. 2008;20 Suppl 1:54-63. [Cited in This Article: ] |
| 37. | Ward SM, Beckett EA, Wang X, Baker F, Khoyi M, Sanders KM. Interstitial cells of Cajal mediate cholinergic neurotransmission from enteric motor neurons. J Neurosci. 2000;20:1393-1403. [Cited in This Article: ] |
| 38. | Iino S, Horiguchi K. Interstitial cells of cajal are involved in neurotransmission in the gastrointestinal tract. Acta Histochem Cytochem. 2006;39:145-153. [Cited in This Article: ] |
| 39. | Fox EA, Phillips RJ, Martinson FA, Baronowsky EA, Powley TL. Vagal afferent innervation of smooth muscle in the stomach and duodenum of the mouse: morphology and topography. J Comp Neurol. 2000;428:558-576. [Cited in This Article: ] |
| 40. | Horiguchi K, Semple GS, Sanders KM, Ward SM. Distribution of pacemaker function through the tunica muscularis of the canine gastric antrum. J Physiol. 2001;537:237-250. [Cited in This Article: ] |
| 41. | Hirst GD. An additional role for ICC in the control of gastrointestinal motility? J Physiol. 2001;537:1. [Cited in This Article: ] |
| 42. | Huizinga JD. Gastrointestinal peristalsis: joint action of enteric nerves, smooth muscle, and interstitial cells of Cajal. Microsc Res Tech. 1999;47:239-247. [Cited in This Article: ] |
| 43. | Tonini M, Costa M, Brookes SJ, Humphreys CM. Dissociation of the ascending excitatory reflex from peristalsis in the guinea-pig small intestine. Neuroscience. 1996;73:287-297. [Cited in This Article: ] |
| 44. | Huizinga JD, Thuneberg L, Vanderwinden JM, Rumessen JJ. Interstitial cells of Cajal as targets for pharmacological intervention in gastrointestinal motor disorders. Trends Pharmacol Sci. 1997;18:393-403. [Cited in This Article: ] |
| 45. | Sanders KM, Ordög T, Ward SM. Physiology and pathophysiology of the interstitial cells of Cajal: from bench to bedside. IV. Genetic and animal models of GI motility disorders caused by loss of interstitial cells of Cajal. Am J Physiol Gastrointest Liver Physiol. 2002;282:G747-G756. [Cited in This Article: ] |
| 46. | Lee HK, Sanders KM. Comparison of ionic currents from interstitial cells and smooth muscle cells of canine colon. J Physiol. 1993;460:135-152. [Cited in This Article: ] |
| 47. | Ward SM, Ordog T, Koh SD, Baker SA, Jun JY, Amberg G, Monaghan K, Sanders KM. Pacemaking in interstitial cells of Cajal depends upon calcium handling by endoplasmic reticulum and mitochondria. J Physiol. 2000;525 Pt 2:355-361. [Cited in This Article: ] |
| 48. | Koh SD, Jun JY, Kim TW, Sanders KM. A Ca(2+)-inhibited non-selective cation conductance contributes to pacemaker currents in mouse interstitial cell of Cajal. J Physiol. 2002;540:803-814. [Cited in This Article: ] |
| 49. | Hirst GD, Edwards FR. Generation of slow waves in the antral region of guinea-pig stomach--a stochastic process. J Physiol. 2001;535:165-180. [Cited in This Article: ] |
| 50. | Dickens EJ, Hirst GD, Tomita T. Identification of rhythmically active cells in guinea-pig stomach. J Physiol. 1999;514:515-531. [Cited in This Article: ] |
| 51. | Suzuki H, Hirst GD. Regenerative potentials evoked in circular smooth muscle of the antral region of guinea-pig stomach. J Physiol. 1999;517:563-573. [Cited in This Article: ] |
| 52. | Suzuki H, Ward SM, Bayguinov YR, Edwards FR, Hirst GD. Involvement of intramuscular interstitial cells in nitrergic inhibition in the mouse gastric antrum. J Physiol. 2003;546:751-763. [Cited in This Article: ] |
| 53. | Edwards FR, Hirst GD, Suzuki H. Unitary nature of regenerative potentials recorded from circular smooth muscle of guinea-pig antrum. J Physiol. 1999;519 Pt 1:235-250. [Cited in This Article: ] |
| 54. | Hudson N, Mayhew I, Pearson G. A reduction in interstitial cells of Cajal in horses with equine dysautonomia (grass sickness). Auton Neurosci. 2001;92:37-44. [Cited in This Article: ] |
| 55. | Long QL, Fang DC, Shi HT, Luo YH. Gastro-electric dysrhythm and lack of gastric interstitial cells of cajal. World J Gastroenterol. 2004;10:1227-1230. [Cited in This Article: ] |
| 56. | Rolle U, Piotrowska AP, Nemeth L, Puri P. Altered distribution of interstitial cells of Cajal in Hirschsprung disease. Arch Pathol Lab Med. 2002;126:928-933. [Cited in This Article: ] |
| 57. | Zárate N, Mearin F, Wang XY, Hewlett B, Huizinga JD, Malagelada JR. Severe idiopathic gastroparesis due to neuronal and interstitial cells of Cajal degeneration: pathological findings and management. Gut. 2003;52:966-970. [Cited in This Article: ] |
| 58. | Fintl C, Hudson NP, Mayhew IG, Edwards GB, Proudman CJ, Pearson GT. Interstitial cells of Cajal (ICC) in equine colic: an immunohistochemical study of horses with obstructive disorders of the small and large intestines. Equine Vet J. 2004;36:474-479. [Cited in This Article: ] |
| 59. | Vanderwinden JM, Rumessen JJ. Interstitial cells of Cajal in human gut and gastrointestinal disease. Microsc Res Tech. 1999;47:344-360. [Cited in This Article: ] |
| 60. | Torihashi S, Horisawa M, Watanabe Y. c-Kit immunoreactive interstitial cells in the human gastrointestinal tract. J Auton Nerv Syst. 1999;75:38-50. [Cited in This Article: ] |
| 61. | Kraichely RE, Farrugia G. Achalasia: physiology and etiopathogenesis. Dis Esophagus. 2006;19:213-223. [Cited in This Article: ] |
| 62. | Negreanu LM, Assor P, Mateescu B, Cirstoiu C. Interstitial cells of Cajal in the gut--a gastroenterologist's point of view. World J Gastroenterol. 2008;14:6285-6288. [Cited in This Article: ] |
| 63. | Richardson BJ, Welch RW. Differential effect of atropine on rightward and leftward lower esophageal sphincter pressure. Gastroenterology. 1981;81:85-89. [Cited in This Article: ] |
| 64. | Ward SM, Morris G, Reese L, Wang XY, Sanders KM. Interstitial cells of Cajal mediate enteric inhibitory neurotransmission in the lower esophageal and pyloric sphincters. Gastroenterology. 1998;115:314-329. [Cited in This Article: ] |
| 65. | Faussone-Pellegrini MS, Cortesini C. The muscle coat of the lower esophageal sphincter in patients with achalasia and hypertensive sphincter. An electron microscopic study. J Submicrosc Cytol. 1985;17:673-685. [Cited in This Article: ] |
| 66. | Myers NA, Jolley SG, Taylor R. Achalasia of the cardia in children: a worldwide survey. J Pediatr Surg. 1994;29:1375-1379. [Cited in This Article: ] |
| 67. | Allgrove J, Clayden GS, Grant DB, Macaulay JC. Familial glucocorticoid deficiency with achalasia of the cardia and deficient tear production. Lancet. 1978;1:1284-1286. [Cited in This Article: ] |
| 68. | Moore PS, Couch RM, Perry YS, Shuckett EP, Winter JS. Allgrove syndrome: an autosomal recessive syndrome of ACTH insensitivity, achalasia and alacrima. Clin Endocrinol (Oxf). 1991;34:107-114. [Cited in This Article: ] |
| 69. | Dugardeyn C, Anooshiravani M, Christophe C, Goyens P, Perlmutter N. Achalasia-alacrima-ACTH insensitivity syndrome (Triple-A-syndrome). J Belge Radiol. 1993;76:167-168. [Cited in This Article: ] |
| 70. | Weber A, Wienker TF, Jung M, Easton D, Dean HJ, Heinrichs C, Reis A, Clark AJ. Linkage of the gene for the triple A syndrome to chromosome 12q13 near the type II keratin gene cluster. Hum Mol Genet. 1996;5:2061-2066. [Cited in This Article: ] |
| 71. | Lui H, Vanderwinden JM, Ji P, De Laet MH. Nitric oxide synthase distribution in the enteric nervous system of children with cardiac achalasia. Chin Med J (Engl). 1997;110:358-361. [Cited in This Article: ] |
| 72. | Yamagishi H, Koike T, Ohara S, Kobayashi S, Ariizumi K, Abe Y, Iijima K, Imatani A, Inomata Y, Kato K. Prevalence of gastroesophageal reflux symptoms in a large unselected general population in Japan. World J Gastroenterol. 2008;14:1358-1364. [Cited in This Article: ] |
| 73. | Kaltenbach T, Crockett S, Gerson LB. Are lifestyle measures effective in patients with gastroesophageal reflux disease? An evidence-based approach. Arch Intern Med. 2006;166:965-971. [Cited in This Article: ] |
| 74. | Dickens EJ, Edwards FR, Hirst GD. Selective knockout of intramuscular interstitial cells reveals their role in the generation of slow waves in mouse stomach. J Physiol. 2001;531:827-833. [Cited in This Article: ] |
| 75. | Ward SM, Sanders KM. Physiology and pathophysiology of the interstitial cell of Cajal: from bench to bedside. I. Functional development and plasticity of interstitial cells of Cajal networks. Am J Physiol Gastrointest Liver Physiol. 2001;281:G602-G611. [Cited in This Article: ] |
| 76. | Shafik A, El-Sibai O, Shafik I, Shafik A. Electroesophagogram in gastroesophageal reflux disease with a new theory on the pathogenesis of its electric changes. BMC Surg. 2004;4:13. [Cited in This Article: ] |
| 77. | Vittal H, Farrugia G, Gomez G, Pasricha PJ. Mechanisms of disease: the pathological basis of gastroparesis--a review of experimental and clinical studies. Nat Clin Pract Gastroenterol Hepatol. 2007;4:336-346. [Cited in This Article: ] |
| 78. | Abell TL, Malinowski S, Minocha A. Nutrition aspects of gastroparesis and therapies for drug-refractory patients. Nutr Clin Pract. 2006;21:23-33. [Cited in This Article: ] |
| 79. | Forster J, Damjanov I, Lin Z, Sarosiek I, Wetzel P, McCallum RW. Absence of the interstitial cells of Cajal in patients with gastroparesis and correlation with clinical findings. J Gastrointest Surg. 2005;9:102-108. [Cited in This Article: ] |
| 80. | Reddymasu SC, McCallum RW. Pharmacotherapy of gastroparesis. Expert Opin Pharmacother. 2009;10:469-484. [Cited in This Article: ] |
| 81. | Hirst GD, Edwards FR. Role of interstitial cells of Cajal in the control of gastric motility. J Pharmacol Sci. 2004;96:1-10. [Cited in This Article: ] |
| 82. | Hayes MA, Goldenberg IS. The problems of infantile pyloric stenosis. Surg Gynecol Obstet. 1957;104:105-138. [Cited in This Article: ] |
| 83. | Rogers IM. The enigma of pyloric stenosis. Some thoughts on the aetiology. Acta Paediatr. 1997;86:6-9. [Cited in This Article: ] |
| 84. | Mitchell LE, Risch N. The genetics of infantile hypertrophic pyloric stenosis. A reanalysis. Am J Dis Child. 1993;147:1203-1211. [Cited in This Article: ] |
| 85. | Rollins MD, Shields MD, Quinn RJ, Wooldridge MA. Pyloric stenosis: congenital or acquired? Arch Dis Child. 1989;64:138-139. [Cited in This Article: ] |
| 86. | Lynn HB. The mechanism of pyloric stenosis and its relationship to preoperative preparation. Arch Surg. 1960;81:453-459. [Cited in This Article: ] |
| 87. | Yamashiro Y, Mayama H, Yamamoto K, Sato M, Nawate G. Conservative management of infantile pyloric stenosis by nasoduodenal feeding. Eur J Pediatr. 1981;136:187-192. [Cited in This Article: ] |
| 88. | Ukabiala O, Lister J. The extent of muscle hypertrophy in infantile hypertrophic pyloric stenosis does not depend on age and duration of symptoms. J Pediatr Surg. 1987;22:200-202. [Cited in This Article: ] |
| 89. | Kobayashi H, O'Briain DS, Puri P. Immunochemical characterization of neural cell adhesion molecule (NCAM), nitric oxide synthase, and neurofilament protein expression in pyloric muscle of patients with pyloric stenosis. J Pediatr Gastroenterol Nutr. 1995;20:319-325. [Cited in This Article: ] |
| 90. | Schröder JM, Dieler R, Skopnik H, Steinau G. Immunohistochemical reactivity of neuropeptides in plastic-embedded semithin sections of the myenteric plexus in infantile hypertrophic pylorus stenosis. Acta Histochem Suppl. 1992;42:341-344. [Cited in This Article: ] |
| 91. | Wattchow DA, Cass DT, Furness JB, Costa M, O'Brien PE, Little KE, Pitkin J. Abnormalities of peptide-containing nerve fibers in infantile hypertrophic pyloric stenosis. Gastroenterology. 1987;92:443-448. [Cited in This Article: ] |
| 92. | Vanderwinden JM, Mailleux P, Schiffmann SN, Vanderhaeghen JJ, De Laet MH. Nitric oxide synthase activity in infantile hypertrophic pyloric stenosis. N Engl J Med. 1992;327:511-515. [Cited in This Article: ] |
| 93. | Tam PK. Observations and perspectives of the pathology and possible aetiology of infantile hypertrophic pyloric stenosis--a histological, biochemical, histochemical and immunocytochemical study. Ann Acad Med Singapore. 1985;14:523-529. [Cited in This Article: ] |
| 94. | Langer JC, Berezin I, Daniel EE. Hypertrophic pyloric stenosis: ultrastructural abnormalities of enteric nerves and the interstitial cells of Cajal. J Pediatr Surg. 1995;30:1535-1543. [Cited in This Article: ] |
| 95. | Vanderwinden JM, Liu H, De Laet MH, Vanderhaeghen JJ. Study of the interstitial cells of Cajal in infantile hypertrophic pyloric stenosis. Gastroenterology. 1996;111:279-288. [Cited in This Article: ] |
| 96. | Yamataka A, Fujiwara T, Kato Y, Okazaki T, Sunagawa M, Miyano T. Lack of intestinal pacemaker (C-KIT-positive) cells in infantile hypertrophic pyloric stenosis. J Pediatr Surg. 1996;31:96-98; discussion 98-99. [Cited in This Article: ] |
| 97. | Huang PL, Dawson TM, Bredt DS, Snyder SH, Fishman MC. Targeted disruption of the neuronal nitric oxide synthase gene. Cell. 1993;75:1273-1286. [Cited in This Article: ] |
| 98. | Meier-Ruge W, Gambazzi F, Käufeler RE, Schmid P, Schmidt CP. The neuropathological diagnosis of neuronal intestinal dysplasia (NID B). Eur J Pediatr Surg. 1994;4:267-273. [Cited in This Article: ] |
| 99. | Kubota M, Ito Y, Ikeda K. Membrane properties and innervation of smooth muscle cells in Hirschsprung's disease. Am J Physiol. 1983;244:G406-G415. [Cited in This Article: ] |
| 100. | Yamataka A, Kato Y, Tibboel D, Murata Y, Sueyoshi N, Fujimoto T, Nishiye H, Miyano T. A lack of intestinal pacemaker (c-kit) in aganglionic bowel of patients with Hirschsprung's disease. J Pediatr Surg. 1995;30:441-444. [Cited in This Article: ] |
| 101. | Horisawa M, Watanabe Y, Torihashi S. Distribution of c-Kit immunopositive cells in normal human colon and in Hirschsprung's disease. J Pediatr Surg. 1998;33:1209-1214. [Cited in This Article: ] |
| 102. | Young HM, Ciampoli D, Southwell BR, Newgreen DF. Origin of interstitial cells of Cajal in the mouse intestine. Dev Biol. 1996;180:97-107. [Cited in This Article: ] |
| 103. | Bidaud C, Salomon R, Van Camp G, Pelet A, Attié T, Eng C, Bonduelle M, Amiel J, Nihoul-Fékété C, Willems PJ. Endothelin-3 gene mutations in isolated and syndromic Hirschsprung disease. Eur J Hum Genet. 1997;5:247-251. [Cited in This Article: ] |
| 104. | Kapur RP. Contemporary approaches toward understanding the pathogenesis of Hirschsprung disease. Pediatr Pathol. 1993;13:83-100. [Cited in This Article: ] |
| 105. | Dow E, Cross S, Wolgemuth DJ, Lyonnet S, Mulligan LM, Mascari M, Ladda R, Williamson R. Second locus for Hirschsprung disease/Waardenburg syndrome in a large Mennonite kindred. Am J Med Genet. 1994;53:75-80. [Cited in This Article: ] |
| 106. | Meier-Ruge W. [Casuistic of colon disorder with symptoms of Hirschsprung's disease (author's transl)]. Verh Dtsch Ges Pathol. 1971;55:506-510. [Cited in This Article: ] |
| 107. | Fadda B, Maier WA, Meier-Ruge W, Schärli A, Daum R. [Neuronal intestinal dysplasia. Critical 10-years' analysis of clinical and biopsy diagnosis]. Z Kinderchir. 1983;38:305-311. [Cited in This Article: ] |
| 108. | Puri P. Intestinal neuronal dysplasia. Semin Pediatr Surg. 2003;12:259-264. [Cited in This Article: ] |
| 109. | Rolle U, Piaseczna-Piotrowska A, Puri P. Interstitial cells of Cajal in the normal gut and in intestinal motility disorders of childhood. Pediatr Surg Int. 2007;23:1139-1152. [Cited in This Article: ] |
| 110. | De Giorgio R, Sarnelli G, Corinaldesi R, Stanghellini V. Advances in our understanding of the pathology of chronic intestinal pseudo-obstruction. Gut. 2004;53:1549-1552. [Cited in This Article: ] |
| 111. | Rudolph CD, Hyman PE, Altschuler SM, Christensen J, Colletti RB, Cucchiara S, Di Lorenzo C, Flores AF, Hillemeier AC, McCallum RW. Diagnosis and treatment of chronic intestinal pseudo-obstruction in children: report of consensus workshop. J Pediatr Gastroenterol Nutr. 1997;24:102-112. [Cited in This Article: ] |
| 112. | Krishnamurthy S, Heng Y, Schuffler MD. Chronic intestinal pseudo-obstruction in infants and children caused by diverse abnormalities of the myenteric plexus. Gastroenterology. 1993;104:1398-1408. [Cited in This Article: ] |
| 113. | Anuras S, Mitros FA, Soper RT, Pringle KC, Maves BV, Younoszai MK, Franken EA Jr, Whitington P. Chronic intestinal pseudoobstruction in young children. Gastroenterology. 1986;91:62-70. [Cited in This Article: ] |
| 114. | Smith VV, Milla PJ. Histological phenotypes of enteric smooth muscle disease causing functional intestinal obstruction in childhood. Histopathology. 1997;31:112-122. [Cited in This Article: ] |
| 115. | Bassotti G, Chistolini F, Nzepa FS, Morelli A. Colonic propulsive impairment in intractable slow-transit constipation. Arch Surg. 2003;138:1302-1304. [Cited in This Article: ] |
| 116. | Camilleri M, Thompson WG, Fleshman JW, Pemberton JH. Clinical management of intractable constipation. Ann Intern Med. 1994;121:520-528. [Cited in This Article: ] |
| 117. | Locke GR 3rd. The epidemiology of functional gastrointestinal disorders in North America. Gastroenterol Clin North Am. 1996;25:1-19. [Cited in This Article: ] |
| 118. | Locke GR 3rd, Pemberton JH, Phillips SF. AGA technical review on constipation. American Gastroenterological Association. Gastroenterology. 2000;119:1766-1778. [Cited in This Article: ] |
| 119. | Nyam DC, Pemberton JH. Long-term results of lateral internal sphincterotomy for chronic anal fissure with particular reference to incidence of fecal incontinence. Dis Colon Rectum. 1999;42:1306-1310. [Cited in This Article: ] |
| 120. | Tong WD, Liu BH, Zhang LY, Zhang SB. Analysis of the c-kit gene in patients with slow transit constipation. Gut. 2006;55:1207-1208. [Cited in This Article: ] |
| 121. | Lyford GL, He CL, Soffer E, Hull TL, Strong SA, Senagore AJ, Burgart LJ, Young-Fadok T, Szurszewski JH, Farrugia G. Pan-colonic decrease in interstitial cells of Cajal in patients with slow transit constipation. Gut. 2002;51:496-501. [Cited in This Article: ] |
| 122. | Schiller LR. New and emerging treatment options for chronic constipation. Rev Gastroenterol Disord. 2004;4 Suppl 2:S43-S51. [Cited in This Article: ] |
| 123. | Shafik A, Shafik AA, El-Sibai O, Mostafa RM. Electric activity of the colon in subjects with constipation due to total colonic inertia: an electrophysiologic study. Arch Surg. 2003;138:1007-1011; discussion 1011. [Cited in This Article: ] |
| 124. | D'Amato G, Steinert DM, McAuliffe JC, Trent JC. Update on the biology and therapy of gastrointestinal stromal tumors. Cancer Control. 2005;12:44-56. [Cited in This Article: ] |
| 125. | Erlandson RA, Klimstra DS, Woodruff JM. Subclassification of gastrointestinal stromal tumors based on evaluation by electron microscopy and immunohistochemistry. Ultrastruct Pathol. 1996;20:373-393. [Cited in This Article: ] |
| 126. | Saul SH, Rast ML, Brooks JJ. The immunohistochemistry of gastrointestinal stromal tumors. Evidence supporting an origin from smooth muscle. Am J Surg Pathol. 1987;11:464-473. [Cited in This Article: ] |
| 127. | Mikami T, Terada T, Nakamura K, Okayasu I. The gastric hypercellular microleiomyoma as a precursor lesion for clinical gastrointestinal stromal tumors. Hum Pathol. 1997;28:1355-1360. [Cited in This Article: ] |
| 128. | Sakurai S, Fukasawa T, Chong JM, Tanaka A, Fukayama M. Embryonic form of smooth muscle myosin heavy chain (SMemb/MHC-B) in gastrointestinal stromal tumor and interstitial cells of Cajal. Am J Pathol. 1999;154:23-28. [Cited in This Article: ] |
| 129. | Monihan JM, Carr NJ, Sobin LH. CD34 immunoexpression in stromal tumours of the gastrointestinal tract and in mesenteric fibromatoses. Histopathology. 1994;25:469-473. [Cited in This Article: ] |
| 130. | Miettinen M, Sarlomo-Rikala M, Lasota J. Gastrointestinal stromal tumours. Ann Chir Gynaecol. 1998;87:278-281. [Cited in This Article: ] |
| 131. | Silverman JS, Tamsen A. Mammary fibroadenoma and some phyllodes tumour stroma are composed of CD34+ fibroblasts and factor XIIIa+ dendrophages. Histopathology. 1996;29:411-419. [Cited in This Article: ] |
| 132. | Chaubal A, Paetau A, Zoltick P, Miettinen M. CD34 immunoreactivity in nervous system tumors. Acta Neuropathol. 1994;88:454-458. [Cited in This Article: ] |
| 133. | Kindblom LG, Remotti HE, Aldenborg F, Meis-Kindblom JM. Gastrointestinal pacemaker cell tumor (GIPACT): gastrointestinal stromal tumors show phenotypic characteristics of the interstitial cells of Cajal. Am J Pathol. 1998;152:1259-1269. [Cited in This Article: ] |
| 134. | Sarlomo-Rikala M, Kovatich AJ, Barusevicius A, Miettinen M. CD117: a sensitive marker for gastrointestinal stromal tumors that is more specific than CD34. Mod Pathol. 1998;11:728-734. [Cited in This Article: ] |
| 135. | Nakahara M, Isozaki K, Hirota S, Miyagawa J, Hase-Sawada N, Taniguchi M, Nishida T, Kanayama S, Kitamura Y, Shinomura Y. A novel gain-of-function mutation of c-kit gene in gastrointestinal stromal tumors. Gastroenterology. 1998;115:1090-1095. [Cited in This Article: ] |
| 136. | Lasota J, Jasinski M, Sarlomo-Rikala M, Miettinen M. Mutations in exon 11 of c-Kit occur preferentially in malignant versus benign gastrointestinal stromal tumors and do not occur in leiomyomas or leiomyosarcomas. Am J Pathol. 1999;154:53-60. [Cited in This Article: ] |
| 137. | Hirota S, Isozaki K, Moriyama Y, Hashimoto K, Nishida T, Ishiguro S, Kawano K, Hanada M, Kurata A, Takeda M. Gain-of-function mutations of c-kit in human gastrointestinal stromal tumors. Science. 1998;279:577-580. [Cited in This Article: ] |
| 138. | Ernst SI, Hubbs AE, Przygodzki RM, Emory TS, Sobin LH, O'Leary TJ. KIT mutation portends poor prognosis in gastrointestinal stromal/smooth muscle tumors. Lab Invest. 1998;78:1633-1636. [Cited in This Article: ] |
| 139. | Yamaura K, Kato K, Miyazawa M, Haba Y, Muramatsu A, Miyata K, Koide N. Stromal tumor of the pancreas with expression of c-kit protein: report of a case. J Gastroenterol Hepatol. 2004;19:467-470. [Cited in This Article: ] |
| 140. | Nakagawa M, Akasaka Y, Kanai T, Yamashita T, Kuroda M, Takayama H, Miyazawa N. Extragastrointestinal stromal tumor of the greater omentum: case report and review of the literature. Hepatogastroenterology. 2003;50:691-695. [Cited in This Article: ] |
| 141. | de Silva CM, Reid R. Gastrointestinal stromal tumors (GIST): C-kit mutations, CD117 expression, differential diagnosis and targeted cancer therapy with Imatinib. Pathol Oncol Res. 2003;9:13-19. [Cited in This Article: ] |