Published online Sep 14, 2006. doi: 10.3748/wjg.v12.i34.5579
Revised: May 28, 2006
Accepted: June 15, 2006
Published online: September 14, 2006
Mirizzi syndrome (MS) is an uncommon complication of gallstone disease and occurs in approximately 1% of all patients suffering from cholelithiasis. The syndrome is characterized by extrinsic compression of the common hepatic duct frequently resulting in clinical presentation of intermittent or constant jaundice. Most cases are not identified preoperatively. Surgery is the indicated treatment for patients with MS. We report here a 71-year-old male patient referred to the surgical outpatient department for diffuse upper abdominal pain and mild jaundice (bilirubin rate: 4.2 mg/dL). Ultrasound examination revealed a stone in the cystic duct compressing the common hepatic duct. The patient had a history of gastrectomy for gastric ulcer 30 years ago. MRCP revealed a stone impacted in the cystic duct causing obstruction of the common hepatic duct by extrinsic compression. With these findings the preoperative diagnosis was indicative of MS. At laparotomy a moderately shrunken gallbladder was found embedded in adhesions containing a large stone which was palpable in the common bile duct. The anterior wall of the body of the gallbladder was opened by an incision which extended longitudinally along the gallbladder towards the common bile duct. The stone measuring 3.0 cm in diameter, was then removed setting astride a large communication with the common bile duct. A Roux-en-Y cholecysto-choledocho-jejunostomy was performed. The subhepatic region was drained. The patient had an uneventful recovery. He was discharged eleven days after operation and remained well after a 30-mo follow-up.
- Citation: Safioleas M, Stamatakos M, Revenas C, Chatziconstantinou C, Safioleas C, Kostakis A. An alternative surgical approach to a difficult case of Mirizzi syndrome: A case report and review of the literature. World J Gastroenterol 2006; 12(34): 5579-5581
- URL: https://www.wjgnet.com/1007-9327/full/v12/i34/5579.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i34.5579
Mirizzi syndrome (MS) is a rare complication of long-standing cholelithiasis, which results from impaction of a large calculus or multiple small stones in the cystic duct or in the neck of the gallbladder causing extrinsic narrowing of the common hepatic duct. This condition may result in the clinical presentation of intermittent or constant jaundice. MS occurs in approximately 1% of all patients with cholelithiasis. Although modern imaging techniques are available, the majority of cases are identified during surgery. During the last two decades, 27 patients suffering from MS have been treated in our department[1,2], we present here a case of a 71-year-old male patient with MS and a literature review.
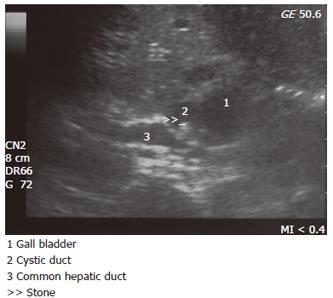
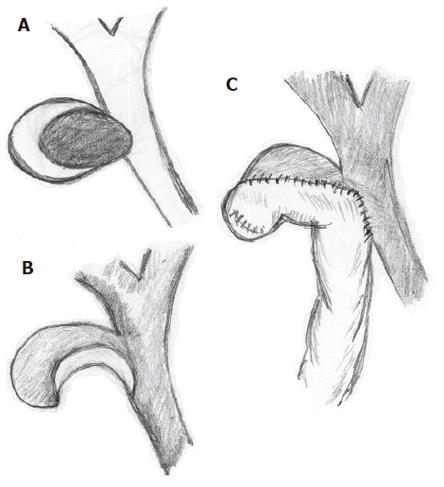
A 71-year-old male patient was referred to the surgical outpatient department for diffuse upper abdominal pain and mild jaundice (bilirubin rate: 4.2 mg/dL). Ultrasound examination revealed a stone in the cystic duct compressing the common hepatic duct (Figure 1). The patient had a history of gastrectomy for gastric ulcer 30 years ago, thus ERCP was not feasible. MRCP revealed a stone impacted in the cystic duct causing obstruction of the common hepatic duct by extrinsic compression. With these findings the preoperative diagnosis was indicative of MS. At laparotomy a moderately shrunken gallbladder was found embedded in adhesions containing a large stone which was palpable in the common bile duct (Figure 2A). It was obvious that the local operative circumstances required great surgical care. Therefore the anterior wall of the body of the gallbladder was opened by an incision which extended longitudinally along the gallbladder towards the common bile duct. The cystic duct could not be identified. The stone measuring 3.0 cm in diameter was then removed setting astride a large communication with the common bile duct (Figure 2B). Based on this finding and because the risk of stricture at the site of fistulae was significant, we decided to bypass the cholecystocholedochal fistulus defect rather than to close it directly or by using a gallbladder flap for closing the opening of the common bile duct around a T-tube. A Roux-en-Y cholecysto-choledocho-jejunostomy was performed (Figure 2C). The subhepatic region was drained. The patient had an uneventful recovery. He was discharged on the 11th postoperative day and remained well after a 30-mo follow-up.
MS was first described in 1948 as obstructive jaundice due to a gallstone impacted in the cystic duct or Hartmann’s pouch compressing the common hepatic duct[3].
McSherry et al[4] in 1982 suggested a subclassification of MS into two types. The first type concerns the external compression of the common hepatic duct by a calculus in the cystic duct or Hartmann’s pouch, whereas in the second type the stone has entered partly or completely into the common bile duct, resulting in a cholecysto-choledochal fistula. Furthermore, in 1989 a new classification of patients with MS and cholecystobiliary fistulae was presented by Csendes et al[5], which includes four types: type I lesion includes those with external compression of the common bile duct; type II lesion is a cholecystobiliary fistula present with erosion of less than one third of the circumference of the bile duct; type III lesion is a fistula involving up to two-thirds of the duct circumference; type IV lesion is a complete destruction of the bile duct.
MS and cholecystobiliary fistulae therefore appear to be different, evolving stages of the same pathological condition, thus it is reasonable that Lubbers[6] proposes that the term MS can now be abandoned, since it is only the first stage of a more complex process.
Gallstone erosion into the common duct is nevertheless a rare complication of cholelithiasis with an incidence rate ranging from 0.7% to 1.4% of all patients undergoing cholecystectomy[7].
The clinical diagnosis of MS is difficult, since there are no pathognomonic patterns of presentation. Ultrasound is diagnostically the best screening method, with ERCP and/or MRCP to confirm the diagnosis. MRCP can be as good as ERCP in the diagnosis and its ability to delineate details of biliary structures, but its disadvantage compared to ERCP is its inability to confirm the presence of fistulae and does not afford therapeutic stenting. On the other hand, T2 weighted sections can differentiate a neoplastic mass from an inflammatory one, that cannot be detected by ultrasonogram or CT scan[8]. Finally intraductal ultrasound, as an adjunct to ERCP, can also be of help[9]. Despite of all these modern diagnostic tools, the problem may become apparent only during surgery.
Surgical treatment for type I MS is partial cholecystectomy leaving the neck of the gallbladder in place[10]. In some cases, open or laparoscopic total cholecystectomy may be performed[11]. However some authors consider this a contraindication for laparoscopic cholecystectomy[12-14].
Surgical treatment of type II MS is less clearly defined. Corlette and Bismuth[15] have recommended partial cholecystectomy, oversuturing of the gallbladder cuff and insertion of a T-tube through the fistula as an adequate treatment for type II MS.
Choledochoplasty is an acceptable therapeutic approach but the amount of gallbladder tissue employed for this has not yet been standardized[16].
Furthermore, cholecystoduodenostomy has been described[17] and hepaticojejunectomy[18] can also be used if complete destruction of the common hepatic duct occurs.
Reconstruction of the extrahepatic biliary tree in case of MS type II with bypass of the lesion using a Roux-en-Y cholecysto-choledochal-jejunostomy as in our case can be carried out. To our knowledge, this is the first case described in the literature.
In conclusion, since the preoperative diagnosis of MS cannot be achieved, an awarded suspicion is necessary to avoid a lesion of the biliary tree if firm adherence around Carlot’s triangle is found. The success of treatment is related to a precocious recognition of the condition even at the time of surgery when the individual characteristics of each case are considered[18].
S- Editor Wang J L- Editor Wang XL E- Editor Bi L
| 1. | Safioleas M, Yiagos E, Doka P, Koskinas A, Stefanou J, Skalkeas Gr. Mirizzi Syndrome. Medical Annals. 1990;13:863-866. [Cited in This Article: ] |
| 2. | Safioleas M, Evagelidakis E, Xypolitas N, Liossi A. Mirizzi Syndrome. Medical Annals. 1999;12:545-547. [Cited in This Article: ] |
| 3. | Mirizzi PL. Syndrome del conducto hepatico. Journal International de Chirurgie. 1948;8:731-737. [Cited in This Article: ] |
| 4. | McSherry CK, Ferstenberg H, Virshup M. The Mirizzi syndrome: suggested classification and surgical therapy. Surg Gastroenterol. 1982;1:219-225. [Cited in This Article: ] |
| 5. | Csendes A, Díaz JC, Burdiles P, Maluenda F, Nava O. Mirizzi syndrome and cholecystobiliary fistula: a unifying classification. Br J Surg. 1989;76:1139-1143. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 216] [Cited by in F6Publishing: 230] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 6. | Lubbers EJ. Mirizzi syndrome. World J Surg. 1983;7:780-785. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 25] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Pemberton M, Wells AD. The Mirizzi syndrome. Postgrad Med J. 1997;73:487-490. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 43] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 8. | Choi BW, Kim MJ, Chung JJ, Chung JB, Yoo HS, Lee JT. Radiologic findings of Mirizzi syndrome with emphasis on MRI. Yonsei Med J. 2000;41:144-146. [PubMed] [Cited in This Article: ] |
| 9. | Phatak N, Kochman ML. Biliary endoscopy. Curr Opin Gastroenterol. 2004;20:281-287. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Abou-Saif A, Al-Kawas FH. Complications of gallstone disease: Mirizzi syndrome, cholecystocholedochal fistula, and gallstone ileus. Am J Gastroenterol. 2002;97:249-254. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 161] [Cited by in F6Publishing: 188] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 11. | Yeh CN, Jan YY, Chen MF. Laparoscopic treatment for Mirizzi syndrome. Surg Endosc. 2003;17:1573-1578. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 46] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 12. | Posta CG. Unexpected Mirizzi anatomy: a major hazard to the common bile duct during laparoscopic cholecystectomy. Surg Laparosc Endosc. 1995;5:412-414. [PubMed] [Cited in This Article: ] |
| 13. | Bagia JS, North L, Hunt DR. Mirizzi syndrome: an extra hazard for laparoscopic surgery. ANZ J Surg. 2001;71:394-397. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Tan KY, Chng HC, Chen CY, Tan SM, Poh BK, Hoe MN. Mirizzi syndrome: noteworthy aspects of a retrospective study in one centre. ANZ J Surg. 2004;74:833-837. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 35] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 15. | Corlette MB, Bismuth H. Biliobiliary fistula. A trap in the surgery of cholelithiasis. Arch Surg. 1975;110:377-383. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 56] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 16. | Shah OJ, Dar MA, Wani MA, Wani NA. Management of Mirizzi syndrome: a new surgical approach. ANZ J Surg. 2001;71:423-427. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 23] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 17. | Baer HU, Matthews JB, Schweizer WP, Gertsch P, Blumgart LH. Management of the Mirizzi syndrome and the surgical implications of cholecystcholedochal fistula. Br J Surg. 1990;77:743-745. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 87] [Cited by in F6Publishing: 91] [Article Influence: 2.7] [Reference Citation Analysis (0)] |