Published online May 28, 2007. doi: 10.3748/wjg.v13.i20.2892
Revised: March 3, 2007
Accepted: March 15, 2007
Published online: May 28, 2007
Adenomyoma is a term generally applied to nodular lesions showing proliferation of both epithelial and smooth muscle components. Despite its benign nature, ampullary adenomyoma is usually presented as biliary obstruction. Most cases are misdiagnosed as carcinoma or adenoma by preoperative endoscopic or radiologic procedure. Therefore, it is frequently treated with extensive surgery. To our knowledge, this is the first reported case in English literature of adenomyoma located in the peripancreatic orifice resulting in intermittent pancreatic duct obstruction and recurrent pancreatitis diagnosed by the endoscopic piecemeal resection.
- Citation: Kwon TH, Park DH, Shim KY, Cho HD, Park JH, Lee SH, Chung IK, Kim HS, Park SH, Kim SJ. Ampullary adenomyoma presenting as acute recurrent pancreatitis. World J Gastroenterol 2007; 13(20): 2892-2894
- URL: https://www.wjgnet.com/1007-9327/full/v13/i20/2892.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i20.2892
Ampullary tumors, both benign and malignant, may present as acute recurrent pancreatitis[1]. The most common benign cause of this situation is adenoma of the major papilla[2,3]. Other benign masses of the major papilla presenting as acute recurrent pancreatitis are extremely rare[4-6]. We describe a rare case of unexposed type ampullary adenomyoma presenting as acute recurrent pancreatitis.
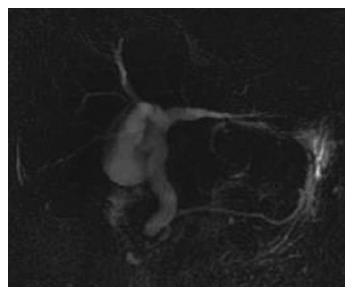
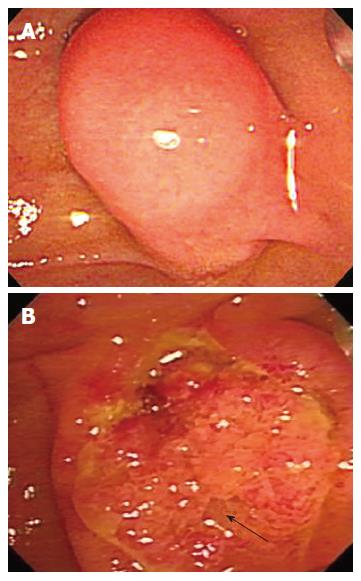
A 74-year-old woman was admitted to our department due to severe epigastric pain for one day. She denied alcohol intake and use of any drugs or medications. Five years ago, she was admitted to our hospital for similar symptoms. At the time, serum chemistry analysis revealed 37/11 U/L (0-40 U/L) aspartate/alanine aminotransferase, 85 U/L (39-117 U/L) alkaline phosphatase, 1.3 mg/dL (0.2-1.2 mg/dL) total bilirubin, 4290 IU/L (60-160 IU/L) amylase, and 1526 IU/L (0-60 IU/L) lipase. Abdominal CT scan showed acute pancreatitis and multiple peripancreatic fluid collections. For personal reasons she refused further evaluation and was discharged after receiving conservative treatment for 1 mo. During the second admission, laboratory data revealed 47/49 U/L (0-40 U/L) aspirate/alanine amino transferase, 90 U/L (39-117 U/L) alkaline phosphatase, 0.7 mg/dL (0.2-1.2 mg/dL) total bilirubin, 1417 IU/L (60-160 IU/L) amylase, and 1353 U/L (0-60 IU/L) lipase. Other laboratory results were within normal range. Abdominal CT scan showed acute pancreatitis with peripancreatic fluid collections presenting as grade E. Magnetic resonance cholangiopancreatography (MRCP) showed a diffuse dilated common bile duct without any signal void. The pancreatic duct was unremarkable (Figure 1). Because the terminal common bile duct (CBD) narrowing was suspicious, endoscopic retrograde choledochopancrea-tography (ERCP) was performed. Duodenoscopy showed the major papilla bulging into the duodenal lumen. The overlying mucosa was intact (Figure 2A).
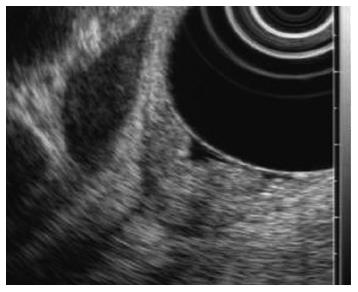
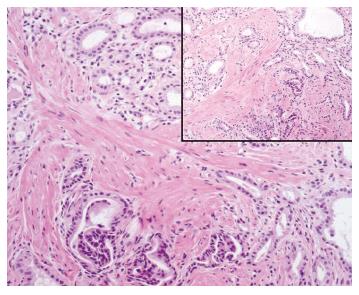
After endoscopic biliary sphincterotomy, an even and firm nodular mass with a granular and villous mucosa was seen originating from the peripancreatic orifice (Figure 2B). Multiple biopsies were taken from the mass. Though the distal common bile duct was diffusely dilated, there was no definite delay of passage after contrast injection. Subsequent endoscopic ultrasonography (EUS) showed slightly elevated echogenic lesions on the major papilla (Figure 3). There was no definite echogenic lesion in the gallbladder. Tentative pathologic diagnosis showed muscle proliferation without atypia. To confirm the diagnosis of unexposed type adenoma we performed a large-particle biopsy (piecemeal resection) using an electrocautery snare. After piecemeal resection, endoscopic pancreatic duct sphincterotomy was performed and a prophylactic pancreatic stent was inserted. Additional argon plasma coagulation (APC) was applied to obliterate remnant villous mucosa. No procedure-related complication occurred following the procedure. Histopathologic analysis of the resected specimen showed an admixture of numerous ductules and a prominent proliferation of smooth muscle in the duodenal submucosa. The ductules were lined by columnar epithelial cells (Figure 4). There were no definite pancreatic acini in the pathologic findings. Based on the pathologic findings, the diagnosis of unexposed type ampullary adenomyoma was confirmed. Follow-up duodenoscopy showed a normal looking of major papilla orifice with scar change. The patient was doing well at the 1 year follow-up.
Adenomyoma is a term generally applied to nodular lesions showing proliferation of both epithelial and smooth muscle components[7,8]. It can occur anywhere in the gastrointestinal tract. Although it is most commonly found in the fundus of the gallbladder, it rarely occurs in the extrahepatic biliary tract, including the ampulla of Vater [8].
Despite its benign nature, in previous reports, ampullary adenomyoma is usually presented as biliary obstruction[9,10]. Most cases are misdiagnosed as carcinoma or adenoma by preoperative endoscopic or radiologic procedure. Therefore, it is frequently treated with extensive surgery[8,9]. To our knowledge, this is the first reported case in English literature of adenomyoma located in the peripancreatic orifice resulting in intermittent pancreatic duct obstruction and recurrent pancreatitis diagnosed by the endoscopic piecemeal resection.
Unexposed type ampullary adenomyoma should be differentiated from chronic papillitis associated with benign conditions such as gallstones and duodenitis. Chronic papillitis may present as adenomatoid ductal hyperplasia with fibrosis and chronic inflammation[10]. In contrast, the intraampullary mass in our case showed admixture of numerous ductules and prominent proliferation of smooth muscle in the submucosa of the duodenum, which was devoid of definite fibrosis.
It may be difficult to detect small ampullary lesions, especially if they do not protrude into the ampulla[1]. Thus, endoscopic biliary sphincterotomy may be helpful in detection of the unexposed types of ampullary tumors, especially in cases of common bile duct dilatation in the absence of gallstones or in cases of unexplained recurrent pancreatitis[1,11]. On endoscopic inspection, the unexposed type ampullary adenomyoma showed lobulated, firm, villous, and mucosal granularities. These endoscopic findings are rather nonspecific and may be observed in nonneoplastic conditions such as a choledochocele, impacted ampullary stones, or papillitis[12]. Thus, endoscopic findings are by no means pathognomic, and tissue diagnosis is essential for accurate diagnosis[12]. However, tissue samples obtained using conventional biopsy forceps may have a low diagnostic yield[11]. Large-particle biopsy using an electric cautery snare has been shown to increase diagnostic accuracy as shown in previous studies[12] and the patient discussed in this report.
In summary, unexposed type ampullary adenomyoma may be added to the list of rare entities causing recurrent pancreatitis.
S- Editor Wang J L- Editor Wang XL E- Editor Ma WH
| 1. | Kim MH, Lee SK, Seo DW, Won SY, Lee SS, Min YI. Tumors of the major duodenal papilla. Gastrointest Endosc. 2001;54:609-620. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 62] [Cited by in F6Publishing: 66] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 2. | Guzzardo G, Kleinman MS, Krackov JH, Schwartz SI. Recurrent acute pancreatitis caused by ampullary villous adenoma. J Clin Gastroenterol. 1990;12:200-202. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 15] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 3. | Berk T, Friedman LS, Goldstein SD, Marks GP, Rosato FE. Relapsing acute pancreatitis as the presenting manifestation of an ampullary neoplasm in a patient with familial polyposis coli. Am J Gastroenterol. 1985;80:627-629. [PubMed] [Cited in This Article: ] |
| 4. | Usui M, Matsuda S, Suzuki H, Hirata K, Ogura Y, Shiraishi T. Somatostatinoma of the papilla of Vater with multiple gastrointestinal stromal tumors in a patient with von Recklinghausen's disease. J Gastroenterol. 2002;37:947-953. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 50] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 5. | Sriram PV, Weise C, Seitz U, Brand B, Schröder S, Soehendra N. Lymphangioma of the major duodenal papilla presenting as acute pancreatitis: treatment by endoscopic snare papillectomy. Gastrointest Endosc. 2000;51:733-736. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Mayoral W, Salcedo J, Al-Kawas F. Ampullary carcinoid tumor presenting as acute pancreatitis in a patient with von Recklinghausen's disease: case report and review of the literature. Endoscopy. 2003;35:854-857. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 24] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Ulich TR, Kollin M, Simmons GE, Wilczynski SP, Waxman K. Adenomyoma of the papilla of Vater. Arch Pathol Lab Med. 1987;111:388-390. [PubMed] [Cited in This Article: ] |
| 8. | Handra-Luca A, Terris B, Couvelard A, Bonte H, Flejou JF. Adenomyoma and adenomyomatous hyperplasia of the Vaterian system: clinical, pathological, and new immunohistochemical features of 13 cases. Mod Pathol. 2003;16:530-536. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 54] [Cited by in F6Publishing: 41] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 9. | Hammarström LE, Holmin T, Stenram U. Adenomyoma of the ampulla of Vater: an uncommon cause of bile duct obstruction. Surg Laparosc Endosc. 1997;7:388-393. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 17] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Narita T, Yokoyama M. Adenomyomatous hyperplasia of the papilla of Vater: A sequela of chronic papillitis? Ann Diagn Pathol. 1999;3:174-177. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 15] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Menzel J, Poremba C, Dietl KH, Böcker W, Domschke W. Tumors of the papilla of Vater--inadequate diagnostic impact of endoscopic forceps biopsies taken prior to and following sphincterotomy. Ann Oncol. 1999;10:1227-1231. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 70] [Cited by in F6Publishing: 77] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 12. | Venu RP, Rolny P, Geenen JE, Hogan WJ, Komorowski RA. Ampullary hamartoma: endoscopic diagnosis and treatment. Gastroenterology. 1991;100:795-798. [PubMed] [Cited in This Article: ] |