Published online Sep 21, 2009. doi: 10.3748/wjg.15.4457
Revised: August 7, 2009
Accepted: August 14, 2009
Published online: September 21, 2009
An iliopsoas hematoma can occur either spontaneously or secondary to trauma or bleeding tendency due to hemophilia and anticoagulant therapy. Although liver cirrhosis is commonly associated with coagulopathy, iliopsoas hematoma is very rare. We herein, present a case of bilateral iliopsoas hematoma in a patient with alcoholic cirrhosis, and review the literature on muscle hematoma associated with cirrhosis. A 56-year-old man with alcoholic cirrhosis was admitted in a state of shock with anemia. The cause of anemia could not be detected, and the patient was treated conservatively. The site of bleeding was not detected with either gastroduodenal endoscopy or upper abdominal computed tomography, the latter of which did not include the iliopsoas muscle. He died on the 10th day of admission and bilateral iliopsoas hematomas were found on autopsy. An iron stain was positive in the iliopsoas muscle. Eight cases of muscle hematoma associated with cirrhosis, including the present case, were found in a review of the literature. Four of these cases involved the rectus abdominis muscle, 3 involved the iliopsoas muscle and 1 involved combined muscles. Alcoholic cirrhosis accounted for 75% of the cases. One case (12.5%) was associated with virus-related cirrhosis, and another with combined virus- and alcohol-related cirrhosis. The mortality rate was 75% despite early diagnosis and low risk scores for cirrhosis. Muscle hematoma in patients with cirrhosis is closely related to alcoholism, and the mortality rate of the condition is extremely high. In conclusion, muscle hematoma should be recognized as an important complication of cirrhosis.
- Citation: Sugiyama C, Akai A, Yamakita N, Ikeda T, Yasuda K. Muscle hematoma: A critically important complication of alcoholic liver cirrhosis. World J Gastroenterol 2009; 15(35): 4457-4460
- URL: https://www.wjgnet.com/1007-9327/full/v15/i35/4457.htm
- DOI: https://dx.doi.org/10.3748/wjg.15.4457
| Case [reference] | Age (yr)/sex | Etiology of cirrhosis | Involved muscle | Laterality | Time to diag from the onset (d) | Time to death from the onset (d) | MELD/ MELD-Na | Treatment | Course |
| #1[7] | 48/F | Alcohol | Rect. abd. | Bil | 14 | Died (autp) | |||
| #2[6] | 46/F | Alcohol | Rect. abd. | Right | < 1 | > 10 | 29/- | Conserve., FFP | Died (autp) |
| #3[8] | 56/M | Alcohol | Rect. abd. | Right | < 1 | Conserve. | Alive | ||
| #4[9] | 58/F | Virus | Rect. abd. | Left | < 1 | Liver transplt & evac | Alive | ||
| #5[10] | 60/M | Alcohol | Iliopsoas | Left | 6 | 29 | 24/29 | Conserve. | Died (autp) |
| #6[8] | 62/M | Alcohol | Iliopsoas | Right | < 1 | 4 | TAE | Died (autp) | |
| #7 (present) | 56/M | Alcohol | Iliopsoas | Bil | 10 | 25/25 | Conserve., FFP | Died (autp) | |
| #8[11] | 60/M | Alcohol + HCV | Gluteus max & biceps femoris & pectralis | Right | < 1 | 150 | 16/16 | Conserve., FFP | Died (autp) |
Liver cirrhosis is commonly associated with coagulopathies, including thrombocytopenia and hypoprothrombinemia, which often cause easy bruising and bleeding[1]. Sudden bleeding from gastrointestinal varices due to portal hypertension is also an established risk of liver cirrhosis. Muscle hematoma usually occurs either traumatically or spontaneously in patients with hemophilia[2] and in patients receiving anticoagulant therapy[3]. However, it is rare in cirrhosis.
We herein, report a case of spontaneous bilateral iliopsoas hematoma in a patient with alcoholic liver cirrhosis. We also include a review of the literature on muscle hematoma associated with cirrhosis. The mortality rate of this condition is extremely high in comparison to that of muscle hematomas in patients with hemophilia or under anticoagulant treatment. These findings characterize muscle hematoma as a clinically important complication of cirrhosis.
A 56-year-old man visited a clinic complaining of severe fatigue. He was found to be in a state of shock with severe anemia and was transferred immediately to our hospital. He had ingested 1.5 L of beer every day for 36 years and alcoholic cirrhosis had been diagnosed.
On arrival, a medical history was impossible to obtain because of his decreased level of consciousness. His body temperature was 35.0°C, his systolic blood pressure was 80 mmHg, and his pulse rate was weak but regular at 62 beats per minute. The abdomen was symmetrical and bowel sounds were weak. On palpation, there was neither rigidity nor tenderness, and no mass was palpable. The psoas position was not observed, and neurological examinations revealed only asterixis. Bilateral leg edema was noted.
The laboratory test results were as follows: white blood cell count, 3300/mm3; hemoglobin, 50 g/L; platelets, 45 000/mm3; albumin, 21 g/L; total bilirubin, 6.4 mg/dL; aspartate aminotransferase/alanine aminotransferase, 58/16 U/L; alkaline phosphatase, 202 U/L; blood urea nitrogen, 32 mg/dL; serum creatinine, 2.1 mg/dL; creatine kinase, 202 U/L; prothrombin time-International Normalized Ratio, 1.48; activated partial thromboplastin time, 31.6 s. Stool samples were positive for occult blood.
A chest X-ray showed cardiomegaly and massive bilateral pleural effusion. Abdominal ultrasonography revealed a dull edge and irregular margins of the liver consistent with cirrhosis. Upper abdominal enhanced computed tomography (CT) also confirmed liver cirrhosis with splenomegaly and massive ascites but did not include the iliopsoas muscle. A gastroduodenal endoscopy did not disclose any hemorrhagic diseases. Further examinations were not performed due to the general deterioration of his condition.
Treatment, including the transfusion of red blood cell concentrate, branched-chain amino acids, and albumin as well as the administration of dopamine hydrochloride and diuretics, was initiated. On the 5th day of admission, imipenem/cilastatin sodium (1 g/d) and gamma globulin (2.5 g/d) were empirically administered for a high fever. On the 8th day, the patient received fresh frozen plasma (FFP) and antithrombin III to treat disseminated intravascular coagulation. Wide ecchymosis appeared on both sides of the patient’s back on the 9th day and he died on the 10th day.
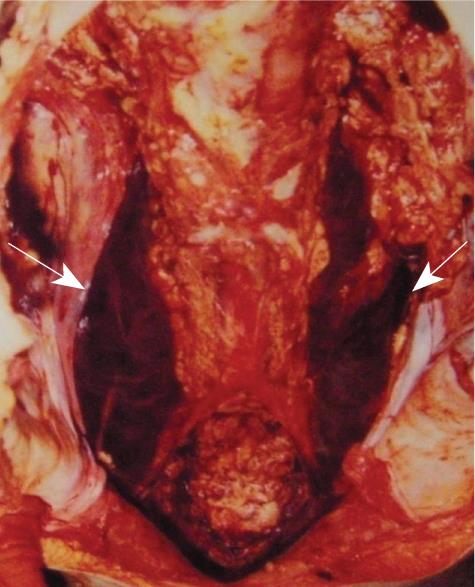
Autopsy findings revealed bilateral iliopsoas hematoma (Figure 1) with liver cirrhosis. The source of bleeding could not be detected inside the iliopsoas muscles, and there was no evidence of either a neoplasm or an arterial anomaly. Other causes of anemia including bone marrow disorders were not detected. A histological examination with iron staining was positive in the iliopsoas muscle. The appearance of this type of staining depends on the age of hemorrhage, and indicated that the bleeding started around the day of admission in this case.
Intramuscular hematoma is classified as either spontaneous or traumatic. Causes of the former include hemorrhagic diseases, neoplasm, and arterial diseases. Iliopsoas and rectus abdominis muscle hematomas are well known as major and well documented complications of hemophilia and anticoagulant therapy[2-5]. Although decreased levels of coagulant factors and thrombocytopenia are often observed in liver cirrhosis, intramuscular hemorrhage is very rare[6].
Early symptoms of an iliopsoas hematoma include groin pain and femoral neuropathy. The present patient was in a drowsy state of consciousness due to shock when he was referred to our hospital. Stools were positive for blood, and therefore, only examinations for upper gastrointestinal tract were performed, and no specific findings were obtained. Unfortunately, the upper abdominal CT scan area did not involve the iliopsoas muscles.
As shown in Table 1, a review of the literature revealed 8 cases of spontaneous muscle hematoma associated with liver cirrhosis, including the present case (Table 1)[6-11]. Of these cases, 4 involved the rectus abdominis muscle[6-9], 3 (including the present case) involved the iliopsoas[8,10], and one involved the gluteus maximus, the biceps femoris and the pectoralis muscles[11]. The mean age of these patients was 55.8 years old. Five of the 8 cases were male (62.5%) and 3 were female (37.5%). Six of the 8 cases were Japanese and the others were Caucasian. Alcoholic cirrhosis accounted for 75% of the cases (6 of 8 cases), and virus-related cirrhosis (virus unknown) and a combination of hepatitis C- and alcohol-related cirrhosis each accounted for 12.5% of the cases (1 each out of 8 cases).
The mortality rate of muscle hematoma associated with cirrhosis was 75% (6 of 8 cases), which is extremely high. All 3 patients with iliopsoas hematoma and 2 of the 4 patients with rectus abdominis muscle hematoma (50%) died. Cherry and Mueller[3] reported that rectus abdominis muscle hematoma is rarely fatal based on a large series of patients from a single institution (mortality rate 1.6%, 2 of 126 cases), most of whom were on various anti-coagulant therapies. Furthermore, the mortality rate of iliopsoas hematoma associated with hemophilia is extremely low after the induction of prophylaxis[2]. According to a review of iliopsoas hematomas in patients receiving intravenous heparin[5], only one of 54 patients (1.9%) died. In these reports, it was generally accepted that early recognition and diagnosis of rectus abdominis and/or iliopsoas hematoma could reduce mortality.
As shown in Table 1, intramuscular hematoma in patients with liver cirrhosis was diagnosed on the day of onset in 6 of the 8 cases (75%). The exceptions included case #5 (diagnosed at 6 d after the onset) and case #7 (the present case, which was diagnosed by autopsy). The Model for End-stage Liver Disease (MELD)[12] and recently reported MELD-Na[13] scores could be calculated in 4 (#2, #5, #7, #8) and 3 (#5, #7, #8) patients, respectively. The mean MELD and MELD-Na scores were 23.5 (range: 16-29) and 23.3 (range: 16-29), respectively, thus suggesting that the probability of death at 90 d (%) ranged from about 4% to 25%[13]. These findings indicate that intramuscular hemorrhage associated with cirrhosis is lethal despite an early diagnosis, even in patients with low MELD or MELD-Na scores.
Huang et al[14] reported interesting findings concerning spontaneous intracranial hemorrhage (SICH) in 4515 hospitalized Chinese cirrhotic patients. Among these patients, 36 experienced SICH and 78% were male. The etiology of cirrhosis included alcoholic cirrhosis in 50% of the patients, virus-related cirrhosis in 27.8%, and combined virus- and alcohol-related cirrhosis in 22.2%. The mean age at onset of SICH in cirrhosis was 53 years. They reported that the overall incidence of SICH in cirrhosis was related to the etiology of cirrhosis, and the incidence of SICH was 6 times higher in alcohol-related cirrhosis than in virus-related cirrhosis. These results are consistent with the present findings on muscle hematoma associated with cirrhosis. It seems likely that a common risk factor, namely alcohol, plays an important role in the promotion of non-variceal hemorrhage in cirrhotic patients. Several actions of alcohol may promote hemorrhage, including the inhibition of platelet adhesion to fibrinogen[15], dose-related ethanol suppression of platelet aggregation induced by extravasation[16], and the promotion of atherosclerosis[17]. However, the participation of these factors in the pathogenesis is still unknown in patients with alcoholic cirrhosis. Among these cases, 6 of 8 were reported in Japan, thus suggesting that intramuscular hematoma and/or SICH with cirrhosis may occur more frequently in Asians that in other ethnicities.
Treatment of muscle hematoma in cirrhotic patients is often challenging. Many factors, including poor general condition due to cirrhosis, lead to poor outcomes. Hematomas might improve with conservative management, as observed in case #3 in Table 1. Zissin et al[18] reported in a literature review that 19 of 26 patients (73%) recovered following transcatheter arterial embolization (TAE) in anticoagulant-related rectus abdominis and iliopsoas hematoma. TAE may be useful for patients in poor condition, although it was unsuccessful in a case of cirrhosis (case #6)[8]. Urgent liver transplantation, which was performed in case #4[9], may be a treatment choice in the future. The bleeding site was detected by angiography in only 1 case of iliopsoas hematoma (#6). In this case, two regions of extravasation of the iliolumbar arterial branches were observed and TAE was performed. In the other cases, the origin of the bleeding could not be detected even at autopsy. This difficulty is one challenge associated with the treatment of this condition. Additional cases could provide further insight into effective treatment methods.
In general, intramuscular hematoma is not mentioned as one of the bleeding complications occurring in cirrhotic patients[1]. Intramuscular hematoma may occur easily by daily motion. For example, a case of rectus abdominis hemorrhage (#3) occurred after an episode of coughing. Taking into account the extremely high mortality rate despite early diagnosis and relatively low risk scores, intramuscular hematoma should be recognized as a rare but clinically important bleeding complication of cirrhosis, especially in cases of alcoholic cirrhosis.
In conclusion, a bilateral iliopsoas hematoma was observed in a patient with alcoholic liver cirrhosis. A review of the literature on intramuscular hemorrhage in cirrhotic patients suggested that alcohol is the common risk factor. In addition, a higher incidence was observed in Asians. This literature review also indicated that muscle hematoma in cases of cirrhosis has a serious prognosis that is quite different from the prognosis of hematomas in patients with hemophilia or under anticoagulant therapy. We should therefore always include muscle hematoma in the differential diagnosis of acute anemia in liver, especially alcoholic, cirrhosis.
Peer reviewer: Devanshi Seth, PhD, Senior Scientist, Centenary Institute & Drug Health Services, RPAH & Clinical Senior Lecturer, Clinical School of Medicine, University of Sydney, Camperdown, NSW 2050, Australia
S- Editor Li LF L- Editor Webster JR E- Editor Yin DH
| 1. | Craxì A, Cammà C, Giunta M. Clinical aspects of bleeding complications in cirrhotic patients. Blood Coagul Fibrinolysis. 2000;11 Suppl 1:S75-S79. [Cited in This Article: ] |
| 2. | Balkan C, Kavakli K, Karapinar D. Iliopsoas haemorrhage in patients with haemophilia: results from one centre. Haemophilia. 2005;11:463-467. [Cited in This Article: ] |
| 3. | Cherry WB, Mueller PS. Rectus sheath hematoma: review of 126 cases at a single institution. Medicine (Baltimore). 2006;85:105-110. [Cited in This Article: ] |
| 4. | Sasson Z, Mangat I, Peckham KA. Spontaneous iliopsoas hematoma in patients with unstable coronary syndromes receiving intravenous heparin in therapeutic doses. Can J Cardiol. 1996;12:490-494. [Cited in This Article: ] |
| 5. | Dauty M, Sigaud M, Trossaërt M, Fressinaud E, Letenneur J, Dubois C. Iliopsoas hematoma in patients with hemophilia: a single-center study. Joint Bone Spine. 2007;74:179-183. [Cited in This Article: ] |
| 6. | Di Bisceglie AM, Richart JM. Spontaneous retroperitoneal and rectus muscle hemorrhage as a potentially lethal complication of cirrhosis. Liver Int. 2006;26:1291-1293. [Cited in This Article: ] |
| 7. | Docherty JG, Herrick AL. Bilateral rectus sheath haematoma complicating alcoholic liver disease. Br J Clin Pract. 1991;45:289. [Cited in This Article: ] |
| 8. | Yoshida H, Tsuji K, Kawakami H, Katanuma A, Sakurai Y, Jong-Hon K, Koizumi K, Mitsui S, Gotoh M, Yoshida A. [Two cases of alcoholic liver cirrhosis associated with intramuscular hematoma]. Nippon Shokakibyo Gakkai Zasshi. 2002;99:1350-1354. [Cited in This Article: ] |
| 9. | Yamamoto S, Sato Y, Takeishi T, Kobayashi T, Watanabe T, Kurosaki I, Hatakeyama K. Liver transplantation in an endostage cirrhosis patient with abdominal compartment syndrome following a spontaneous rectus sheath hematoma. J Gastroenterol Hepatol. 2004;19:118-119. [Cited in This Article: ] |
| 10. | Kamura M, Tanahashi T, Yamakita N, Ikeda T. [A case of idiopathic iliopsoas hematoma associated with liver cirrhosis]. Nippon Shokakibyo Gakkai Zasshi. 1998;95:1266-1269. [Cited in This Article: ] |
| 11. | Tozawa H, Kobayashi S, Muramatsu A, Hasegawa C, Hayakawa T. [A case of alcoholic liver cirrhosis associated with intramuscular hematoma]. Nippon Shokakibyo Gakkai Zasshi. 2006;103:839-843. [Cited in This Article: ] |
| 12. | Malinchoc M, Kamath PS, Gordon FD, Peine CJ, Rank J, ter Borg PC. A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Hepatology. 2000;31:864-871. [Cited in This Article: ] |
| 13. | Kim WR, Biggins SW, Kremers WK, Wiesner RH, Kamath PS, Benson JT, Edwards E, Therneau TM. Hyponatremia and mortality among patients on the liver-transplant waiting list. N Engl J Med. 2008;359:1018-1026. [Cited in This Article: ] |
| 14. | Huang HH, Lin HH, Shih YL, Chen PJ, Chang WK, Chu HC, Chao YC, Hsieh TY. Spontaneous intracranial hemorrhage in cirrhotic patients. Clin Neurol Neurosurg. 2008;110:253-258. [Cited in This Article: ] |
| 15. | de Lange DW, Hijmering ML, Lorsheyd A, Scholman WL, Kraaijenhagen RJ, Akkerman JW, van de Wiel A. Rapid intake of alcohol (binge drinking) inhibits platelet adhesion to fibrinogen under flow. Alcohol Clin Exp Res. 2004;28:1562-1568. [Cited in This Article: ] |
| 16. | Horak JK, Brandon TA, Ribeiro LG, Ware JA, Miller RR, Solis RT. Effects of ethanol and hemolysis on in vivo and in vitro platelet aggregation. J Cardiovasc Pharmacol. 1982;4:1037-1041. [Cited in This Article: ] |
| 17. | Cooper DE, Goff DC Jr, Bell RA, Zaccaro D, Mayer-Davis EJ, Karter AJ. Is insulin sensitivity a causal intermediate in the relationship between alcohol consumption and carotid atherosclerosis?: the insulin resistance and atherosclerosis study. Diabetes Care. 2002;25:1425-1431. [Cited in This Article: ] |
| 18. | Zissin R, Gayer G, Kots E, Ellis M, Bartal G, Griton I. Transcatheter arterial embolisation in anticoagulant-related haematoma--a current therapeutic option: a report of four patients and review of the literature. Int J Clin Pract. 2007;61:1321-1327. [Cited in This Article: ] |