Published online Feb 28, 2009. doi: 10.3748/wjg.15.1010
Revised: January 4, 2009
Accepted: January 11, 2009
Published online: February 28, 2009
Solitary pancreatic involvement of tuberculosis is rare, especially in an immunocompetent individual, and it may be misdiagnosed as pancreatic cystic neoplasms. Pancreatic cystic neoplasms are being identified in increasing numbers, probably because of the frequent use of radiology and advances in endoscopic techniques. However, they are composed of a variety of neoplasms with a wide range of malignant potential, and it is often difficult to differentiate pancreatic tuberculosis mimicking cystic neoplasms from benign or malignant pancreatic cystic neoplasms. Non-surgical diagnosis of pancreatic tuberculosis is inconclusive and continues to be a challenge in many cases. If so, then laparotomy should be employed to establish the diagnosis. Therefore, pancreatic tuberculosis should be kept in mind during the differential diagnosis of solitary cystic masses in the pancreas. We report a patient who had solitary pancreatic tuberculosis masquerading as pancreatic serous cystadenoma.
- Citation: Hong SG, Kim JS, Joo MK, Lee KG, Kim KH, Oh CR, Park JJ, Bak YT. Pancreatic tuberculosis masquerading as pancreatic serous cystadenoma. World J Gastroenterol 2009; 15(8): 1010-1013
- URL: https://www.wjgnet.com/1007-9327/full/v15/i8/1010.htm
- DOI: https://dx.doi.org/10.3748/wjg.15.1010
Pancreatic tuberculosis is uncommon and isolated involvement is rare. Pancreatic tuberculosis is a well-known masquerader, and the diverse clinical and radiological picture of this chronic infection may be revealed as a variable pancreatic lesion, including pancreatic cystic neoplasm, such as serous cystadenoma. In view of the non-specific presentation and imaging appearance of the disease, a high index of suspicion is required to obtain a preoperative diagnosis. However, the diagnosis is usually established at laparotomy. Herein, we describe one case of solitary pancreatic tuberculosis that presented as a lobulated multicystic neoplasm that resembled serous cystadenoma.
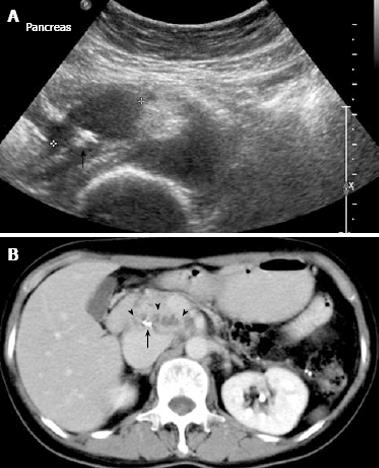
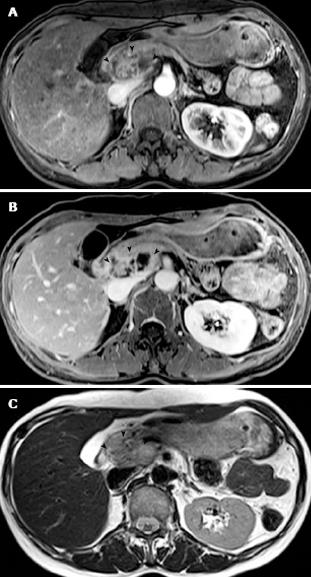
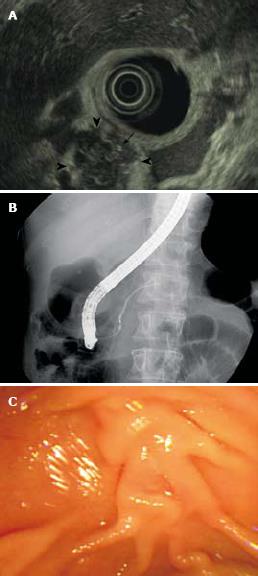
A 51-year-old woman was referred from another hospital for further management of a pancreatic head tumor detected on an abdominal ultrasound scan. On admission, the patient appeared to be in excellent condition. She presented with mild epigastric discomfort which had persisted for 2 wk. She had no tenderness over the epigastric area and no definite mass was palpable. Other physical examination findings were unremarkable. According to the patients’ history, she had no coughing, fever, jaundice, diarrhea, hematemesis or melena. There was no prior history of pancreatitis, liver disease, alcohol use, tuberculosis or malignancy in the patient or her family. Initial laboratory values revealed: white blood cell count, 6.9 × 109/L; hemoglobin, 11.4 g/dL; aspartate aminotransferase, 19 IU/L (reference range, 10-44 IU/L); alanine aminotransferase, 6 IU/L (12-79 IU/L); total bilirubin, 0.9 mg/dL (0.2-1.3 mg/dL); albumin, 4.0 g/dL (3.3-5.1 g/dL); alkaline phosphatase, 8 IU/L (42-136 IU/L); amylase, 69 U/dL (28-100 U/dL); and lipase, 80.3 U/dL (10-150 U/dL). Serological tests for antibodies to hepatitis B virus surface antigen, hepatitis C virus, and human immunodeficiency virus yielded negative results. Other blood tests were normal, except for an elevated erythrocyte sedimentation rate (99 mm/h). Levels of carbohydrate antigen 19-9 and carcinoembryonic antigen were within normal limits. A chest radiograph exhibited no abnormal findings. Abdominal ultrasound (US) examination revealed an irregularly contoured, hypoechoic, cystic lesion in the head of the pancreas, with calcification at the center of the mass and no dilation of the bile duct system or the pancreatic duct (Figure 1A). Contrast-enhanced computerized tomography (CT) of the abdomen showed an inhomogeneous lobulated multicystic mass of 4.5 cm × 2.0 cm in the head and uncinate process of the pancreas, with central calcification (Figure 1B). Subsequent magnetic resonance imaging (MRI) revealed a sharply delineated multiloculated mass in the pancreas head with peripheral and central areas of enhancement on a gadolinium-enhanced T-1 weighted image (Figure 2A and B). On the T-2 weighted image, a heterogeneous mass with areas of increased and decreased signal intensities was noted (Figure 2C). Endoscopic US also demonstrated a lobulated multicystic lesion of heterogeneous echotexture (Figure 3A). Endoscopic retrograde cholangiopancreatography (ERCP) showed a normal appearance of the ampulla and no mucus secretion from its orifice (Figure 3B). There was no communication between the pancreatic duct and the cystic mass (Figure 3C). After completing these investigations, the principal provisional diagnosis of the lesion was a cystic neoplasm of the pancreas, such as serous cystadenoma.
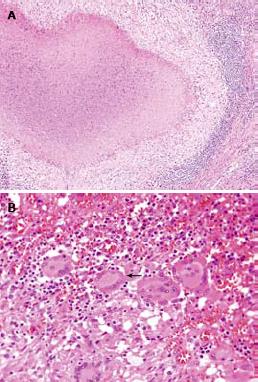
We planned close observation and follow-up by regular surveillance imaging because malignant transformation of serous cystadenoma is exceedingly rare. However, the patient and her family preferred removal of the lesion because they were concerned about its malignant potential. She underwent a pylorus-preserving Whipple’s operation (pancreaticoduodenectomy). The operation revealed a firm mass in the head of the pancreas, approximately 6.5 cm × 4.0 cm × 3.8 cm in size, and lymphadenopathy. Histological examination of the resected specimen showed caseating granulomas and the presence of Langhans’ giant cells, which was suggestive of tuberculosis in the pancreatic head and lymph nodes, and polymerase chain reaction for tuberculosis was positive (Figure 4). Following the histological diagnosis of pancreatic tuberculosis, the patient was successfully treated with antituberculous therapy. The patient is doing well and has experienced no further abdominal discomfort.
Tuberculosis is still a common illness worldwide. Dissemination to the gastrointestinal tract, liver, spleen and mesenteric lymph nodes is common in abdominal and military tuberculosis in developing countries. Although extra-pulmonary tuberculosis is an emerging clinical problem, it rarely affects the pancreas.
Pancreatic tuberculosis usually occurs as a complication of miliary tuberculosis in immunodeficient individuals. Isolated involvement of the pancreas is exceedingly rare worldwide[12]. It presents radiologically with variable manifestations, with a wide spectrum of symptoms, and can mimic pancreatic cystic neoplasm[3]. CT may show an enlarged pancreas with focal hypodense lesions and irregular borders, sometimes with an irregular multilobular cyst in the head region or enlarged peripancreatic lymph nodes[4]. In contrast-enhanced CT, this well-defined mass may show irregular margins with peripheral enhancement and multiloculated appearance of central enhancement. These features, however, are non-specific and may resemble those of neoplastic cystic lesions of the pancreas. The MRI features of focal tuberculosis of the pancreas show a sharply delineated mass located in the pancreatic head, which shows heterogeneous enhancement[5]. However, there are no radiological features that are pathognomonic of tuberculosis. The diagnosis usually is not suspected before laparotomy unless there is evidence of tuberculosis elsewhere, or a relevant clinical history[467].
Serous cystadenoma, also known as microcystic adenoma, is usually a benign pancreatic neoplasm that occurs most often in women and is typically diagnosed during the sixth to ninth decades of life[8]. Usually small (< 2 cm) and microcystic, they may grow to be quite large. The most common feature of serous cystadenoma is a polycystic pattern. The cystic lesion has many loculi, thin septa, external lobulation, and central scarring with stellate calcification upon CT[9]. External lobulation and a central scar, with or without a stellate pattern of calcification, are two important morphological features. The presence of a central scar visualized with the use of CT or MRI is a highly diagnostic feature that is found in about 30% of serous cystadenomas. The finding of multiple small (< 3 mm) compartments within a cystic lesion in endoscopic ultrasound images is suggestive of serous cystadenoma[10]. A cyst with a central stellate scar is considered virtually diagnostic of a serous cystadenoma.
This radiological appearance of pancreatic cystic tumors is excellent and, owing to recent improvements in pancreatic imaging, increasing numbers of cystic lesions have been identified in asymptomatic patients. However, the pancreatic imaging is imperfect, and hence may not be diagnostic of serous cystadenoma.
In our patient, the non-specific clinical and laboratory investigations, combined with a lobulated, multicystic pancreatic mass with focal calcification upon radiological imaging may lead to an erroneous primary diagnosis of serous cystadenoma. We conclude that pancreatic tuberculosis should be considered in the differential diagnosis of solitary pancreatic cystic lesions, even in healthy patients.
| 1. | Liu Q, He Z, Bie P. Solitary pancreatic tuberculous abscess mimicking prancreatic cystadenocarcinoma: a case report. BMC Gastroenterol. 2003;3:1. [Cited in This Article: ] |
| 2. | Evans JD, Hamanaka Y, Olliff SP, Neoptolemos JP. Tuberculosis of the pancreas presenting as metastatic pancreatic carcinoma. A case report and review of the literature. Dig Surg. 2000;17:183-187. [Cited in This Article: ] |
| 3. | Cheng J, Tadi K, Halpern M, Feurdean M, McNelis J, Brensilver J. Pancreatic tuberculosis in a human immuno-deficiency virus positive patient: a case report. World J Gastroenterol. 2008;14:939-940. [Cited in This Article: ] |
| 4. | Saluja SS, Ray S, Pal S, Kukeraja M, Srivastava DN, Sahni P, Chattopadhyay TK. Hepatobiliary and pancreatic tuberculosis: a two decade experience. BMC Surg. 2007;7:10. [Cited in This Article: ] |
| 5. | De Backer AI, Mortele KJ, Bomans P, De Keulenaer BL, Vanschoubroeck IJ, Kockx MM. Tuberculosis of the pancreas: MRI features. AJR Am J Roentgenol. 2005;184:50-54. [Cited in This Article: ] |
| 6. | Ahlawat SK, Charabaty-Pishvaian A, Lewis JH, Haddad NG. Pancreatic tuberculosis diagnosed with endoscopic ultrasound guided fine needle aspiration. JOP. 2005;6:598-602. [Cited in This Article: ] |
| 7. | Rezeig MA, Fashir BM, Al-Suhaibani H, Al-Fadda M, Amin T, Eisa H. Pancreatic tuberculosis mimicking pancreatic carcinoma: four case reports and review of the literature. Dig Dis Sci. 1998;43:329-331. [Cited in This Article: ] |
| 8. | Rampy BA, Waxman I, Xiao SY, Logrono R. Serous cystadenoma of the pancreas with papillary features: a diagnostic pitfall on fine-needle aspiration biopsy. Arch Pathol Lab Med. 2001;125:1591-1594. [Cited in This Article: ] |
| 9. | Kim HJ, Lee DH, Ko YT, Lim JW, Kim HC, Kim KW. CT of serous cystadenoma of the pancreas and mimicking masses. AJR Am J Roentgenol. 2008;190:406-412. [Cited in This Article: ] |