Published online Feb 1, 2004. doi: 10.3748/wjg.v10.i3.458
Revised: September 8, 2003
Accepted: September 11, 2003
Published online: February 1, 2004
Balantidium coli is the only parasitic ciliate of man. It is a flattened oval organism covered with cilia, and a gullet at the anterior end. It is infrequently pathogenic for man, although epidemic buds in tropical zones have been described. The infection fundamentally affects the colon and causes variable clinic pictures, from asymptomatic to serious dysenteric forms. We present a case of parasitologically diagnosed as causes of diarrhea in a patient with non-Hodgkin’s lymphoma from Turkey. In order to find out the causative etiologic agent of diarrhea, stool samples were examined by native, lugol and flotation methods and we detected moving trophozoites, which were approximately 60 μm long and 35 μm wide. These bodies were diagnosed as Balantidium coli. This case underlines that Balantidium coli should also be considered as a possible pathogen in immunocompromised patients with diarrhea.
- Citation: Yazar S, Altuntas F, Sahin I, Atambay M. Dysentery caused by Balantidium coli in a patient with non-Hodgkin’s lymphoma from Turkey. World J Gastroenterol 2004; 10(3): 458-459
- URL: https://www.wjgnet.com/1007-9327/full/v10/i3/458.htm
- DOI: https://dx.doi.org/10.3748/wjg.v10.i3.458
Balantidium coli (B.coli), the largest protozoon affecting humans, is a ciliate organism often associated with pigs. The greenish-yellow trophozoites may measure up to 120 × 150 µm and are capable of attacking the intestinal epithelium, creating ulcers and causing bloody diarrhea similar to that of amebic dysentery. It commonly infects primates, rats and pigs, and has a world-wide distribution. It is the only parasite of the family of Balantidiidae that, in rare instances, is pathogenic for humans. Balantidiasis is an infection of the large intestine by the ciliate protozoon, B. coli. In many infections (perhaps 80 percent) B. coli lives as a commensal in the lumen of the colon and causes no symptoms. A variety of gastrointestinal symptoms, including cramping, abdominal pain, nausea and foul breath, also occur. Encystment usually occurs in the intestinal lumen or stool (human or swine), and the large round cysts transmit the infection through contaminated food or water. Pigs act as carriers and are not often adversely affected by this organism[1,2].
Fortunately, balantidiasis is uncommon in temperate climates. It is found in association with pigs throughout the tropics, especially the Philippines[1]. Evidence indicates that some infected humans may become asymptomatic cyst carriers, whereas others clear the infection spontaneously. As with amebiasis, this condition probably runs the gamut between mild colitis and severe, potentially fatal dysentery. Treatment of adults and older children is usually accomplished with tetracycline, 500 mg four times daily for 20 days and metronidazole, 750 mg three times daily for five days[3].
Our study in this paper is the first reported case of balantidiasis in a patient with non-Hodgkin’s lymphoma from Turkey.
A 47 year-old female patient with non-Hodgkin’s lymphoma and complaining of diarrhea and abdominal pain was admitted to our hospital. In the patient’s history, there were watery, bad smelling, bloody diarrhea (ten times per day) and abdominal pain.
Physical examination revealed mild abdominal tenderness and increased sounds of intestine. In laboratory examination, blood routine tests were found as follows: Hb: 9.6 g/dl, Htc: 31.4%, white blood cells: 0.4 × 109/L (with 20% granulocytes and 80% lymphocytes), platelets: 56 × 109/L and sedimentation rate: 40 mm/h. Biochemical tests results were as follows: Fbg: 82 mg/dl, BUN: 40 mg/dl, creatinin: 0.7 mg/dl, total protein: 7.6 gr/dl, AST: 30 U/L, ALT: 32 U/L, ALP: 231 U/L, GGT: 43 U/L, LDH: 342 U/L, albumin: 4.1 gr/dl.
We did not obtain any abnormalities in abdominal ultrasonography and direct X-ray. There was no growth of any pathogens in stool and blood culture.
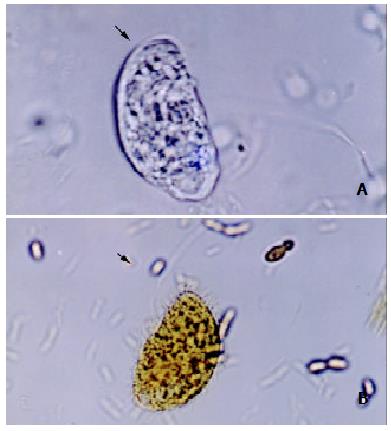
In order to find the causative etiologic agent of diarrhea, stool samples were obtained from the patient and sent to the laboratory. The stool samples were examined parasitologically by native, lugol and flotation methods. Approximately 60 µm long and 35 µm broad moving trophozoites with cilia were seen. These bodies were diagnosed as Balantidium coli (Figure 1).
Consequently, we diagnosed this organism as Balantidium coli. The patient was treated with metronidazole 750 mg three times daily for five days. Following the treatment, the symptoms rapidly and completely resolved. Re-examination of a stool sample, however, did not reveal the presence of any organism.
Balantidium coli is a protozoon and the only one ciliate that is able to cause disease in man. The trophozoite or vegetative state has oval form covered by a great amount of cilia grouped in row. In its forcebody they are peristoma and citostoma that continue with citofaringe. The later end finishes in the anal pore or citopigio. The cysts are oval or spherical, they measure from 45 to 65 µm in length[2].
Although the distribution of B.coli is cosmopolitan, infection in humans takes place by the ingestion of cysts coming from lees of the parasite guests. Of this form, different epidemic buds like the one arising in the Truk Islands after a typhoon, have taken place. That typhoon caused an extensive contamination of superficial and underground water with lees of pigs, which provided the source of water for the population[4] and led to a severe prevalence in psychiatric hospitals[5,6].Sporadic transmission was also produced by the water, contaminated vegetables crude and fecal-oral mechanism. People in contact with pigs were more likely to be infected, thus, it is said that the Aymara children of the Plateau of Bolivia had a greater prevalence of this infection, although usually they remained asymptomatic[7]. Our patient was personally questioned, she had not contacted with a pig. Probably, she might have got this parasite either via contaminated food or water. This case underlines that B. coli should also be considered as a possible pathogen in immunocompromised patients with diarrhea even if they have no contact with pigs.
Edited by Zhu LH Proofread by Wang XL
| 1. | Schmidt GD, Roberts LS. Phylum coli. Foundation of parasitology. 4th editor St. Louis: Times Mirror/ Mosby College Publication 1989; 175-180. [Cited in This Article: ] |
| 2. | González de Canales Simón P, del Olmo Martínez L, Cortejoso Hernández A, Arranz Santos T. [Colonic balantidiasis]. Gastroenterol Hepatol. 2000;23:129-131. [PubMed] [Cited in This Article: ] |
| 3. | Juckett G. Intestinal protozoa. Am Fam Physician. 1996;53:2507-2518. [PubMed] [Cited in This Article: ] |
| 4. | Walzer PD, Judson FN, Murphy KB, Healy GR, English DK, Schultz MG. Balantidiasis outbreak in Truk. Am J Trop Med Hyg. 1973;22:33-41. [PubMed] [Cited in This Article: ] |
| 5. | Giacometti A, Cirioni O, Balducci M, Drenaggi D, Quarta M, De Federicis M, Ruggeri P, Colapinto D, Ripani G, Scalise G. Epidemiologic features of intestinal parasitic infections in Italian mental institutions. Eur J Epidemiol. 1997;13:825-830. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 34] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | AREAN VM, KOPPISCH E. Balantidiasis; a review and report of cases. Am J Pathol. 1956;32:1089-1115. [PubMed] [Cited in This Article: ] |
| 7. | Esteban JG, Aguirre C, Angles R, Ash LR, Mas-Coma S. Balantidiasis in Aymara children from the northern Bolivian Altiplano. Am J Trop Med Hyg. 1998;59:922-927. [PubMed] [Cited in This Article: ] |